Biomechanics of the Elbow
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -
Shoulder Shoulder
SHOULDER SHOULDER ⦿ Connects arm to thorax ⦿ 3 joints ◼ Glenohumeral joint ◼ Acromioclavicular joint ◼ Sternoclavicular joint ⦿ https://www.youtube.com/watch?v=rRIz6oO A0Vs ⦿ Functional Areas ◼ scapulothoracic ◼ scapulohumeral SHOULDER MOVEMENTS ⦿ Global Shoulder ⦿ Arm (Shoulder Movement Joint) ◼ Elevation ◼ Flexion ◼ Depression ◼ Extension ◼ Abduction ◼ Abduction ◼ Adduction ◼ Adduction ◼ Medial Rotation ◼ Medial Rotation ◼ Lateral Rotation ◼ Lateral Rotation SHOULDER MOVEMENTS ⦿ Movement of shoulder can affect spine and rib cage ◼ Flexion of arm Extension of spine ◼ Extension of arm Flexion of spine ◼ Adduction of arm Ipsilateral sidebending of spine ◼ Abduction of arm Contralateral sidebending of spine ◼ Medial rotation of arm Rotation of spine ◼ Lateral rotation of arm Rotation of spine SHOULDER GIRDLE ⦿ Scapulae ⦿ Clavicles ⦿ Sternum ⦿ Provides mobile base for movement of arms CLAVICLE ⦿ Collarbone ⦿ Elongated S shaped bone ⦿ Articulates with Sternum through Manubrium ⦿ Articulates with Scapula through Acromion STERNOCLAVICULAR JOINT STERNOCLAVICULAR JOINT ⦿ Saddle Joint ◼ Between Manubrium and Clavicle ⦿ Movement ◼ Flexion - move forward ◼ Extension - move backward ◼ Elevation - move upward ◼ Depression - move downward ◼ Rotation ⦿ Usually movement happens with scapula Scapula Scapula ● Flat triangular bone ● 3 borders ○ Superior, Medial, Lateral ● 3 angles ○ Superior, Inferior, Lateral ● Processes and Spine ○ Acromion Process, Coracoid Process, Spine of Scapula ● Fossa ○ Supraspinous, Infraspinous, Subscapularis, Glenoid SCAPULA -

A STUDY of MORPHOLOGY and MORPHOMETRY of PROXIMAL END of DRY RADIUS BONES with ITS CLINICAL IMPLICATIONS Suraj Ethiraj 1, Jyothi K C *2, Shailaja Shetty 3
International Journal of Anatomy and Research, Int J Anat Res 2019, Vol 7(3.1):6712-16. ISSN 2321-4287 Original Research Article DOI: https://dx.doi.org/10.16965/ijar.2019.203 A STUDY OF MORPHOLOGY AND MORPHOMETRY OF PROXIMAL END OF DRY RADIUS BONES WITH ITS CLINICAL IMPLICATIONS Suraj Ethiraj 1, Jyothi K C *2, Shailaja Shetty 3. 1 Final year MBBS, M S Ramaiah Medical College, Bangalore, Karnataka, India. 2 Assistant Professor, Department of Anatomy, M S Ramaiah Medical College, Bangalore, Karnataka, India. 3 Professor & HOD, Department of Anatomy, M S Ramaiah Medical College, Bangalore, Karnataka, India. ABSTRACT Background: Fracture of the radial head constitute 1/3rd of all the elbow fractures. It occurs as a result of a fall on an outstretched hand or a direct blow to the lateral aspect of elbow joint. This is now becoming more common due to pre existing co-morbidities like osteoporosis and chronic osteoarthritis. Surgical correction of the comminuted fractures of radial head involves reconstruction or replacement with artificial radial head prosthesis in cases where reconstruction is not possible. Aims and Objectives: To analyze the morphometric details of proximal end of radius and to describe the morphological features of head and bicipital tuberosity of the radius. Materials & Methodology: Sixty dry human adult radius bones of unknown age and sex were assessed for morphometric and morphological characters. Vernier caliper was used to measure the various parameters on the proximal ends of radius bones. The data was tabulated and analyzed using SPSS software. Results: The mean length of radius was found to be 23.98 cm. -

Lecture 6 Comparative Anatomy of the Elbow and Forearm Functions Of
