IVF40 Final Programme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Full Programme
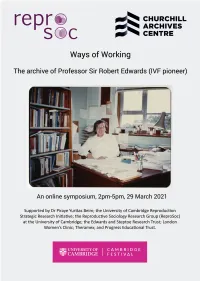
Ways of Working online symposium programme 2.00pm-2.05pm Welcome from Allen Packwood, Director of Churchill Archives Centre. 2.05pm-2.35pm Madelin Evans (Edwards Papers Archivist, Churchill Archives Centre) and Professor Nick Hopwood (Department of History and Philosophy of Science, University of Cambridge) in conversation about using the archive of Robert Edwards for research. 2.35pm-3.05pm Professor Sarah Franklin (Reproductive Sociology Research Group, University of Cambridge) and Gina Glover (Artist, creator of Art in ART: Symbolic Reproduction exhibition) on working with images of reproduction in the Edwards archive. 3.05pm-3.15pm Break, with the chance to view a film of Art in ART: Symbolic Reproduction exhibition by Gina Glover 3.15pm-3.45pm Dr Kay Elder (Senior Research Scientist, Bourn Hall Clinic) and Dr Staffan Müller-Wille (University Lecturer, Department of History and Philosophy of Science, University of Cambridge) on using clinical research notebooks, and scientific notebooks and manuscripts, for historical research. 3.45pm-4.15pm Professor Sir Richard Gardner (Emeritus Royal Society Research Professor in the University of Oxford) and Professor Roger Gosden (lately Professor at Cornell University, now Visiting Scholar at William & Mary and official biographer of Robert Edwards) on Robert Edwards’ style of working in the laboratory. 4.15pm-4.30pm Dr Jenny Joy (daughter of Robert Edwards, key in gathering together his archive) will talk about her experience of how her father worked. 4.30pm-5pm Concluding remarks, questions and discussion The Papers of Professor Sir Robert Edwards, at Churchill Archives Centre The archive comprises 141 boxes of personal and scientific papers including correspondence, research and laboratory notebooks, draft publications and journal articles, newspaper clippings, photographs, videos and film. -

IVF Histories and Cultures Workshop 3 22-23Rd June 2015, Christ's
IVF Histories and Cultures Workshop 3 22-23rd June 2015, Christ’s College Cambridge Monday June 22nd 2015 Plumb Auditorium, Christ’s College 12:00 – 12:45pm Lunch and Registration 12:45 – 1:30pm Opening Remarks & Workshop Introduction 1:30 - 3:00pm Panel 1 Staging Embryos Presenters: Roger Gosden, Kay Elder Chair: Susan Squier 3:00 – 3:30pm Tea & Coffee 3:30-4:30pm Panel 2 Cellular Time Presenter: Merete Lie Discussant: Manuela Perrotta Chair: Carrie Friese 4:30 – 5:00pm Break 5:00 - 6:30pm Plenary 1: Nick Hopwood (The Yusuf Hamied Theatre) Chair: Martin Johnson 6:30 – 7:00pm Reception 7:00 – 9:00pm Dinner Tuesday June 23rd 2015 Plumb Auditorium, Christ’s College 9:30 – 11:00am Panel 3, Time Lapses Presenters: Gaëlle Recher, Simon Fishel Discussant: Andrew Webster Chair: Bob Moor 11:00 – 11:30pm Tea & Coffee 11:30 - 1:00pm Panel 4, Freeze Frames Presenter: Lucy van de Wiel Discussant: Suzanne Anker Chair: Gina Glover 1:00 – 2:00pm Lunch 2:00-3:30pm ‘Biological Clocks’ Small Group Discussions and Feedback 3:30 – 4:00pm Break 4:00 - 5:30pm Plenary 2: Hannah Landecker (The Yusuf Hamied Theatre) 5:30 – 6:00pm Closing Reception Welcome ‘Time Lines, Time Lapses’ In this, our third ESRC-funded workshop, we will be considering the question of embryonic development as a visual and serial sequence, with particular reference to the recent introduction of time lapse imagery into clinical IVF. Described as one of the most significant technological improvements to modern IVF, time lapse imagery is also a technique that has a long history in the context of basic experimental science. -

It Was at the 77Th Meeting of ESHRE's Executive Committee in April
PREFACE t was at the 77th meeting of ESHRE’s Executive Committee in April I 2002 that the prospect of writing the society’s history was first formally discussed. In fact, the seed of the idea had been sown a few months earlier by ESHRE’s new chairman at the time, Hans Evers, and chairman elect Arne Sunde. After their nominations had been approved at the 2001 annual meeting in Lausanne, both Evers and Sunde had immediately set about the composition of a 16-point strategy report for the Executive Committee, designed to take ESHRE’s management forward over the following three or four years. Section 16 of that report, under the heading of “other items”, was a proposal that ESHRE’s past chairmen should collect “the important documents and illustrations from their term of office” with a view to recording the society’s history. Now, in the spring of 2002, as the Executive Committee sat down at ESHRE’s Central Office in the suburbs of Brussels to battle their way through the strategic plan, they too recognised the huge advance in reproductive medicine reflected in ESHRE’s history. A record of that history would indeed represent ESHRE’s place within that advance - and ESHRE’s contribution to it. The Executive Committee thus did what it always did when faced with a proposal which required consideration and planning: it formed a committee. The ESHRE History Task Force was set up at that meeting in April 2002 under the chairmanship of Basil Tarlatzis; joining him on the committee were his fellow past chairmen Jean Cohen, Pier Giorgio Crosignani, Klaus Diedrich and Andre´ Van Steirteghem. -

