Updated Network Meta-Analysis of First-Line EGFR
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Combining Biomarkers for Immunotherapy
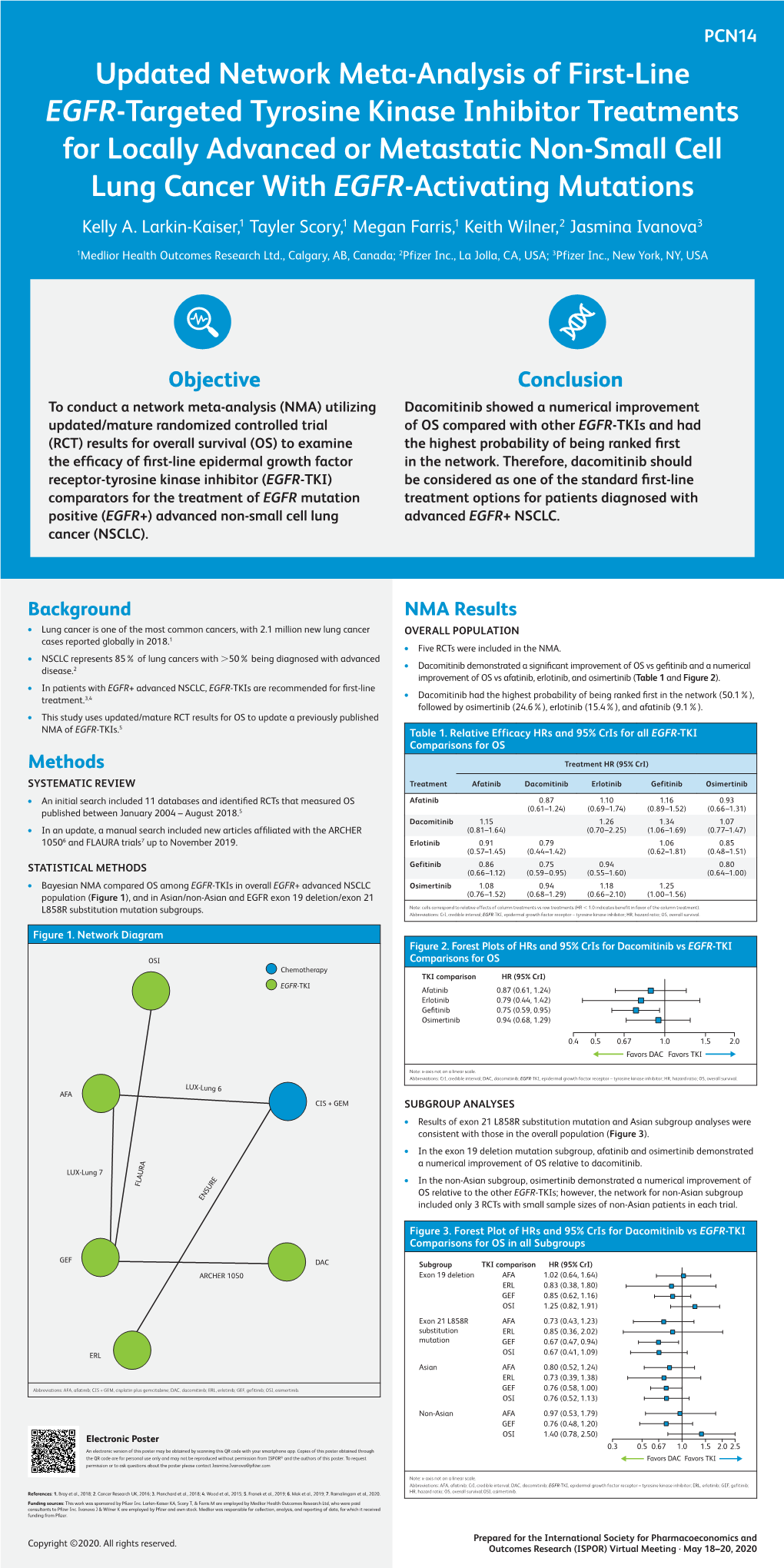
Published OnlineFirst October 30, 2018; DOI: 10.1158/2159-8290.CD-NB2018-143 NEWS IN BRIEF also showed that it could be applicable Dacomitinib Approved, to CD22-targeted CAR T-cell therapy. “What’s really interesting is that but Might Not Be Used they uncovered a gene transfer–related The FDA approved the EGFR inhibi- mechanism of relapse, which I don’t tor dacomitinib (Vizimpro; Pfizer) as a think has been seen before,” says first-line therapy for patients with meta- Marcela Maus, MD, PhD, of Massachu- static, EGFR-mutant non–small cell setts General Hospital Cancer Center lung cancer (NSCLC). Clinicians, how- Structural formula for dacomitinib. in Boston. Inadvertent CAR19 trans- ever, doubt that the drug will be used duction aside, she notes, this single much in clinical practice, as it joins a treating brain metastases (J Clin Oncol B cell likely possessed additional char- crowded field of EGFR inhibitors that 2018 Aug 28 [Epub ahead of print]). acteristics that enabled it to survive includes osimertinib (Tagrisso; Astra- “I still think that osimertinib remains the therapy manufacturing process, Zeneca), the current standard of care. the standard for first-line [therapy] because engineered T cells are typically Instead, they are focused on the next based on toxicity, and based on its quick to eliminate any leukemic cells wave of therapeutic options. ability to elicit meaningful responses in in the patient-derived product. Dacomitinib was approved based on patients with brain metastasis,” he says. Ruella agrees that “some combina- -

