Hematology D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Exploring the Potential of the Platelet Membrane Proteome As a Source Of
Donovan et al. Alzheimer’s Research & Therapy 2013, 5:32 http://alzres.com/content/5/3/32 RESEARCH Open Access Exploring the potential of the platelet membrane proteome as a source of peripheral biomarkers for Alzheimer’s disease Laura E Donovan1†, Eric B Dammer2†, Duc M Duong3, John J Hanfelt4, Allan I Levey1, Nicholas T Seyfried1,3* and James J Lah1* Abstract Introduction: Peripheral biomarkers to diagnose Alzheimer’s disease (AD) have not been established. Given parallels between neuron and platelet biology, we hypothesized platelet membrane-associated protein changes may differentiate patients clinically defined with probable AD from noncognitive impaired controls. Methods: Purified platelets, confirmed by flow cytometry were obtained from individuals before fractionation by ultracentrifugation. Following a comparison of individual membrane fractions by SDS-PAGE for general proteome uniformity, equal protein weight from the membrane fractions for five representative samples from AD and five samples from controls were pooled. AD and control protein pools were further divided into molecular weight regions by one-dimensional SDS-PAGE, prior to digestion in gel. Tryptic peptides were analyzed by reverse-phase liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS). Ionized peptide intensities were averaged for each identified protein in the two pools, thereby measuring relative protein abundance between the two membrane protein pools. Log2-transformed ratio (AD/control) of protein abundances fit a normal distribution, thereby permitting determination of significantly changed protein abundances in the AD pool. Results: We report a comparative analysis of the membrane-enriched platelet proteome between patients with mild to moderate AD and cognitively normal, healthy subjects. -

Phenotypic and Molecular Genetic Analysis of Pyruvate Kinase Deficiency in a Tunisian Family
The Egyptian Journal of Medical Human Genetics (2016) 17, 265–270 HOSTED BY Ain Shams University The Egyptian Journal of Medical Human Genetics www.ejmhg.eg.net www.sciencedirect.com ORIGINAL ARTICLE Phenotypic and molecular genetic analysis of Pyruvate Kinase deficiency in a Tunisian family Jaouani Mouna a,1,*, Hamdi Nadia a,1, Chaouch Leila a, Kalai Miniar a, Mellouli Fethi b, Darragi Imen a, Boudriga Imen a, Chaouachi Dorra a, Bejaoui Mohamed b, Abbes Salem a a Laboratory of Molecular and Cellular Hematology, Pasteur Institute, Tunis, Tunisia b Service d’Immuno-He´matologie Pe´diatrique, Centre National de Greffe de Moelle Osseuse, Tunis, Tunisia Received 9 July 2015; accepted 6 September 2015 Available online 26 September 2015 KEYWORDS Abstract Pyruvate Kinase (PK) deficiency is the most frequent red cell enzymatic defect responsi- Pyruvate Kinase deficiency; ble for hereditary non-spherocytic hemolytic anemia. The disease has been studied in several ethnic Phenotypic and molecular groups. However, it is yet an unknown pathology in Tunisia. We report here, the phenotypic and investigation; molecular investigation of PK deficiency in a Tunisian family. Hemolytic anemia; This study was carried out on two Tunisian brothers and members of their family. Hematolog- Hydrops fetalis; ical, biochemical analysis and erythrocyte PK activity were performed. The molecular characteriza- PKLR mutation tion was carried out by gene sequencing technique. The first patient died few hours after birth by hydrops fetalis, the second one presented with neonatal jaundice and severe anemia necessitating urgent blood transfusion. This severe clinical pic- ture is the result of a homozygous mutation of PKLR gene at exon 8 (c.1079G>A; p.Cys360Tyr). -

Immunoglobulin G Is a Platelet Alpha Granule-Secreted Protein
Immunoglobulin G is a platelet alpha granule-secreted protein. J N George, … , L K Knieriem, D F Bainton J Clin Invest. 1985;76(5):2020-2025. https://doi.org/10.1172/JCI112203. Research Article It has been known for 27 yr that blood platelets contain IgG, yet its subcellular location and significance have never been clearly determined. In these studies, the location of IgG within human platelets was investigated by immunocytochemical techniques and by the response of platelet IgG to agents that cause platelet secretion. Using frozen thin-sections of platelets and an immunogold probe, IgG was located within the alpha-granules. Thrombin stimulation caused parallel secretion of platelet IgG and two known alpha-granule proteins, platelet factor 4 and beta-thromboglobulin, beginning at 0.02 U/ml and reaching 100% at 0.5 U/ml. Thrombin-induced secretion of all three proteins was inhibited by prostaglandin E1 and dibutyryl-cyclic AMP. Calcium ionophore A23187 also caused parallel secretion of all three proteins, whereas ADP caused virtually no secretion of any of the three. From these data and a review of the literature, we hypothesize that plasma IgG is taken up by megakaryocytes and delivered to the alpha-granules, where it is stored for later secretion by mature platelets. Find the latest version: https://jci.me/112203/pdf Rapid Publication Immunoglobulin G Is a Platelet Alpha Granule-secreted Protein James N. George, Sherry Saucerman, Shirley P. Levine, and Linda K. Knieriem Division ofHematology, Department ofMedicine, University of Texas Health Science Center, and Audie L. Murphy Veterans Hospital, San Antonio, Texas 78284 Dorothy F. -

