International Standards for the Treatment of Drug Use Disorders — Draft for Field Testing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Substance Abuse and Dependence
9 Substance Abuse and Dependence CHAPTER CHAPTER OUTLINE CLASSIFICATION OF SUBSTANCE-RELATED THEORETICAL PERSPECTIVES 310–316 Residential Approaches DISORDERS 291–296 Biological Perspectives Psychodynamic Approaches Substance Abuse and Dependence Learning Perspectives Behavioral Approaches Addiction and Other Forms of Compulsive Cognitive Perspectives Relapse-Prevention Training Behavior Psychodynamic Perspectives SUMMING UP 325–326 Racial and Ethnic Differences in Substance Sociocultural Perspectives Use Disorders TREATMENT OF SUBSTANCE ABUSE Pathways to Drug Dependence AND DEPENDENCE 316–325 DRUGS OF ABUSE 296–310 Biological Approaches Depressants Culturally Sensitive Treatment Stimulants of Alcoholism Hallucinogens Nonprofessional Support Groups TRUTH or FICTION T❑ F❑ Heroin accounts for more deaths “Nothing and Nobody Comes Before than any other drug. (p. 291) T❑ F❑ You cannot be psychologically My Coke” dependent on a drug without also being She had just caught me with cocaine again after I had managed to convince her that physically dependent on it. (p. 295) I hadn’t used in over a month. Of course I had been tooting (snorting) almost every T❑ F❑ More teenagers and young adults die day, but I had managed to cover my tracks a little better than usual. So she said to from alcohol-related motor vehicle accidents me that I was going to have to make a choice—either cocaine or her. Before she than from any other cause. (p. 297) finished the sentence, I knew what was coming, so I told her to think carefully about what she was going to say. It was clear to me that there wasn’t a choice. I love my T❑ F❑ It is safe to let someone who has wife, but I’m not going to choose anything over cocaine. -

Substance Use Disorders (SUD) Begin in Childhood Or Adolescence (Kandel, 1992)
PSYCHIATRY TELEHEALTH, LIAISON & CONSULTS (PSYCH TLC) Substance Related Disorders in Children and Adolescents Written and initially reviewed, 11/2011: Zaid Malik, M.D. Deepmala Deepmala, M.D Jody Brown, M.D. Laurence Miller, M.D. Reviewed and updated, 03/04/2014: Deepmala Deepmala, M.D. Work submitted by Contract # 4600016732 from the Division of Medical Services, Arkansas Department of Human Services 1 | P a g e Department of Human Services Psych TLC Phone Numbers: 501-526-7425 or 1-866-273-3835 The free Child Psychiatry Telemedicine, Liaison & Consult (Psych TLC) service is available for: Consultation on psychiatric medication related issues including: . Advice on initial management for your patient . Titration of psychiatric medications . Side effects of psychiatric medications . Combination of psychiatric medications with other medications Consultation regarding children with mental health related issues Psychiatric evaluations in special cases via tele-video Educational opportunities This service is free to all Arkansas physicians caring for children. Telephone consults are made within 15 minutes of placing the call and can be accomplished while the child and/or parent are still in the office. Arkansas Division of Behavioral Health Services (DBHS): (501) 686-9465 http://humanservices.arkansas.gov/dbhs/Pages/default.aspx 2 | P a g e Substance Related Disorders in Children and Adolescents ______________________________________________________ Table of Contents 1. Epidemiology 2. Symptomatology 3. Diagnostic Criteria -- Highlights of Changes from DSM IV to DSM 5 3.1 Substance Use Disorder 3.2 Substance Induced Disorder 3.2.1 Substance Withdrawal 3.2.2 Substance Intoxication 3.2.3 Substance/Medication-Induced Mental Disorders 4. Etiology, Risk Factors and Protective Factors 4.1 Etiology 4.2 Risk Factors and Protective Factors 5. -