First-Line Treatment Options for Patients with Stage IV Non-Small Cell Lung Cancer with Driver Alterations
First-Line Treatment Options for Patients with Stage IV Non-Small Cell Lung Cancer with Driver Alterations Patients with stage IV non-small cell lung cancer Nonsquamous cell carcinoma and squamous cell carcinoma Activating EGFR mutation other Sensitizing (L858R/exon 19 MET exon 14 skipping than exon 20 insertion mutations, EGFR exon 20 mutation ALK rearrangement ROS1 rearrangement BRAF V600E mutation RET rearrangement NTRK rearrangement mutations KRAS alterations HER2 alterations NRG1 alterations deletion) EGFR mutation T790M, L858R or Ex19Del PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options Emerging target; no Emerging target; no Emerging target; no Platinum doublet † † † Osimertinib monotherapy S Afatinib monotherapy M M Alectinib S Entrectinib M Dabrafenib/trametinib M Capmatinib M Selpercatinib M Entrectinib M conclusions available conclusions available conclusions available chemotherapy ± bevacizumab Gefitinib with doublet Standard treatment based on Standard treatment based on Standard treatment based on M M M Brigatinib S Crizotinib M M Tepotinib M Pralsetinib* W Larotrectinib M chemotherapy non-driver mutation guideline non-driver mutation guideline non-driver mutation guideline If alectinib or brigatinib are not available If entrectinib or crizotinib are not available Standard treatment based on Standard treatment based on Standard treatment based on Dacomitinib monotherapy M Osimertinib W M M M Ceritinib S Ceritinib W non-driver mutation guideline non-driver mutation guideline non-driver mutation guideline Monotherapy with afatinib M Crizotinib S Lortlatinib W Standard treatment based on Erlotinib/ramucirumab M M non-driver mutation guideline Erlotinib/bevacizumab M Monotherapy with erlotinib M Strength of Recommendation Monotherapy with gefitinib M S Strong M Moderate W Weak Monotherapy with icotinib M Notes. -

Trastuzumab Emtansine (T-DM1)
Published OnlineFirst September 11, 2018; DOI: 10.1158/1078-0432.CCR-18-1590 Research Article Clinical Cancer Research Trastuzumab Emtansine (T-DM1) in Patients with Previously Treated HER2-Overexpressing Metastatic Non–Small Cell Lung Cancer: Efficacy, Safety, and Biomarkers Solange Peters1, Rolf Stahel2, Lukas Bubendorf3, Philip Bonomi4, Augusto Villegas5, Dariusz M. Kowalski6, Christina S. Baik7, Dolores Isla8, Javier De Castro Carpeno9, Pilar Garrido10, Achim Rittmeyer11, Marcello Tiseo12, Christoph Meyenberg13, Sanne de Haas14, Lisa H. Lam15, Michael W. Lu15, and Thomas E. Stinchcombe16 Abstract Purpose: HER2-targeted therapy is not standard of care Results: Forty-nine patients received T-DM1 (29 IHC 2þ, for HER2-positive non–small cell lung cancer (NSCLC). This 20 IHC 3þ). No treatment responses were observed in the phase II study investigated efficacy and safety of the HER2- IHC 2þ cohort. Four partial responses were observed in the targeted antibody–drug conjugate trastuzumab emtansine IHC 3þ cohort (ORR, 20%; 95% confidence interval, 5.7%– (T-DM1) in patients with previously treated advanced 43.7%). Clinical benefit rates were 7% and 30% in the IHC HER2-overexpressing NSCLC. 2þ and 3þ cohorts, respectively. Response duration for the Patients and Methods: Eligible patients had HER2-over- responders was 2.9, 7.3, 8.3, and 10.8 months. Median expressing NSCLC (centrally tested IHC) and received progression-free survival and overall survival were similar previous platinum-based chemotherapy and targeted between cohorts. Three of 4 responders had HER2 gene therapy in the case of EGFR mutation or ALK gene amplification. No new safety signals were observed. rearrangement. Patients were divided into cohorts based Conclusions: T-DM1 showed a signal of activity in patients on HER2 IHC (2þ,3þ). -