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

Non-Commercial Use Only
only use Non-commercial 14th International Conference on Thalassaemia and Other Haemoglobinopathies 16th TIF Conference for Patients and Parents 17-19 November 2017 • Grand Hotel Palace, Thessaloniki, Greece only use For thalassemia patients with chronic transfusional iron overload... Make a lasting impression with EXJADENon-commercial film-coated tablets The efficacy of deferasirox in a convenient once-daily film-coated tablet Please see your local Novartis representative for Full Product Information Reference: EXJADE® film-coated tablets [EU Summary of Product Characteristics]. Novartis; August 2017. Important note: Before prescribing, consult full prescribing information. iron after having achieved a satisfactory body iron level and therefore retreatment cannot be recommended. ♦ Maximum daily dose is 14 mg/kg body weight. ♦ In pediatric patients the Presentation: Dispersible tablets containing 125 mg, 250 mg or 500 mg of deferasirox. dosing should not exceed 7 mg/kg; closer monitoring of LIC and serum ferritin is essential Film-coated tablets containing 90 mg, 180 mg or 360 mg of deferasirox. to avoid overchelation; in addition to monthly serum ferritin assessments, LIC should be Indications: For the treatment of chronic iron overload due to frequent blood transfusions monitored every 3 months when serum ferritin is ≤800 micrograms/l. (≥7 ml/kg/month of packed red blood cells) in patients with beta-thalassemia major aged Dosage: Special population ♦ In moderate hepatic impairment (Child-Pugh B) dose should 6 years and older. ♦ Also indicated for the treatment of chronic iron overload due to blood not exceed 50% of the normal dose. Should not be used in severe hepatic impairment transfusions when deferoxamine therapy is contraindicated or inadequate in the following (Child-Pugh C). -

Point-Of-Care Testing for Anticoagulation Monitoring In
Point-of-Care Testing for Anticoagulation PATIENT SAFETY Monitoring in Neuroendovascular Procedures H.M. Hussein SUMMARY: POC testing is defined as diagnostic testing at or near the site of patient care. Rapid A.L. Georgiadis measurement of the intensity of anticoagulation and, more recently, platelet inhibition allows dose titration of adjuvant medications such a heparin and antiplatelet agents during neuroendovascular A.I. Qureshi procedures. However, knowledge among practicing physicians regarding the pathophysiologic basis of these measurements and variations in knowledge about the differences among devices is often limited. This review discusses the role of anticoagulation in endovascular procedures and the currently available POC tests for anticoagulation monitoring. ABBREVIATIONS: ACT ϭ activated clotting time; Anti-Xa ϭ quantitative chromogenic heparin assay; aPTT ϭ activated partial thromboplastin time; AT ϭ antithrombin; CI ϭ confidence interval; GP IIb/IIIa ϭ glycoprotein IIb/IIIa; Hemonox-CT ϭ Hemonox clotting time; HIT ϭ heparin-induced thrombocytopenia; HMT ϭ Heparin Management Test; IV ϭ intravenous; LMWH ϭ low-molecular- weight heparin; MI ϭ myocardial infarction; OR ϭ odds ratio; PCI ϭ percutaneous coronary intervention; POC ϭ point of care; UFH ϭ unfractionated heparin hromboembolism ensues from activation of platelets and Brief Overview of Anticoagulant Medications Tthe coagulation cascade and is a major source of compli- Anticoagulants reduce the activity of proteases in the coagula- cations during endovascular procedures. Multiple studies tion cascade. On the basis of their mechanism of action (Fig 1), have demonstrated accelerated platelet activation during cor- anticoagulants can be divided into 4 major groups: vitamin K onary and cerebral angioplasty.1,2 The coagulation cascade antagonists (warfarin), heparins (UFH and LMWH), direct (Fig 1) consists of a sequential conversion of a series of proen- thrombin inhibitors, and direct factor Xa inhibitors. -