Treatment of Patients with Substance Use Disorders Second Edition
PRACTICE GUIDELINE FOR THE Treatment of Patients With Substance Use Disorders Second Edition WORK GROUP ON SUBSTANCE USE DISORDERS Herbert D. Kleber, M.D., Chair Roger D. Weiss, M.D., Vice-Chair Raymond F. Anton Jr., M.D. To n y P. G e o r ge , M .D . Shelly F. Greenfield, M.D., M.P.H. Thomas R. Kosten, M.D. Charles P. O’Brien, M.D., Ph.D. Bruce J. Rounsaville, M.D. Eric C. Strain, M.D. Douglas M. Ziedonis, M.D. Grace Hennessy, M.D. (Consultant) Hilary Smith Connery, M.D., Ph.D. (Consultant) This practice guideline was approved in December 2005 and published in August 2006. A guideline watch, summarizing significant developments in the scientific literature since publication of this guideline, may be available in the Psychiatric Practice section of the APA web site at www.psych.org. 1 Copyright 2010, American Psychiatric Association. APA makes this practice guideline freely available to promote its dissemination and use; however, copyright protections are enforced in full. No part of this guideline may be reproduced except as permitted under Sections 107 and 108 of U.S. Copyright Act. For permission for reuse, visit APPI Permissions & Licensing Center at http://www.appi.org/CustomerService/Pages/Permissions.aspx. AMERICAN PSYCHIATRIC ASSOCIATION STEERING COMMITTEE ON PRACTICE GUIDELINES John S. McIntyre, M.D., Chair Sara C. Charles, M.D., Vice-Chair Daniel J. Anzia, M.D. Ian A. Cook, M.D. Molly T. Finnerty, M.D. Bradley R. Johnson, M.D. James E. Nininger, M.D. Paul Summergrad, M.D. Sherwyn M. -

Substance Induced Disorders
Substance Induced Disorders Julie Kmiec, DO University of Pittsburgh AOAAM 2018 Objectives At the end of this lecture, participants should be able to: ❖Understand the difference between substance induced disorders and independent psychiatric disorders ❖Be able to diagnose substance induced disorder versus independent mood, anxiety, or psychotic disorder ❖Discuss typical treatment for independent psychiatric disorders ❖Understand the importance of differentiating between substance-induced and independent psychiatric disorders List of Substances in DSM ❖Alcohol ❖Caffeine ❖Cannabis ❖Hallucinogens (ecstasy, LSD, PCP, mescaline, etc) ❖Inhalants ❖Opioids ❖Sedatives, hypnotics, and anxiolytics ❖Stimulants (amphetamines, cocaine, and other stimulants) ❖Tobacco ❖Other (or unknown) substances DSM-5, 2013 DIAGNOSES ASSOCIATED WITH CLASS OF SUBSTANCE Substance Anxiety Depress Bipolar Psychotic OC Neuroco Sleep Delirium Sexual gnitive alcohol I/W I/W I/W I/W I/W/P I/W I/W I/W cannabis I I I/W I hallucinogen I I I I I inhalant I I I I/P I opioid W I/W I/W I/W I/W sedative W I/W I/W I/W I/W/P I/W I/W I/W stimulant I/W I/W I/W W I/W I/W I I caffeine I I/W tobacco W Onset during I = intoxication; W = withdrawal P = persisting DSM-5, 2013 DIAGNOSES ASSOCIATED WITH CLASS OF SUBSTANCE Substance SUD Intoxication Withdrawal alcohol X X X cannabis X X X hallucinogen X X inhalant X X opioid X X X sedative X X X stimulant X X X caffeine X X tobacco X X DSM-5, 2013 Diagnosis ❖Difficult to diagnose psychiatric disorders when someone actively using substance ❖Symptoms -

Phenomenology Epidemiology
Phenomenology DEFINITIONS Intoxication: reversible, substance-specific physiological and behavioral changes due to recent exposure to a psychoactive substance. Addiction: compulsion to use a drug, usually for its psychic, rather than therapeutic, effects Tolerance: the decline in potency of an opioid experienced with continued use, so that higher doses are needed to achieve the same effect. This is a receptor mediated effect, typical of many psychoactive drugs. Physical Dependence: refers to the development of withdrawal symptoms once a drug is stopped. Withdrawal: a physiological state that follows cessation or reduction in the amount of a drug used. Generally these effects are the opposite of the drugs normal effects. Substance Dependence (DSM version): A maladaptive pattern of substance use with adverse clinical consequences. Substance Abuse (DSM version): A maladaptive pattern of use that causes clinically significant impairment. Alcoholism: A repetitive, but inconsistent and sometimes unpredictable loss of control of drinking which produces symptoms of serious dysfunction or disability. Clearly there is a wide range of findings possible on the mental status exam, however any exam should look for typical signs of regular substance use. Epidemiology Use of psychoactive substances is common in society, and is often socially acceptable or at least tolerated. Historically, psychoactive substance has served a variety of purposes, including medicinal, social, recreational and religious. In the U.S., 90% people report some alcohol use, 80% report some caffeine use, 25% report use of tobacco products, and 37% report having used illicit substances (at least once in life). Dependence and Abuse are also very common (13.6% in ECA). Over 10 million Americans are alcoholics, over 8 million are "Problem drinkers." Only 3% of alcoholics are on skid row. -