Dacomitinib (Interim Monograph)
Dacomitinib (interim monograph) DRUG NAME: Dacomitinib SYNONYM(S): PF-002998041 COMMON TRADE NAME(S): VIZIMPRO® CLASSIFICATION: molecular targeted therapy Special pediatric considerations are noted when applicable, otherwise adult provisions apply. MECHANISM OF ACTION: Dacomitinib is a second-generation tyrosine kinase inhibitor (TKI). It selectively and irreversibly binds to the kinase domains EGFR/HER1, HER2 and HER4, which inhibits tyrosine kinase autophosphorylation, resulting in reduction of tumour growth and tumour regression. Dacomitinib has activity against the EGFR activating mutations exon 19 deletion and exon 21 L858R substitution.1-4 PHARMACOKINETICS: Oral Absorption bioavailability 80%; steady state within 14 days Distribution extensively distributed throughout the body cross blood brain barrier? yes (equal brain/plasma concentrations based on animal data) volume of distribution 1889 L plasma protein binding 98% Metabolism hepatic via CYP 2D6 (major) and CYP 3A4 (minor) pathways active metabolite(s)2,5 major: O-desmethyl dacomitinib (similar activity to dacomitinib); other: oxidative metabolites (unknown activity) inactive metabolite(s) no information found Excretion mainly fecal elimination urine 3% (<1% parent drug)2,6 feces 79% (20% parent drug)2,6 terminal half life dacomitinib: 70 h (54 to 80 h)2,3 O-desmethyl dacomitinib: 73 h3 clearance 24.9 L/h4 Adapted from standard reference2 unless specified otherwise. USES: Primary uses: Other uses: *Lung cancer, non-small cell *Health Canada approved indication BC Cancer Drug Manual©. All rights reserved. Page 1 of 7 Dacomitinib (interim monograph) This document may not be reproduced in any form without the express written permission of BC Cancer Provincial Pharmacy. Developed: 1 March 2020 Revised: Dacomitinib (interim monograph) SPECIAL PRECAUTIONS: Special populations: • Patients who are female, non-Asian, or 65 years of age or older may experience more serious adverse events than other patients.2 Carcinogenicity: no information found Mutagenicity: Not mutagenic in Ames test. -

Wednesday, June 12, 2019 4:00Pm
Wednesday, June 12, 2019 4:00pm Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review (DUR) Board Members FROM: Melissa Abbott, Pharm.D. SUBJECT: Packet Contents for DUR Board Meeting – June 12, 2019 DATE: June 5, 2019 Note: The DUR Board will meet at 4:00pm. The meeting will be held at 4345 N. Lincoln Blvd. Enclosed are the following items related to the June meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Update on Medication Coverage Authorization Unit/Use of Angiotensin Converting Enzyme Inhibitor (ACEI)/ Angiotensin Receptor Blocker (ARB) Therapy in Patients with Diabetes and Hypertension (HTN) Mailing Update – Appendix B Action Item – Vote to Prior Authorize Aldurazyme® (Laronidase) and Naglazyme® (Galsulfase) – Appendix C Action Item – Vote to Prior Authorize Plenvu® [Polyethylene Glycol (PEG)-3350/Sodium Ascorbate/Sodium Sulfate/Ascorbic Acid/Sodium Chloride/Potassium Chloride] – Appendix D Action Item – Vote to Prior Authorize Consensi® (Amlodipine/Celecoxib) and Kapspargo™ Sprinkle [Metoprolol Succinate Extended-Release (ER)] – Appendix E Action Item – Vote to Update the Prior Authorization Criteria For H.P. Acthar® Gel (Repository Corticotropin Injection) – Appendix F Action Item – Vote to Prior Authorize Fulphila® (Pegfilgrastim-jmdb), Nivestym™ (Filgrastim-aafi), -

