Intercostal, Ilioinguinal, and Iliohypogastric Nerve Transfers for Lower Limb Reinnervation After Spinal Cord Injury: an Anatomical Feasibility and Experimental Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

JMSCR Vol||06||Issue||12||Page 318-327||December 2018
JMSCR Vol||06||Issue||12||Page 318-327||December 2018 www.jmscr.igmpublication.org Impact Factor (SJIF): 6.379 Index Copernicus Value: 79.54 ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v6i12.50 Routine Ilionguinal and Iliohypogastric Nerve Excision in Lichenstein Hernia Repair - A Prospective Study of 50 Cases Authors Dr Harekrishna Majhi1, Dr Bhupesh Kumar Nayak2 1Associate Professor, Department of General Surgery, VSS IMSAR, Burla 2Senior Resident, Department of General Surgery, VSS IMSAR, Burla Email: [email protected], Contact No.: 9437137230 Abstract Chronic inguinal neuralgia is one of the most significant complications following inguinal hernia repair. Subsequent patient disability can be severe & may often require numerous interventions for treatment. The purpose of the study is to evaluate long term outcomes following nerve excision to nerve preservation when performing lichenstein inguinal hernia repairs. A prospective study of cases with excision of illionguinal & illiohypogastric nerve excision during lichenstein hernia repair with post operative groin repair at 6 month & 1 yrs from May 2015-17 was carried out in the Deptt. of General Surgery, VSSIMSAR, Burla. neuralgia reported for Lichtenstein repair of Introduction inguinal hernias range from 6% to 29%. The No disease of human body, belongs to the probable cause of chronic inguiodynia after province of the surgeon, requires its treatment, a hernioplasty due to entrapment, inflammation, better combination of accurate anatomical ligation, neuroma or fibrotic reactions involving knowledge with surgical skill than hernia in all its ilioinguinal, iliohypogastric & genitial branch of variety. This statement made by SIR Astley genito-femoral nerve. -

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

Netter's Anatomy Flash Cards – Section 7 – List 4Th Edition
Netter's Anatomy Flash Cards – Section 7 – List 4th Edition https://www.memrise.com/course/1577594/ Section 7 Lower Limb (72 cards) Plate 7-1 Hip (Coxal) Bone: Lateral View 1.1 Posterior superior iliac spine 1.2 Posterior inferior iliac spine 1.3 Greater sciatic notch 1.4 Body of ilium 1.5 Body of ischium 1.6 Ischial tuberosity 1.7 Pubic tubercle 1.8 Acetabulum 1.9 Iliac crest Plate 7-2 Hip (Coxal) Bone: Medial View 2.1 Wing (ala) of ilium (iliac fossa) 2.2 Pecten pubis (pectineal line) 2.3 Ramus of ischium 2.4 Lesser sciatic notch 2.5 Ischial spine 2.6 Articular surface (for sacrum) 2.7 Iliac tuberosity Plate 7-3 Hip Joint: Lateral View 3.1 Lunate (articular) surface of acetabulum 3.2 Articular cartilage 3.3 Head of femur 3.4 Ligament of head of femur (cut) 3.5 Obturator membrane 3.6 Acetabular labrum (fibrocartilaginous) Plate 7-4 Hip Joint: Anterior and Posterior Views 4.1 Iliofemoral ligament (Y ligament of Bigelow) 4.2 Pubofemoral ligament 4.3 Iliofemoral ligament 4.4 Ischiofemoral ligament Plate 7-5 Femur 5.1 Greater trochanter 5.2 Shaft (body) 5.3 Lateral epicondyle 5.4 Lateral condyle 5.5 Medial condyle 5.6 Medial epicondyle 5.7 Adductor tubercle 5.8 Linea aspera (Medial lip; Lateral lip) 5.9 Lesser trochanter 5.10 Intertrochanteric crest 5.11 Neck 5.12 Head Plate 7-6 Tibia and Fibula 6.1 Lateral condyle 6.2 Apex, Head, and Neck of fibula 6.3 Fibula 6.4 Lateral malleolus 6.5 Medial malleolus 6.6 Tibia 6.7 Tibial tuberosity 6.8 Medial condyle 6.9 Superior articular surfaces (medial and lateral facets) 6.10 Malleolar fossa of lateral -
33. Spinal Nerves. Cervical Plexus
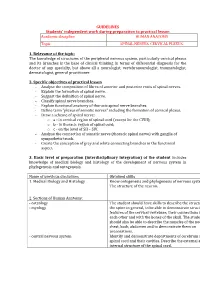
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