HFEA ANNUAL REPORT 2000.Qxd
Human Fertilisation and Embryology Authority NINTH ANNUAL REPORT & ACCOUNTS 2000 Human Fertilisation and Embryology Authority, 30 Artillery lane, London E1 7LS Telephone: 0207 377 5077 Fax: 0207 377 1871 Website: http://www.hfea.gov.uk First published 2000 Copyright © HFEA 2000 This report covers the year beginning 1 November 1998 with a forward look for the year beginning 1 November 1999. CONTENTS CHAIRMAN'S LETTER i-ii 1. THE HUMAN FERTILISATION AND EMBRYOLOGY AUTHORITY THE HFEA'S MEMBERSHIP AND ITS EXECUTIVE 1 QUINQUENNIAL REVIEW 2 PERFORMANCE INDICATORS 2 EFFICIENCY SAVINGS 2 LICENCE FEE REVIEW 2 THE CODE OF PRACTICE ON ENFORCEMENT 3 MEMBERSHIP OF THE HUMAN FERTILISATION AND EMBRYOLOGY AUTHORITY 4 MEMBERSHIP OF HFEA COMMITTEES AND WORKING GROUPS 5 2. LICENSING AND AUDIT OF LICENSED CLINICS INTRODUCTION 6 THE LICENSING AND INSPECTION PROCESS 6 INSPECTION PROTOCOLS 7 BREACHES AND ENFORCEMENT 7 THE AUDIT PROGRAMME OF LICENSED CLINICS' DATA 7 3. THE CODE OF PRACTICE INTRODUCTION 8 WELFARE OF THE CHILD 8 THE FIFTH EDITION OF THE CODE OF PRACTICE 9 REVISION OF CONSENT FORMS 9 4. COLLECTING AND PROVIDING DATA DEVELOPMENT OF THE HFEA'S DATA REGISTER 10 IVF DATA 11 MULTIPLE BIRTHS AND TWO AND THREE EMBRYO TRANSFER 11 DONOR INSEMINATION DATA 12 5. RESEARCH INTRODUCTION 25 LICENSED RESEARCH PROJECTS 26 THE RESEARCH LICENSING PROCESS 26 6. POLICY UPDATE AND ISSUES FOR THE COMING YEAR PREIMPLANTATION GENETIC DIAGNOSIS (PGD) 27 EGG FREEZING 27 CLONING 27 EGG SHARING 28 PAYMENT OF EXPENSES TO DONORS 28 HFEA INFORMATION FOR TREATMENT ETHICS COMMITTEES 28 SCREENING OF SPERM DONORS 28 BULK IMPORT 29 STORAGE OF OVARIAN AND TESTICULAR TISSUE 29 THE STATUTORY STORAGE PERIOD FOR GAMETES AND EMBRYOS 29 MIXED IVF/ICSI EMBRYO TRANSFERS 29 WORKING GROUP ON NEW DEVELOPMENTS IN REPRODUCTIVE TECHNOLOGY 29 7. -

The Evolution of in Vitro Fertilization in the United States: a Closer Look at Media Coverage
THE EVOLUTION OF IN VITRO FERTILIZATION IN THE UNITED STATES: A CLOSER LOOK AT MEDIA COVERAGE Jillian Clair Canada A thesis submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Master of Arts in the School of Journalism and Mass Communication Chapel Hill 2007 Approved by Advisor: Chris Roush Reader: Jan Yopp Reader: Dr. Stan Beyler © 2007 Jillian Clair Canada ALL RIGHTS RESERVED ii ABSTRACT JILLIAN CLAIR CANADA: The Evolution of In Vitro Fertilization in the United States: A Closer Look at Media Coverage (Under the direction of Chris Roush, Jan Yopp and Dr. Stan Beyler) Since the inception of in vitro fertilization in the United States in 1981 the U.S. media have covered its advances, moral debates and oddities. The reproductive technology, which manually combines both egg and sperm to form an embryo outside of a woman’s uterus, sparks the public’s curiosity in many ways – ethically, legally, emotionally and scientifically. Infertility, the disease that IVF overpowers, affects one million women each year. But the media rarely write in-depth articles that give readers and viewers information about the evolution of IVF and the years of trials and error that doctors and patients endured to improve the technique. Nor has the press covered the cost of IVF. That information is important to potential patients and the medical field and the history of research and medical development. This series of three magazine articles fills the information gap and also looks at the media’s response to that gap.