HER2-/HER3-Targeting Antibody—Drug Conjugates for Treating Lung and Colorectal Cancers Resistant to EGFR Inhibitors
cancers Review HER2-/HER3-Targeting Antibody—Drug Conjugates for Treating Lung and Colorectal Cancers Resistant to EGFR Inhibitors Kimio Yonesaka Department of Medical Oncology, Kindai University Faculty of Medicine, 377-2 Ohno-Higashi Osaka-Sayamashi, Osaka 589-8511, Japan; [email protected]; Tel.: +81-72-366-0221; Fax: +81-72-360-5000 Simple Summary: Epidermal growth factor receptor (EGFR) is one of the anticancer drug targets for certain malignancies including nonsmall cell lung cancer (NSCLC), colorectal cancer (CRC), and head and neck squamous cell carcinoma. However, the grave issue of drug resistance through diverse mechanisms persists. Since the discovery of aberrantly activated human epidermal growth factor receptor-2 (HER2) and HER3 mediating resistance to EGFR-inhibitors, intensive investigations on HER2- and HER3-targeting treatments have revealed their advantages and limitations. An innovative antibody-drug conjugate (ADC) technology, with a new linker-payload system, has provided a solution to overcome this resistance. HER2-targeting ADC trastuzumab deruxtecan or HER3-targeting ADC patritumab deruxtecan, using the same cleavable linker-payload system, demonstrated promising responsiveness in patients with HER2-positive CRC or EGFR-mutated NSCLC, respectively. The current manuscript presents an overview of the accumulated evidence on HER2- and HER3-targeting therapy and discussion on remaining issues for further improvement of treatments for cancers resistant to EGFR-inhibitors. Abstract: Epidermal growth factor receptor (EGFR) is one of the anticancer drug targets for certain Citation: Yonesaka, K. malignancies, including nonsmall cell lung cancer (NSCLC), colorectal cancer (CRC), and head HER2-/HER3-Targeting and neck squamous cell carcinoma. However, the grave issue of drug resistance through diverse Antibody—Drug Conjugates for mechanisms persists, including secondary EGFR-mutation and its downstream RAS/RAF mutation. -

Evaluation of the Antitumor Activity of Dacomitinib in Models of Human Bladder Cancer
Evaluation of the Antitumor Activity of Dacomitinib in Models of Human Bladder Cancer Petros D Grivas,1,4,5 Kathleen C Day,3,4,5 Andreas Karatsinides,3 Alyssa Paul,3 Nazia Shakir,3 Iya Owainati,3 Monica Liebert,3 Lakshmi P Kunju,2 Dafydd Thomas,2 Maha Hussain,1,3,5 and Mark L Day3,4,5 1Division of Hematology/Oncology, Department of Internal Medicine, 2Department of Pathology, 3Department of Urology, 4Translational Oncology Program, and 5University of Michigan Comprehensive Cancer Center, University of Michigan, Ann Arbor, Michigan, United States of America Members of the human epidermal growth factor receptor (HER) family play a significant role in bladder cancer progression and may underlie the development of chemotherapy resistance. Dacomitinib is an irreversible tyrosine kinase inhibitor with structural specificity for the catalytic domains of epidermal growth factor receptor (EGFR), HER2 and HER4 that has exhibited vigorous effi- cacy against other solid tumors. We evaluated the antitumor activity of dacomitinib in human bladder cancer cell lines express- ing varying levels of HER family receptors. These cell lines also were established as bladder cancer xenografts in nonobese diabetic/severe combined immunodeficiency (NOD/SCID) mice to assess dacomitinib activity in vivo. Significant cytotoxic and cytostatic effects were noted in cells expressing elevated levels of the dacomitinib target receptors with apoptosis and cell cycle arrest being the predominant mechanisms of antitumor activity. Cells expressing lower levels of HER receptors were much less sen- sitive to dacomitinib. Interestingly, dacomitinib was more active than either trastuzumab or cetuximab in vitro, and exhibited in- creased growth inhibition of bladder tumor xenografts compared with lapatinib. -