The Supra-Iliac Anterior Quadratus Lumborum Block
Can J Anesth/J Can Anesth https://doi.org/10.1007/s12630-019-01312-z REPORTS OF ORIGINAL INVESTIGATIONS The supra-iliac anterior quadratus lumborum block: a cadaveric study and case series Le bloc du muscle carre´ des lombes ante´rieur par approche supra-iliaque : une e´tude cadave´rique et une se´rie de cas Hesham Elsharkawy, MD, MBA, MSc . Kariem El-Boghdadly, MBBS, BSc, FRCA, EDRA, MSc . Theresa J. Barnes, MD, MPH . Richard Drake, PhD . Kamal Maheshwari, MD, MPH . Loran Mounir Soliman, MD . Jean-Louis Horn, MD . Ki Jinn Chin, MD, FRCPC Received: 9 July 2018 / Revised: 10 December 2018 / Accepted: 10 December 2018 Ó Canadian Anesthesiologists’ Society 2019 Abstract Methods Ultrasound-guided bilateral supra-iliac anterior Purpose The local anesthetic injectate spread with fascial QL blocks were performed with 30 mL of India ink dye in plane blocks and corresponding clinical outcomes may six fresh adult cadavers. Cadavers were subsequently vary depending on the site of injection. We developed and dissected to determine distribution of the dye. In five evaluated a supra-iliac approach to the anterior quadratus patients undergoing hip surgery, a unilateral supra-iliac lumborum (QL) block and hypothesized that this single anterior QL block with 25 mL ropivacaine 0.5% followed injection might successfully block the lumbar and sacral by a continuous catheter infusion was performed. Patients plexus in cadavers and provide analgesia for patients were clinically assessed daily for block efficacy. undergoing hip surgery. Results The cadaveric injections showed consistent dye involvement of the majority of the branches of the lumbar plexus, including the femoral nerve, lateral femoral cutaneous nerve, ilioinguinal nerve, and iliohypogastric Permission to use images was obtained from the Cleveland Clinic nerve. -

The Spinal Nerves That Constitute the Plexus Lumbosacrales of Porcupines (Hystrix Cristata)
Original Paper Veterinarni Medicina, 54, 2009 (4): 194–197 The spinal nerves that constitute the plexus lumbosacrales of porcupines (Hystrix cristata) A. Aydin, G. Dinc, S. Yilmaz Faculty of Veterinary Medicine, Firat University, Elazig, Turkey ABSTRACT: In this study, the spinal nerves that constitute the plexus lumbosacrales of porcupines (Hystrix cristata) were investigated. Four porcupines (two males and two females) were used in this work. Animals were appropriately dissected and the spinal nerves that constitute the plexus lumbosacrales were examined. It was found that the plexus lumbosacrales of the porcupines was formed by whole rami ventralis of L1, L2, L3, L4, S1 and a fine branch from T15 and S2. The rami ventralis of T15 and S2 were divided into two branches. The caudal branch of T15 and cranial branch of S2 contributed to the plexus lumbosacrales. At the last part of the plexus lumbosacrales, a thick branch was formed by contributions from the whole of L4 and S1, and a branch from each of L3 and S2. This root gives rise to the nerve branches which are disseminated to the posterior legs (caudal glu- teal nerve, caudal cutaneous femoral nerve, ischiadic nerve). Thus, the origins of spinal nerves that constitute the plexus lumbosacrales of porcupine differ from rodantia and other mammals. Keywords: lumbosacral plexus; nerves; posterior legs; porcupines (Hystrix cristata) List of abbreviations M = musculus, T = thoracal, L = lumbal, S = sacral, Ca = caudal The porcupine is a member of the Hystricidae fam- were opened by an incision made along the linea ily, a small group of rodentia (Karol, 1963; Weichert, alba and a dissection of the muscles. -

Study of Anatomical Pattern of Lumbar Plexus in Human (Cadaveric Study)
54 Az. J. Pharm Sci. Vol. 54, September, 2016. STUDY OF ANATOMICAL PATTERN OF LUMBAR PLEXUS IN HUMAN (CADAVERIC STUDY) BY Prof. Gamal S Desouki, prof. Maged S Alansary,dr Ahmed K Elbana and Mohammad H Mandor FROM Professor Anatomy and Embryology Faculty of Medicine - Al-Azhar University professor of anesthesia Faculty of Medicine - Al-Azhar University Anatomy and Embryology Faculty of Medicine - Al-Azhar University Department of Anatomy and Embryology Faculty of Medicine of Al-Azhar University, Cairo Abstract The lumbar plexus is situated within the substance of the posterior part of psoas major muscle. It is formed by the ventral rami of the frist three nerves and greater part of the fourth lumbar nerve with or without a contribution from the ventral ramus of last thoracic nerve. The pattern of formation of lumbar plexus is altered if the plexus is prefixed (if the third lumbar is the lowest nerve which enters the lumbar plexus) or postfixed (if there is contribution from the 5th lumbar nerve). The branches of the lumbar plexus may be injured during lumbar plexus block and certain surgical procedures, particularly in the lower abdominal region (appendectomy, inguinal hernia repair, iliac crest bone graft harvesting and gynecologic procedures through transverse incisions). Thus, a better knowledge of the regional anatomy and its variations is essential for preventing the lesions of the branches of the lumbar plexus. Key Words: Anatomical variations, Lumbar plexus. Introduction The lumbar plexus formed by the ventral rami of the upper three nerves and most of the fourth lumbar nerve with or without a contribution from the ventral ramous of last thoracic nerve. -