Alterations in Platelet Alpha-Granule Secretion and Adhesion on Collagen Under Flow in Mice Lacking the Atypical Rho Gtpase Rhobtb3
cells Article Alterations in Platelet Alpha-Granule Secretion and Adhesion on Collagen under Flow in Mice Lacking the Atypical Rho GTPase RhoBTB3 Martin Berger 1,2, David R. J. Riley 1, Julia Lutz 1, Jawad S. Khalil 1, Ahmed Aburima 1, Khalid M. Naseem 3 and Francisco Rivero 1,* 1 Centre for Atherothrombosis and Metabolic Disease, Hull York Medical School, Faculty of Health Sciences, University of Hull, HU6 7RX Hull, UK; [email protected] (M.B.); [email protected] (D.R.J.R.); [email protected] (J.L.); [email protected] (J.S.K.); [email protected] (A.A.) 2 Department of Internal Medicine 1, University Hospital, RWTH Aachen, 52074 Aachen, Germany 3 Leeds Institute for Cardiovascular and Metabolic Medicine, University of Leeds, LS2 9NL Leeds, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-1482-466433 Received: 8 January 2019; Accepted: 7 February 2019; Published: 11 February 2019 Abstract: Typical Rho GTPases, such as Rac1, Cdc42, and RhoA, act as molecular switches regulating various aspects of platelet cytoskeleton reorganization. The loss of these enzymes results in reduced platelet functionality. Atypical Rho GTPases of the RhoBTB subfamily are characterized by divergent domain architecture. One family member, RhoBTB3, is expressed in platelets, but its function is unclear. In the present study we examined the role of RhoBTB3 in platelet function using a knockout mouse model. We found the platelet count, size, numbers of both alpha and dense granules, and surface receptor profile in these mice were comparable to wild-type mice. -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -
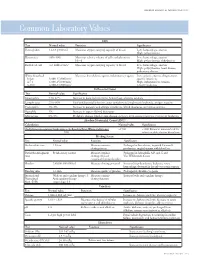
Common Laboratory Values
AmericAn AcAdemy of PediAtric dentistry Reference Manual 2006-2007 Resource Section 251 Common LaboratoryCommon Values Laboratory Values CBC Test Normal value Function Significance Hemoglobin 12-18 g/100 mL Measures oxygen carrying capacity of blood Low: hemorrhage, anemia High: polycythemia Hematocrit 35%-50% Measures relative volume of cells and plasma in Low: hemorrhage, anemia blood High: polycythemia, dehydration Red blood cell 4-6 million/mm3 Measures oxygen-carrying capacity of blood Low: hemorrhage, anemia High: polycythemia, heart disease, pulmonary disease White blood cell Measures host defense against inflammatory agents Low: aplastic anemia, drug toxicity, Infant 8,000-15,000/mm3 specific infections 4-7 y 6,000-15,000/mm3 High: inflammation, trauma, 8-18 y 4,500-13,500/mm3 toxicity, leukemia Differential Count Test Normal value Significance Neutrophils 54%-62% Increase in bacterial infections, hemorrhage, diabetic acidosis Lymphocytes 25%-30% Viral and bacterial infection, acute and chronic lymphocytic leukemia, antigen reaction Eosinophils 1%-3% Increase in parasitic and allergic conditions, blood dyscrasias, pernicious anemia Basophils 1% Increase in types of blood dyscrasias Monocytes 0%-9% Hodgkin’s disease, lipid storage disease, recovery from severe infections, monocytic leukemia Absolute Neutrophil Count (ANC) Calculation Normal value Significance (% Polymorphonuclear Leukocytes + % Bands)×Total White Cell Count >1500 <1000 Patient at increased risk for 100 infection; defer elective dental care Bleeding Screen Test -

224 Subpart H—Hematology Kits and Packages
§ 864.7040 21 CFR Ch. I (4–1–02 Edition) Subpart H—Hematology Kits and the treatment of venous thrombosis or Packages pulmonary embolism by measuring the coagulation time of whole blood. § 864.7040 Adenosine triphosphate re- (b) Classification. Class II (perform- lease assay. ance standards). (a) Identification. An adenosine [45 FR 60611, Sept. 12, 1980] triphosphate release assay is a device that measures the release of adenosine § 864.7250 Erythropoietin assay. triphosphate (ATP) from platelets fol- (a) Identification. A erythropoietin lowing aggregation. This measurement assay is a device that measures the is made on platelet-rich plasma using a concentration of erythropoietin (an en- photometer and a luminescent firefly zyme that regulates the production of extract. Simultaneous measurements red blood cells) in serum or urine. This of platelet aggregation and ATP re- assay provides diagnostic information lease are used to evaluate platelet for the evaluation of erythrocytosis function disorders. (increased total red cell mass) and ane- (b) Classification. Class I (general mia. controls). (b) Classification. Class II. The special [45 FR 60609, Sept. 12, 1980] control for this device is FDA’s ‘‘Docu- ment for Special Controls for Erythro- § 864.7060 Antithrombin III assay. poietin Assay Premarket Notification (a) Identification. An antithrombin III (510(k)s).’’ assay is a device that is used to deter- [45 FR 60612, Sept. 12, 1980, as amended at 52 mine the plasma level of antithrombin FR 17733, May 11, 1987; 65 FR 17144, Mar. 31, III (a substance which acts with the 2000] anticoagulant heparin to prevent co- agulation). This determination is used § 864.7275 Euglobulin lysis time tests. -