Lung Cancer Agents – Unified Formulary
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Pharmacy Policy Lung Cancer Agents – Unified Formulary Policy Number: 9.712 Version Number: 1.1 Version Effective Date: 3/3/2021 Product Applicability All Plan+ Products Well Sense Health Plan Boston Medical Center HealthNet Plan New Hampshire Medicaid MassHealth- MCO MassHealth- ACO Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options Note: Disclaimer and audit information is located at the end of this document. Prior Authorization Policy Reference Table: Drugs that require PA No PA Alecensa® (alectinib) Alunbrig® (brigatinib) Gilotrif® (afatinib) Iressa® (gefitinib) Lorbrena® (lorlatinib) Tabrecta® (capmatinib) Tagrisso® (osimertinib) Tarceva® (erlotinib) * Vizimpro® (dacomitinib) Xalkori® (crizotinib) Zykadia® (ceritinib) *A-rated generic available. Both brand and A-rated generic require PA. + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. The Plan operates in Massachusetts under the trade name Boston Medical Center HealthNet Plan and in other states under the trade name Well Sense Health Plan. Lung Cancer Agents 1 of 7 Procedure: Approval Diagnosis: Advanced or metastatic non-small cell lung cancer (All agents) Advanced or metastatic pancreatic cancer (erlotinib) Stage IIB to IIIA NSCLC (Tagrisso®) Approval Criteria: Prescriber provides documentation of ALL of the following: 1. Appropriate diagnosis* Alecensa® (alectinib) 2. Prescriber is an oncologist 3. Appropriate dosing Zykadia® (ceritinib) 4. Cancer is anaplastic lymphoma kinase (ALK)-positive (Documentation must be provided on the PA request or in attached medical records) 5. ONE of the following: a. If the request is for Alecensa® (alectinib), quantity requested is ≤8 units/day b. -

Lung Cancer: Dacomitinib
RESEARCH HIGHLIGHTS Nature Reviews Clinical Oncology 12, 3 (2015); published online 25 November 2014; doi:10.1038/nclinonc.2014.210 LUNG CANCER Dacomitinib: getting on target after negative ARCHER trial Despite the progress made in treating setting did not demonstrate any outcome To establish whether dacomitinib patients with non-small-cell lung cancer advantage for dacomitinib. However, the represents a new treatment advance in (NSCLC) with standard-of-care EGFR role of dacomitinib in the first-line setting patients with advanced-stage EGFR-mutant tyrosine kinase inhibitors (TKI), such as in patients with activating EGFR mutations NSCLC, this drug needs to be compared gefitinib, in the first-line setting, it is well has not been investigated. directly with a first-line agent; in this regard, known that patients inevitably develop Pasi Jänne and coauthors now reveal a phase III trial comparing dacomitinib with drug resistance within 1 year and relapse. encouraging data from a multicentre, gefitinib as initial therapy for patients Hence, new therapeutic approaches are phase II trial that assessed dacomitinib with advanced-stage disease in ongoing. desperately needed. (30 mg or 45 mg) in 89 patients with Dacomitinib is a pan-HER inhibitor advanced-stage NSCLC (45 had EGFR Lisa Hutchinson that targets EGFR, HER2 and HER4, and mutations). Patients with known KRAS has shown promising preclinical activity. mutations or known EGFR wild-type Original article Jänne, P. et al. Dacomitinib as first-line As is often the case, targeted agents do not disease and nonadenocarcinoma disease treatment in patients with clinically or molecularly selected provide survival advantages in unselected were excluded. -