The Neuroanatomy of Female Pelvic Pain
Chapter 2 The Neuroanatomy of Female Pelvic Pain Frank H. Willard and Mark D. Schuenke Introduction The female pelvis is innervated through primary afferent fi bers that course in nerves related to both the somatic and autonomic nervous systems. The somatic pelvis includes the bony pelvis, its ligaments, and its surrounding skeletal muscle of the urogenital and anal triangles, whereas the visceral pelvis includes the endopelvic fascial lining of the levator ani and the organ systems that it surrounds such as the rectum, reproductive organs, and urinary bladder. Uncovering the origin of pelvic pain patterns created by the convergence of these two separate primary afferent fi ber systems – somatic and visceral – on common neuronal circuitry in the sacral and thoracolumbar spinal cord can be a very dif fi cult process. Diagnosing these blended somatovisceral pelvic pain patterns in the female is further complicated by the strong descending signals from the cerebrum and brainstem to the dorsal horn neurons that can signi fi cantly modulate the perception of pain. These descending systems are themselves signi fi cantly in fl uenced by both the physiological (such as hormonal) and psychological (such as emotional) states of the individual further distorting the intensity, quality, and localization of pain from the pelvis. The interpretation of pelvic pain patterns requires a sound knowledge of the innervation of somatic and visceral pelvic structures coupled with an understand- ing of the interactions occurring in the dorsal horn of the lower spinal cord as well as in the brainstem and forebrain. This review will examine the somatic and vis- ceral innervation of the major structures and organ systems in and around the female pelvis. -

35. Lumbar Plexus. Sacral Plexus. Coccygeal Plexus
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic LUMBAR PLEXUS. SACRAL PLEXUS. COCCYGEAL PLEXUS 1. Relevance of the topic Lumbar, sacral and coccygeal plexuses innervate the skin of the abdomen, lower back and lower extremities and all the muscles of the lower limbs. Acquired knowledge is the basis for many fields of practical medicine, such as neurology, surgery and traumatology. 2. Specific objectives After the lesson the student should know and be able to: - describe the sources of the formation of the lumbar plexus; - classify the nerves of the lumbar plexus; - to be able to demonstrate and define the branches of the lumbar plexus; - describe sources of sacral plexus formation; - classify sacral plexus nerves; - be able to demonstrate and identify short and long branches of the sacral plexus; - describe the sources of formation coccygeal plexus; - classify coccygeal plexus nerves; - be able to demonstrate and identify branches of coccygeal plexus; - to explain the innervation of muscles and skin in the areas of the lower back and lower extremity. 3. Basic level of preparation For practical this lesson a student should know and be able: - to know the anatomy of the spine, pelvis, lower extremities; - to analyze and show large and small pelvis, their bones; - to analyze and demonstrate bones and joints of the lower limbs; - to demonstrate muscles of the abdomen, perineum, pelvic girdle and lower limbs; - to know the anatomy (external and internal structure) of the spinal cord; - to know the spinal nerve anatomy. 4. Tasks for independent work during preparation for the classes 4.1. -