MARIJUANA and SUBSTANCE USE DISORDER, Part 1: a Historical Perspective and DSM-5 Overview
MARIJUANA AND SUBSTANCE USE DISORDER, Part 1: a historical perspective and DSM-5 overview Introduction Marijuana is the most widely used illicit drug in the Western world and the third most commonly used recreational drug after alcohol and tobacco. According to the World Health Organization, it also is the illicit substance most widely cultivated, trafficked, and used. Although the long-term clinical outcome of marijuana use disorder may be less severe than other commonly used substances, it is by no means a "safe" drug. Sustained marijuana use can have negative impacts on the brain as well as the body. Studies have indicated a link between regular marijuana use and schizophrenia as well as a demonstrated relationship between marijuana use and a higher incidence of lung cancer. Although there are no pharmacological treatments available with a proven impact on marijuana use disorder, there are several types of behavior therapy that may be effective in treating this disorder. Worldwide Use Of Marijuana For a number of years, the United Nations has been compiling annual surveys of worldwide drug use, including cannabis. Reflecting the difficulties and uncertainties associated with developing estimates of the number of people who use drugs (such as the quality of the data gathered and the methodologies used to sample populations), the latest United Nations estimates are presented in ranges, reflecting the lower and upper estimates indicated through the array of surveys ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com 1 available. In their 2012 report (covering 2010), the United Nations estimated that between 119.4 and 224.5 million people between the ages of 15 and 64 had used cannabis in the past year, representing between 2.6% and 5.0% of the world’s population.22 In 2014, approximately 22.2 million people ages 12 and up reported using marijuana during the past month. -

Current Concepts on Drug Abuse and Dependence Daniela Luiza Baconi Carol Davila University of Medicine and Pharmacy, Daniela [email protected]
Journal of Mind and Medical Sciences Volume 2 | Issue 1 Article 4 2015 Current Concepts on Drug Abuse and Dependence Daniela Luiza Baconi Carol Davila University of Medicine and Pharmacy, [email protected] Anne-Marie Ciobanu Carol Davila University of Pharmacy and Medicine Ana Maria Vlăsceanu Carol Davila University of Medicine and Pharmacy Oana Denisa Cobani St. John Emergency Hospital Carolina Negrei Carol Davila University of Medicine and Pharmacy See next page for additional authors Follow this and additional works at: http://scholar.valpo.edu/jmms Part of the Medicine and Health Sciences Commons Recommended Citation Baconi, Daniela Luiza; Ciobanu, Anne-Marie; Vlăsceanu, Ana Maria; Cobani, Oana Denisa; Negrei, Carolina; and Bălălău, Cristian (2015) "Current Concepts on Drug Abuse and Dependence," Journal of Mind and Medical Sciences: Vol. 2 : Iss. 1 , Article 4. Available at: http://scholar.valpo.edu/jmms/vol2/iss1/4 This Review Article is brought to you for free and open access by ValpoScholar. It has been accepted for inclusion in Journal of Mind and Medical Sciences by an authorized administrator of ValpoScholar. For more information, please contact a ValpoScholar staff member at [email protected]. Current Concepts on Drug Abuse and Dependence Authors Daniela Luiza Baconi, Anne-Marie Ciobanu, Ana Maria Vlăsceanu, Oana Denisa Cobani, Carolina Negrei, and Cristian Bălălău This review article is available in Journal of Mind and Medical Sciences: http://scholar.valpo.edu/jmms/vol2/iss1/4 JMMS 2015, 2(1): 18- 33. REVIEW Current concepts on drug abuse and dependence Daniela Luiza Baconi1, Anne-Marie Ciobanu2, Ana Maria Vlăsceanu1, Oana Denisa Cobani3, Carolina Negrei1, Cristian Bălălău4 1 Carol Davila University of Medicine and Pharmacy, Faculty of Pharmacy, Department of Toxicology 2 Carol Davila University of Medicine and Pharmacy, Faculty of Pharmacy, Medicines Control 3 St. -