• Cytosis: O Neutrophilia: Defined As an Increase in the Neutrophilic Count in the Peripheral Blood Above Reference Range for Age
HENATOLYMPHOID SYSTEM THIRD YEAR MEDICAL STUDENTS-UNIVERSITY OF JORDAN AHMAD T. MANSOUR, MD NONNEOPLASTIC DISEASES OF THE WHITE BLOOD CELLS • There are five major types of WBCs in the blood: neutrophils, lymphocytes, eosinophils, basophils and monocytes. • The normal function of the white blood cells depends on a tight regulation of their count and their function. Therefore, disease develops if there is a derangement of the cells count or function, it takes one of the following forms: o Cytosis: increase in the number of circulating cells above reference range. (Note: leukocytosis means an increase in the WBC count, neutrophilia means increase in the neutrophilic count, lymphocytosis means increase in the lymphocytic count, monocytosis means increase in the monocytic count, basophilia means increase in the basophilic count and eosinophilia means in crease in the eosinophilic count). o Cytopenia: decrease in the number of circulating cells below reference range. (Note: neutropenia means decreased neutrophils, lymphocytopenia, or simply lymphopenia, means decrease in lymphocytes, monocytopenia means decrease in monocytes, eosinopenia means decrease in eosinophils, and basopenia means decrease in basophils). o Abnormal or absent function • Cytosis: o Neutrophilia: defined as an increase in the neutrophilic count in the peripheral blood above reference range for age. o Causes: bacterial infection is the most common and most important etiology. Tissue necrosis in cases of burns or trauma and medications such as epinephrine and corticosteroids are also additional causes for neutrophilia. § Some physiologic conditions can lead to neutrophilia such as stress, smoking and pregnancy. o Pathophysiology: neutrophils are present in the blood in two populations: circulating and marginal (meaning neutrophils stuck to the vessel wall). -

Study of Osmotic Fragility Status of Red Blood Cell in Type II Diabetes Mellitus Patients
European Journal of Environment and Public Health, 2017, 1(2), 06 ISSN: 2468-1997 Study of Osmotic Fragility Status of Red Blood Cell in Type II Diabetes Mellitus Patients Nihad Rownak1, Shahin Akhter2, Monira Khatun3, Sohel Baksh4, Shafquat Rafiq5*, Mushfiqur Rahman6 1 Department of Physiology, University of Science & Technology Chittagong, BANGLADESH 2 Department of Physiology, Chittagong Medical College, Chittagong, BANGLADESH 3 Department of Physiology, Chattagram Maa O Shishu Hospital Medical College, Chittagong, BANGLADESH 4 Department of Physiology, Cox’s Bazar Medical College, BANGLADESH 5 Croydon University Hospital NHS Trust, UNITED KINGDOM 6 Department of Pediatric Surgery, Chittagong Medical College, Chittagong, BANGLADESH *Corresponding Author: [email protected] Citation: Rownak, N., Akhter, S., Khatun, M., Baksh, S., Rafiq, S., and Rahman, M. (2017). Study of Osmotic Fragility Status of Red Blood Cell in Type II Diabetes Mellitus Patients. European Journal of Environment and Public Health, 1(2), 06. https://doi.org/10.20897/ejeph/77094 Published: December 28, 2017 ABSTRACT Diabetes Mellitus (DM) is one of the most prevalent non-communicable diseases in the world. Cell membrane injury is an important mechanism for pathophysoilogical changes in DM. Osmotic fragility (OF) status of Red blood cell (RBC) in hyperglycemic patients is expected to be increased. This study was conducted in Chittagong medical college hospital and Chittagong Diabetic Hospital from January 2015 to December 2015. 100 newly diagnosed (duration ≤ 3 years) type II diabetes mellitus patients (Fasting blood glucose is ≥7 mmol/L) were selected as cases. Age, sex and BMI matched 100 healthy subjects were included as control. OF of RBC was measured by traditional method with a series of hypotonic solution of NaCl of different strength in twelve test tubes numbered serially.