Lecture 6 Comparative anatomy of the Elbow and Forearm Functions of the Elbow in humans The set if the elbow allows for the hand to be placed in a position that makes it ideal for manipulation • Mostly non-weight supporting, and very important in throwing Bones Distal humerus- articulating parts Capitulum - Articulates with radial head - Almost half a sphere Trochlea - Like a pulleu - Articulates with trochlea notch of the ulna Distal humerus – non articulating parts Medial epicondyle - Blunt medial projection - Anterior surface has attachment for fore arm flexors Lateral epicondyle - Lateral non-articulating part - Attachment for forearm extensors on lateral part Distal humerus – fossae Olecranon fossa On posterior surface contains the olecranon of the ulna Coronoid fossa Anterior surface contains ulna coronoid process Radial fossa Shallow fossa anteriorly, contains the radius in flexion. Radius Proximal end Lateral bone in the forearm - Proximal end includes a head, neck and radial tuberosity - Head discoid and like a shallow cup, articulates with the capitulum - Neck is a constriction blew the head Distal end - Interosseous border for attachment of interosseous membrane - Styloid process sharp projection on lateral side of distal radius - Dorsal tubercle a large tuberosity on the posterior surface of the distal end. Ulna Proximal end - Olecranon hook like projection which enters the humeral olecranon fossa - Trochlea notch for articulation with the trochlea od the humerous - Coronoid process projects anteriorly distal to the olecranon - Radial notch – small oval depression on lateral side of coronoid process Distal end - Shaft sharp lateral border attachement foe Interosseous membrane - Styloid process on the distal end - Radial articulation distal rounded articulation that conforms to the ulna notch of the radius. -

Arm and Cubital Fossa
Two Minute History M1 - Anatomy Dissection: • 300 B.C Arm and Cubital Alexandrian Egypt: King Ptolemy I, its ok Fossa to dissect cadavers of executed, mummies etc… •Herophilus “Father of Anatomy” accused by a rival of DG Simpson, Ph.D. dissecting 600 criminals…..live criminals VCU Department of Anatomy •1300 AD Europe Pope Boniface VIII edict to stop dissection to reduce the flow of bodies “parted out and boiled” from the crusades. Unclear if this is broad ban or very narrow. 1 2 Dissection: Dissection: •1540 parliament passes “The United Company of Barbers and •1700’s with the expansion of medical Surgeons, dissect 4-6 executed schools cadavers are used as tuition criminals/yr (not enough even then) •Competition is very high and medical •1600’s Britain. The executed are schools actively advertise that training includes dissections etc.. dissected in public as punishment • 1628 William Harvey •1828 London had 10 full time (cardiovascular fame). Autopsy & 200 part time body snatchers (“seasonal work” at 312 bodies/yr) of live and dead…. Medicine expands and shortages develop •Inventions to foil grave robbers Harvey dissects father and sister •1828 Robert Knox….and the rest • 1740’s Lots of private medical is amazing history. schools competing for students, William Hogarth The Reward of Cruelty 3 4 market forces develop 1750-1751 Dissection: •Burke was hanged: 25,000 watched. Hare was granted immunity as crowd called “Burke Hare” •1828, knock on the •Burke dissected: 30,000 came to see the open lab door, Knox’s assistant purchases a cadaver -

The Ulna Humerus and Ulna: Landmarks and Articulations
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. The Ulna o the ulna is a medial long bone, the longer of the two in the forearm. Proximally, it articulates with the capitulum and trochlea of the humerus; . At the radial notch, it articulates with the head of radius o It stabilizes the forearm o The HEAD LIES DISTALLY. The Olecranon The Trochlear Notch The Coronoid Process The Radial Notch where the head of the radius goes The Tuberosity of the Ulna is where the Brachialis attaches The deep part of Supinator fossa the supinator Supinator crest attaches here Bony features include: - Olecranon - Trochlear notch - Coronoid process - Radial notch - Tuberosity of ulna - Supinator fosa - Supinator crest - Head of ulna - Ulnar styloid process The head of ulna The ulnar styloid process Humerus and ulna: landmarks and articulations o the humerus is a long bone, the largest in the upper limb o it articulates proximally with the scapula at the scapulohumeral (glenohumeral) joint o it articulates distally with the ulna at the elbow joint o the ulna and humerus articulate at the elbow joint o the articulations include: . articulation between the trochlea of the humerus and the trochlear notch of the ulna . articulation of the olecranon process and the olecranon fossa during extension . articulation of the coronoid process and the coronoid fossa during flexion o the surface landmarks include . the medial and lateral epicondyle . the olecranon . the posterior border of the ulna . -