A Guide to Substance Abuse Services for Primary Care Clinicians
Substance Abuse and Mental Health Services Administration Center for Substance Abuse Treatment A Guide to Substance Abuse Services for Primary Care Clinicians Treatment Improvement Protocol (TIP) Series 24 A Guide to Substance Abuse Services for Primary Care Clinicians Treatment Improvement Protocol (TIP) Series 24 Eleanor Sullivan, Ph.D., R.N., F.A.A.N. Michael Fleming, M.D., M.P.H. Consensus Panel Co-Chairs U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Substance Abuse and Mental Health Services Administration Center for Substance Abuse Treatment 1 Choke Cherry Road Rockville, MD 20857 This publication is part of the Substance Abuse I.C.A.D.C., served as the CSAT government Prevention and Treatment Block Grant technical project officer. Paddy Cook, Constance Grant assistance program. All material appearing in Gartner, M.S.W., Lise Markl, Randi Henderson, this volume except that taken directly from Margaret K. Brooks, Esq., Donald Wesson, M.D., copyrighted sources is in the public domain and Mary Lou Dogoloff, Virginia Vitzthum, and may be reproduced or copied without Elizabeth Hayes served as writers. Special permission from the Substance Abuse and thanks to Daniel Vinson, M.D., M.S.H.P., Mim J. Mental Health Services Administration’s Landry, Mary Smolenski, C.R.N.P., Ed.D., (SAMHSA) Center for Substance Abuse MaryLou Leonard, Pamela Nicholson, Annie Treatment (CSAT) or the authors. Citation of Thornton, Jack Rhode, Cecil Gross, Niyati the source is appreciated. Do not reproduce or Pandya, and Wendy Carter for their distribute this publication for a fee without considerable contributions to this document. -

Guidelines for the Management of Psychoactive Substance Intoxication
Guidelines for the Management of Psychoactive Substance Intoxication & Withdrawal in Kwa Zulu Natal Table of Contents 1. General Information 2. Where & by whom should intoxication and withdrawal be damaged 3. Guidelines for outpatients/community withdrawals 4. Screening for substance abuse/ dependence 5. Recommended Interventions 6. Brief interventions 7. What if the client refuses help? 8. General Principals for detoxification 9. Flow diagram of referral pathways 10. How to manage Clients with Alcohol problems 11. How to manage Cannabis problems 12. How to manage Mandrax problems 13. How to manage Opioid problems 14. How to manage Stimulant problems - Cocaine - Amphetamines (including Tik) 15. How to manage Ecstasy problems 16. How to manage Hallucinogen problems 17. How to manage Volatile Substance (inhalant) 18. How to manage Benzodiazepine problems Detoxification protocols for children and adolescents with substance use disorders 19. Alcohol 20. Cannabis/ Cannabis & Mandrax 21. Opioids 22. Benzodiazepines 23. Hallucinogens 24. Volatile solvents 25. Nicotine 26. Useful phone numbers Page 2 MANAGEMENT OF SUBSTANCE USE DISORDERS (SUD): General information: The treatment of SUD begins with the medical stabilisation of the patient (dealing with intoxication, withdrawal and medical complications). Medical stabilisation is however not a sufficient intervention to ensure future sobriety. It needs to be followed by an intervention to prevent relapse back to substance use. Brief interventions may be used in cases of misuse or abuse. (See brief interventions below) Patients who fulfil criteria for dependence need a referral to a specialist addiction treatment service. This does not “cure” the patient, but provide tools and the support necessary to maintain sobriety. Relapses and lapses (short periods of relapse) may still happen and should be viewed as a learning opportunity. -

Substance-Related Disorders
CHAPTER :12 Substance-Related Disorders TOPIC OVERVIEW Depressants Alcohol Sedative-Hypnotic Drugs Opioids Stimulants Cocaine Amphetamines Caffeine Hallucinogens Cannabis Combinations of Substances What Causes Substance-Related Disorders? The Sociocultural View The Psychodynamic View Cognitive-Behavioral Views The Biological View How Are Substance-Related Disorders Treated? Psychodynamic Therapies Behavioral Therapies Cognitive-Behavioral Therapies Biological Treatments Sociocultural Therapies Putting It Together: New Wrinkles to a Familiar Story 157 158 CHAPTER 12 LECTURE OUTLINE I. SUBSTANCE-RELATED DISORDERS A. What is a drug? 1. Any substance other than food that affects our bodies or minds a. Need not be a medicine or be illegal B. Current language uses the term substance rather than drug to overtly include alcohol, to- bacco, and caffeine C. Substances may cause temporary changes in behavior, emotion, or thought 1. May result in substance intoxication (literally, “poisoning”), a temporary state of poor judgment, mood changes, irritability, slurred speech, and poor coordination 2. Some substances such as LSD may produce a particular form of intoxication, some- times call hallucinosis, which consists of perceptual distortion and hallucinations D. Some substances also can produce long-term problems: 1. Substance abuse: A pattern of behavior where a person relies on a drug excessively and chronically, damaging relationships, affecting work functioning, and/or putting self or others in danger 2. Substance dependence: A more advanced pattern of use where a person abuses a drug and centers his or her life around it a. Also called addiction b. May include tolerance (need increasing doses to get an effect) and withdrawal (unpleasant and dangerous symptoms when substance use is stopped or cut down) E. -