Oral Adverse Events Associated with Targeted Cancer Therapies
Oral adverse events associated with targeted cancer therapies Milda Chmieliauskaite, DMD, MPH ¢ Ivan Stojanov, DMD ¢ Mana Saraghi, DMD Andres Pinto, DMD, MPH, MSCE, MBA, FDSRCS (Edin) Over the past decade, targeted therapies have emerged ancer is the second-leading cause of death in the as promising forms of cancer treatment and are increas- United States. At some point in time, many dental ingly included in chemotherapeutic regimens for an patients will be undergoing cancer treatment. ever-growing list of human cancers. Targeted therapies C Conventional chemotherapeutic agents are cytotoxic to all repli- are so-named due to their specific targeting of dysregu- cating cells and do not target specific cancer cells; many adverse lated signaling pathways in cancer cells. This enhanced effects are attributable to this lack of discrimination. Many new discrimination between tumor and normal cells is a more cancer drugs are referred to as targeted therapy because they promising and efficacious approach to cancer treatment target dysregulated signaling pathways specific to a particular than conventional cytotoxic chemotherapy. However, tar- type of cancer to inhibit cancer cell growth or survival. As geted therapies still have side effects, and some manifest these therapies do not simply target any and all replicating cells, in the oral cavity. Oral adverse events tend to be mild their effects promise to be more specific than conventional 1 and thus may be overlooked in the context of a patient’s chemotherapy. overarching diagnosis and management. These oral Despite an improvement in their overall side effect profile, lesions are often noted during an intraoral examination targeted therapies still manifest adverse effects, including oral and identified in the context of the patient’s medical his- and perioral lesions. -

A Guide to Treatment
A Guide to Treatment While there are data in this guide that are found within the product labeling, this guide also includes data and information regarding potential management strategies from post hoc analyses that are not included in the product labeling, and are indicated as such throughout. INDICATION VIZIMPRO is indicated for the first-line treatment of patients with metastatic non-small cell lung cancer (NSCLC) with epidermal growth factor receptor (EGFR) exon 19 deletion or exon 21 L858R substitution mutations as detected by an FDA-approved test. SELECTED SAFETY INFORMATION There are no contraindications for VIZIMPRO Interstitial Lung Disease (ILD): Severe and fatal ILD/pneumonitis occurred in patients treated with VIZIMPRO and occurred in 0.5% of the 394 VIZIMPRO-treated patients; 0.3% of cases were fatal. Monitor patients for pulmonary symptoms indicative of ILD/pneumonitis. Withhold VIZIMPRO and promptly investigate for ILD in patients who present with worsening of respiratory symptoms which may be indicative of ILD (e.g., dyspnea, cough, and fever). Permanently discontinue VIZIMPRO if ILD is confirmed. Please see Important Safety Information on page 30. Please see Full Prescribing Information at VIZIMPROhcp.com. Table of contents Start the treatment plan with VIZIMPRO® (dacomitinib) ................................. Page 3 VIZIMPRO efficacy ............................................................................. Page 6 VIZIMPRO safety profile ...................................................................... Page 8 -

Tyrosine Kinase Inhibitors in Cancer: Breakthrough and Challenges of Targeted Therapy
cancers Review Tyrosine Kinase Inhibitors in Cancer: Breakthrough and Challenges of Targeted Therapy 1,2, 3,4 1 2 3, Charles Pottier * , Margaux Fresnais , Marie Gilon , Guy Jérusalem ,Rémi Longuespée y 1, and Nor Eddine Sounni y 1 Laboratory of Tumor and Development Biology, GIGA-Cancer and GIGA-I3, GIGA-Research, University Hospital of Liège, 4000 Liège, Belgium; [email protected] (M.G.); [email protected] (N.E.S.) 2 Department of Medical Oncology, University Hospital of Liège, 4000 Liège, Belgium; [email protected] 3 Department of Clinical Pharmacology and Pharmacoepidemiology, University Hospital of Heidelberg, 69120 Heidelberg, Germany; [email protected] (M.F.); [email protected] (R.L.) 4 German Cancer Consortium (DKTK)-German Cancer Research Center (DKFZ), 69120 Heidelberg, Germany * Correspondence: [email protected] Equivalent contribution. y Received: 17 January 2020; Accepted: 16 March 2020; Published: 20 March 2020 Abstract: Receptor tyrosine kinases (RTKs) are key regulatory signaling proteins governing cancer cell growth and metastasis. During the last two decades, several molecules targeting RTKs were used in oncology as a first or second line therapy in different types of cancer. However, their effectiveness is limited by the appearance of resistance or adverse effects. In this review, we summarize the main features of RTKs and their inhibitors (RTKIs), their current use in oncology, and mechanisms of resistance. We also describe the technological advances of artificial intelligence, chemoproteomics, and microfluidics in elaborating powerful strategies that could be used in providing more efficient and selective small molecules inhibitors of RTKs.