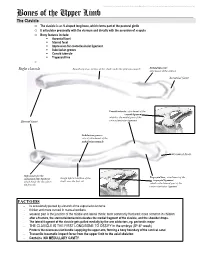
Bones of the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Bones of the Upper Limb The Clavicle o The clavicle is an S-shaped long bone, which forms part of the pectoral girdle o It articulates proximally with the sternum and distally with the acromion of scapula o Bony features include: . Acromial facet . Sternal facet . Impression for costoclavicular ligament . Subclavian groove . Conoid tubercle . Trapezoid line o Right clavicle Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: attachment of the deltoid Acromial facet Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Subclavian groove: site of attachment of the subclavius muscle Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Rough inferior surface of the trapezoid ligament which binds the clavicle to shaft, over the first rib which is the lateral part of the the first rib coracoclavicular ligament FACTOIDS - Its occasionally pierced by a branch of the supraclavicular nerve - thicker and more curved in manual workers - weakest part is the junction of the middle and lateral thirds: most commonly fractured; more common in children - after a fracture, the sternocleidomastoid elevates the medial fragment of the clavicle, and the shoulder drops. - The lateral fragment of the clavicle gets pulled medially by the arm adductors, eg. pectoralis major - THE CLAVICLE IS THE FIRST LONG BONE TO OSSIFY in the embryo (5th-6th week) - Protects the neurovascular bundle supplying the upper arm, forming a bony boundary of the cervical canal - Transmits traumatic impact force from the upper limb to the axial skeleton - Contains NO MEDULLARY CAVITY - This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. -

Radial Head Dislocation and Subluxation in Osteogenesis Imperfecta
2694 COPYRIGHT Ó 2007 BY THE JOURNAL OF BONE AND JOINT SURGERY,INCORPORATED Radial Head Dislocation and Subluxation in Osteogenesis Imperfecta By Alice Marcdargent Fassier, MD, Frank Rauch, MD, Mehdi Aarabi, MD, Chantal Janelle, MD, FRCS, and Francxois Fassier, MD, FRCS Investigation performed at Shriners Hospital, Montreal, Quebec, Canada Background: Upper limb deformity in children with osteogenesis imperfecta may substantially impair function. The aims of this retrospective work were to study the prevalence of radial head malalignment (dislocation or subluxation) in different types of osteogenesis imperfecta and to identify factors linked to it. Methods: We assessed 489 upper limbs from 254 patients (with a mean age of 9.6 years and including 130 female patients) who had various types of osteogenesis imperfecta. Radiographs representing a single time-point for each patient were assessed for the presence and direction of radial head malalignment and associated abnormalities (dysplasia of the capitellum or of the radial head or neck, calcification of the interosseous mem- brane, or radioulnar synostosis). Deformations of the humerus, radius, and ulna were assessed with regard to location, direction, and magnitude. The forearm range of motion in pronation and supination and the hand grip force were measured in a subset of patients. Results: We observed radial head dislocation or subluxation in forty-four and thirty-nine upper extremities, respec- tively. The frequency of radial head malalignment was significantly higher in type-V osteogenesis imperfecta (86%) than in the other types (0% to 29%) (p < 0.001). Dysplasia of the humeral capitellum, radial head, or radial neck was associated with malalignment in all types of osteogenesis imperfecta, with the exception of capitellum dys- plasia in type V. -