Posterior Approach to Kidney Dissection: an Old Surgical Approach for Integrated Medical Curricula Frank J
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of New England University of New England DUNE: DigitalUNE Biomedical Sciences Faculty Publications Biomedical Sciences Faculty Works 2-16-2015 Posterior Approach To Kidney Dissection: An Old Surgical Approach For Integrated Medical Curricula Frank J. Daly University of New England, [email protected] David L. Bolender Medical College of Wisconsin Deepali Jain Michigan State University Sheryl Uyeda SUNY Upstate Medical University Todd M. Hoagland Medical College of Wisconsin Follow this and additional works at: http://dune.une.edu/biomed_facpubs Part of the Endocrine System Commons, and the Urogenital System Commons Recommended Citation Daly, Frank J.; Bolender, David L.; Jain, Deepali; Uyeda, Sheryl; and Hoagland, Todd M., "Posterior Approach To Kidney Dissection: An Old Surgical Approach For Integrated Medical Curricula" (2015). Biomedical Sciences Faculty Publications. 6. http://dune.une.edu/biomed_facpubs/6 This Article is brought to you for free and open access by the Biomedical Sciences Faculty Works at DUNE: DigitalUNE. It has been accepted for inclusion in Biomedical Sciences Faculty Publications by an authorized administrator of DUNE: DigitalUNE. For more information, please contact [email protected]. Posterior Approach to Kidney Dissection 1 ASE-14-0094.R1 Descriptive article Posterior Approach to Kidney Dissection: An Old Surgical Approach for Integrated Medical Curricula Frank J. Daly1*, David L. Bolender2, Deepali Jain3, Sheryl Uyeda4, Todd M. Hoagland2 1Department of Biomedical Sciences, University of New England College of Osteopathic Medicine, Biddeford, Maine 2Department of Cell Biology, Neurobiology and Anatomy, Medical College of Wisconsin, Milwaukee, Wisconsin 3Department of Surgery, Grand Rapids Educational Partners, Michigan State University College of Human Medicine, Grand Rapids, Michigan. -

Cutaneous Nerve Stimulation and Motoneuronal Excitability. II: Evidence for Non-Segmental Influences
Journal of Neurology, Neurosurgery, and Psychiatry 1984;47: 190-196 Cutaneous nerve stimulation and motoneuronal excitability. II: evidence for non-segmental influences PJ DELWAIDE, P CRENNA* From the Section ofNeurology and Clinical Neurophysiology University of Liege, Liege, Belgium SUMMARY After stimulation of a sensory nerve, even distant motor nuclei undergo excitability changes which are evidenced by recovery curves. In all, two unequal peaks of facilitation can be identified. They appear when a given motor nucleus is tested after stimulation of various sensory nerves or when the same stimulation (of the sural nerve) is studied in various motor nuclei. The first facilitation is seen earlier in the masseter, then in the arm muscles and finally in lower limb muscles. The existence of a supraspinal centre activated by low threshold exteroceptive afferents and facilitating motor nuclei in a rostro-caudal sequence is postulated to account for certain features of the first and second peaks of facilitation. In an earlier publication, we' described excitability sural nerve stimulation on various motor nuclei changes in soleus and tibialis anterior motoneurons located along the length of the neuraxis: soleus, following stimulation of the sural nerve at different quadriceps, short biceps, biceps brachii and masse- intensities. A stimulus intensity which elicits tactile ter. sensation (2.5 x perception threshold) increased the amplitude of test monosynaptic soleus reflexes over Subjects and Methods two successive periods, from 55 to 90 ms (Fa) and from 130 to 170 ms (Fb). Similar results were Seventeen normal volunteers of both sexes were studied, obtained when the sural nerve contralateral to the some of them several times; they were aged between 18 test reflex was stimulated. -

Quadratus Lumborum Blocks
REGIONAL ANAESTHESIA Tutorial433 Quadratus Lumborum Blocks Ro´ isı´ n Nee†1, John McDonnell2 1Regional Fellow, Galway University Hospital, Galway, Ireland 2Consultant Anaesthetist, Galway University Hospital, Galway, Ireland Edited by: Dr. Su Cheen Ng, University College Hospital London, UK Dr. Gillian Foxall, Consultant Anaesthetist, Royal Surrey County Hospital, Guildford, UK †Corresponding author e-mail: [email protected] Published 29 September 2020 KEY POINTS Quadratus lumborum blocks (QLB) are a variation on transversus abdominis plane (TAP) blocks. Four different approaches to ultrasound-guided QLB have been described. QLB can be used to provide adjuvant analgesia for abdominal, orthopaedic, gynaecological and urological surgery. They can be performed in the lateral or supine position with a wedge under the patient’s hip. The shamrock sign of the psoas, erector spinae and the quadratus lumborum muscles around the transverse process on ultrasound allows identification of the needle insertion point. INTRODUCTION Dr. Rafa Blanco first described quadratus lumborum blocks (QLBs) in 20071 as a ‘‘no pops’’ transversus abdominis plane (TAP) block. It has been proposed as a more consistent method of accomplishing somatic as well as visceral analgesia of the abdomen than the TAP block and may provide an extended sensory blockade between T4 and L1. It can be used as an adjuvant technique for analgesia but does not provide adequate blockade to be used for anaesthesia. The QLB was developed to address the fact that as ultrasound imaging for regional anaesthesia has become more widespread, the tendency has been to move the injection point of the TAP block more anterior on the abdominal wall as compared with the original landmark technique, which is at the Triangle of Petit.