CCHCS Care Guide: Intoxication and Withdrawal SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF-MANAGEMENT GOALS ALERTS
October 2020 CCHCS Care Guide: Intoxication and Withdrawal SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF-MANAGEMENT GOALS ALERTS Recognize signs and symptoms of intoxication/ Patients who present with an opioid overdose should be withdrawal that may need stabilization at a higher level referred to an addiction provider (the Addiction Medicine of care (HLOC) Central Team [AMCT] or institution Addiction Medicine Successfully treat symptoms of withdrawal in a way Champion) for evaluation that facilitates opportunities to offer access to treatment Severe respiratory depression, unstable vital signs, altered for substance use disorder (SUD) level of consciousness, risk for sympathetic storm should be Patients who are eligible and interested in pursuing referred to a HLOC SUD treatment should be referred to addiction services Patients presenting with altered level of consciousness typical (See CCHCS Care Guide: Substance Use Disorder) of intoxication should also be checked for possible coinciding injury that can complicate their presentation ASSESSMENT The first step is stabilizing patient and airway, then determine whether signs and symptoms warrant transfer to a HLOC, or if the patient can be successfully treated within the institution in a treatment and triage area (TTA) or inpatient medical bed. The identification of withdrawal or intoxication must begin with the collection of pertinent patient information including: patient history, physical examination, and laboratory screening. Use intoxication diagnostic codes – search under intoxication and select for the specific substance(s) used. The signs and symptoms of intoxication and withdrawal differ by the specific type of substance used. This Care Guide covers intoxication and withdrawal related to the following substances: Alcohol (Pages 5-6) Opioids (Pages 7-9) Stimulants (Page 10) Sedative-Hypnotics (Page 11) TREATMENT Treatment for Intoxication For substances other than opioids and benzodiazepines, there are no specific antagonist (reversal) agents to treat an intoxication. -
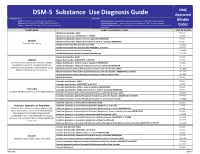
DSM-5 Substance Use Diagnosis Guide
DMC DSM-5 Substance Use Diagnosis Guide Approved SEVERITY LEVELS SPECIFIERS Billable o Mild = Presence of 2-3 DSM-5 criteria symptoms o Early Remission = 3 months to 1 year with no presence of DSM-5 criteria symptoms o Moderate = Presence of 4-5 DSM-5 criteria symptoms o Sustained Remission = 1 year or more with no presence of DSM-5 criteria symptoms o Severe = Presence of 6 or more DSM-5 criteria symptoms o In Controlled Environment = If individual is in an environment where access to substances are Codes restricted SUBSTANCE DSM-5 DIAGNOSIS LABEL ICD-10 CODES Alcohol Use Disorder, MILD F10.10 Alcohol Use Disorder, MODERATE or SEVERE F10.20 Alcohol Use Disorder, Mild in early or sustained REMISSION F10.11 Alcohol Alcohol Use Disorder, Moderate or Severe in early or sustained REMISSION F10.21 Example: beer, liquor Alcohol Intoxication with Use Disorder, MILD F10.129 Alcohol Intoxication with Use Disorder, MODERATE or SEVERE F10.229 Alcohol Intoxication without Use Disorder F10.929 Alcohol Withdrawal without Perceptual Disturbances F10.239 Opioid Use Disorder, MILD F11.10 Opioid Opioid Use Disorder, MODERATE or SEVERE F11.20 Example: Heroin, Hydrocodone (Norco, Vicodin), Opioid Use Disorder, Mild in early or sustained REMISSION F11.11 Oxycodone (OxyContin, Percocet), Morphine, Opioid Use Disorder, Moderate or Severe in early or sustained REMISSION F11.21 Hydomorphone (Dilaudid), Codeine (cough syrup), Opioid Intoxication without Perceptual Disturbances with Use Disorder, MILD F11.129 Meperidine (Demerol), Fentanyl, etc. Opioid Intoxication