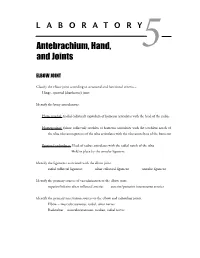
Antebrachium, Hand, and Joints
LABORATORY Antebrachium, Hand, 5 and Joints ELBOW JOINT Classify the elbow joint according to structural and functional criteria – Hinge, synovial (diarthrotic) joint Identify the bony articulations. Humeroradial: (radial collateral) capitulum of humerus articulates with the head of the radius Humeroulnar: (ulnar collateral) trochlea of humerus articulates with the trochlear notch of the ulna olecranon process of the ulna articulates with the olecranon fossa of the humerus Proximal radioulnar: Head of radius articulates with the radial notch of the ulna Held in place by the annular ligament Identify the ligaments associated with the elbow joint. radial collateral ligament ulnar collateral ligament annular ligament Identify the primary sources of vascularization to the elbow joint. superior/inferior ulnar collateral arteries anterior/posterior interosseous arteries Identify the primary innervation sources to the elbow and radioulnar joints. Elbow – musculocutaneous, radial, ulnar nerves Radioulnar – musculocutaneous, median, radial nerves 28 Laboratory 5 • Antebrachium, Hand, and Joints Identify the structures associated with the cubital fossa. brachial artery median nerve median cubital vein biceps brachii tendon Discuss the venous return from the brachial region. cephalic vein basilic vein median cubital vein axillary vein RADIOULNAR JOINTS Proximal radioulnar: Head of radius articulates with the radial notch of the ulna Distal radioulnar: Head of the ulna articulates with the ulnar notch on the radius Allows radius to move anteriorly across the ulna during pronation Classify the radioulnar joints according to structural and functional criteria, and identify the associated ligaments. Proximal – pivot, synovial diarthrotic joint Distal – pivot, synovial diarthrotic joint annular ligament triangular ligament (articular disc) radial/ulnar collateral ligaments (fibrocartilage complex) radial/ulnar collateral ligaments WRIST JOINT Classify the wrist joint according to structural and functional criteria – diarthrotic, synovial condyloid. -
Plane Scapula / Humerus Synovial; Ball
JOINTS OF THE APPENDICULAR SKELETON UPPER LIMB Joint Articulating Bones Structural Type Acromioclavicular Scapula / Clavicle Synovial; plane Synovial; Shoulder (Glenohumeral) Scapula / Humerus ball-and-socket Elbow Ulna / Humerus Synovial; hinge Proximal radioulnar Radius / Ulna Synovial; pivot Distal radioulnar Radius / Ulna Synovial; pivot Radius / Wrist Synovial; condylar Proximal carpals Intercarpal Adjacent carpals Synovial; plane Trapezium / Thumb (Carpometacarpal ) Synovial; saddle Metacarpal 1 Carpometacarpal Carpal / Metacarpal Synovial; plane Knuckle Metacarpal / Synovial; condylar (Metacarpophalangeal) Proximal phalanx Finger (Interphalangeal) Adjacent phanges Synovial; hinge Upper Limb – Selected Joints (Marieb / Hoehn – Chapter 8; Pgs. 262 – 269) A. Shoulder Joint: The shoulder joint is a ball-and-socket type synovial joint (Figure 1). The very shallow glenoid cavity of the scapula and the large humeral head endow the shoulder joint with the greatest degree of mobility of any joint in the body. However, this increase in freedom of movement comes at the expense of stability; should dislocations are a fairly common injury, especially in the forward and downward direction. Figure 1: Right shoulder joint, anterior and lateral views (note: acromioclavicular and coracoclavicular ligaments not shown) Fibrocartilage: Glenoid labrum: Rim of fibrocartilage on margin of glenoid cavity; slightly deepens articulation point of scapula with humerus. Ligaments: Coracohumeral ligament: Attaches the base of the coracoid process of the scapula to the greater tubercle of the humerus; helps support weight of the upper limb. Glenohumeral ligaments: Three layered ligaments (superior, middle, inferior) located on the anterior aspect of the joint; offer weak support to the joint and may be partially absent in some individuals. Coracoacromial ligament: Attaches the coracoid process of the scapula to the acromion of the scapula; reinforces scapular structure. -

Bones, Part 1: the Appendicular Skeleton
PowerPoint® Lecture Slides The Appendicular Skeleton prepared by Leslie Hendon University of Alabama, Birmingham • Pectoral girdle • Attaches the upper limbs to the trunk Pelvic girdle C H A P T E R • 8 • Attaches the lower limbs to the trunk Part 1 • Upper and lower limbs differ in function Bones, • Share the same structural plan Part 1: The Appendicular Skeleton Copyright © 2011 Pearson Education, Inc. Copyright © 2011 Pearson Education, Inc. The Pectoral Girdle The Pectoral Girdle • Consists of the clavicle and the scapula • Provides attachment for many muscles that • Pectoral girdles do not quite encircle the move the upper limb body completely • Girdle is very light and upper limbs are • Medial end of each clavicle articulates with mobile the manubrium and first rib • Only clavicle articulates with the axial skeleton • Laterally—the ends of the clavicles join the • Socket of the shoulder joint (glenoid cavity) is scapulae shallow • Scapulae do not join each other or the axial • Good for flexibility, bad for stability skeleton Copyright © 2011 Pearson Education, Inc. Copyright © 2011 Pearson Education, Inc. Articulated Pectoral Girdle Clavicles Sternal (medial) Clavicle end Acromio- clavicular Scapula Posterior joint Anterior Acromial (lateral) end (b) Right clavicle, superior view Acromial end Anterior Trapezoid line Sternal end Posterior Tuberosity for PLAY Shoulder Conoid tubercle costoclavicular ligament (a) Articulated pectoral girdle (c) Right clavicle, inferior view Copyright © 2011 Pearson Education, Inc. Figure 8.1a Copyright © 2011 Pearson Education, Inc. Figure 8.1b, c 1 Scapulae Structures of the Scapula Acromion Suprascapular notch Superior border • Lie on the dorsal surface of the rib cage Coracoid Superior process angle • Located between ribs 2–7 Glenoid cavity • Have three borders • Superior • Medial (vertebral) • Lateral (axillary) Subscapular Lateral border fossa • Have three angles Medial border • Lateral, superior, and inferior (a) Right scapula, anterior aspect Inferior angle Copyright © 2011 Pearson Education, Inc. -

Upper Limb Syllabus
UPPER LIMB COURSE CONTENT COMPETENCIES The first year medical student should be able to understand and describe the gross anatomy of the various regions, bones, joints, muscles, vessels and nerves of upper limb, demonstrate the actions of the muscle groups at various joints, correlate the anatomical basis of clinical manifestations of nerve injuries and fractures of upper limb and demonstrate the radiological anatomy of upper limb. REGIONS Mammary gland; Axilla; Cubital fossa; Fascial spaces of the hand Definition, location, boundaries, contents (major), venepuncture Level 2: Details with relations and functional importance of individual structures Fascial spaces – forearm space, radial bursa, ulnar bursa, palmar spaces Dupuytren’s contracture Hand as a functional unit - grips Nerve injury, carpal tunnel syndrome Level 3: Applied aspects: Axilla – Collaterals, lymph nodes (breast), axillary sheath (cervico-axillary canal), abscess drainage Palm – Comparative anatomy (thumb, palmaris brevis), position of rest and of function, collaterals Fascial spaces – Surgical significance OSTEOLOGY Identification, region, anatomical position, parts, joints formed, development; (For carpals, identification of individual carpals in an articulated hand) Level 2: Description, attachments, relations; clavipectoral fascia; boundaries of anatomical snuff-box; salient features about carpals Level 3: Applied aspects: Clavicle – Line of force transmission, commonest site of fracture Scapula – Fracture scapula Humerus – Supracondylar spur, angle of humeral torsion,