Informed Consent Lasik
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soft Tissue Laser Dentistry and Oral Surgery Peter Vitruk, Phd
Soft Tissue Laser Dentistry and Oral Surgery Peter Vitruk, PhD Introduction The “sound scientific basis and proven efficacy in order to ensure public safety” is one of the main eligibility requirements of the ADA CERP Recognition Standards and Procedures [1]. The outdated Laser Dentistry Curriculum Guidelines [2] from early 1990s is in need of an upgrade with respect to several important laser-tissue interaction concepts such as Absorption Spectra and Hot Glass Tip. This position statement of The American Board of Laser Surgery (ABLS) on soft tissue dentistry and oral surgery is written and approved by the ABLS’s Board of Directors. It focuses on soft tissue ablation and coagulation science as it relates to both (1) photo-thermal laser-tissue interaction, and (2) thermo-mechanical interaction of the hot glass tip with the tissue. Laser Wavelengths and Soft Tissue Chromophores Currently, the lasers that are practically available to clinical dentistry operate in three regions of the electromagnetic spectrum: near-infrared (near-IR) around 1,000 nm, i.e. diode lasers at 808, 810, 940, 970, 980, and 1,064 nm and Nd:YAG laser at 1,064 nm; mid-infrared (mid-IR) around 3,000 nm, i.e. erbium lasers at 2,780 nm and 2,940 nm; and infrared (IR) around 10,000 nm, i.e. CO2 lasers at 9,300 and 10,600 nm. The primary chromophores for ablation and coagulation of oral soft tissue are hemoglobin, oxyhemoglobin, melanin, and water [3]. These four chromophores are also distributed spatially within oral tissue. Water and melanin, for example, reside in the 100-300 µm-thick epithelium [4], while water, hemoglobin, and oxyhemoglobin reside in sub-epithelium (lamina propria and submucosa) [5], as illustrated in Figure 1. -
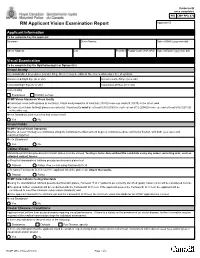
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Early Postoperative Rotational Stability and Its Related Factors of a Single-Piece Acrylic Toric Intraocular Lens
Eye (2020) 34:474–479 https://doi.org/10.1038/s41433-019-0521-0 ARTICLE Early Postoperative Rotational stability and its related factors of a single-piece acrylic toric intraocular lens 1,2 3 4 5 1 1 1 Shuyi Li ● Xi Li ● Suhong He ● Qianyin Zheng ● Xiang Chen ● Xingdi Wu ● Wen Xu Received: 30 November 2018 / Accepted: 18 June 2019 / Published online: 12 July 2019 © The Author(s) 2019. This article is published with open access Abstract Purpose In the present study, we aimed to evaluate the early postoperative rotational stability of TECNIS toric intraocular lens (IOL) and analyse its correlation with preoperative and intraoperative parameters. Methods A total of 102 eyes from 87 cataract patients who underwent implantation of TECNIS toric IOL during July 2016 to November 2017 were enrolled in this retrospective study. Preoperative parameters including corneal astigmatism, axial length (AL), lens thickness (LT), anterior chamber depth (ACD) and sulcus-to-sulcus (STS), were determined. The area of capsulorhexis was measured with Rhinoceros 5.0 software. The follow-up examinations including the residual astigmatism (RAS) and postoperative toric IOL axis, were performed at 1 month and 3 months after surgery. − − 1234567890();,: 1234567890();,: Results RAS was 0.84 ± 0.88 D at 1 month and 0.81 ± 0.89 D at 3 months after surgery. The rotation of toric IOL at 3 months was 4.83 ± 3.65°. The Pearson’s r of ACD, horizontal and vertical STS, and toric IOL target axis was 0.011, 0.039, 0.045 and 0.082. The toric IOL rotation was positively correlated with the area of capsulorhexis (r = 0.522, P = 0.0003), LT (r = 0.288, P = 0.003) and AL (r = 0.259, P = 0.009). -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Cutaneous Laser Surgery
Cutaneous Laser Surgery Vineet Mishra, M.D. Director of Mohs Surgery & Procedural Dermatology Assistant Professor of Dermatology University of Texas Health Science Center – San Antonio Visible-Infrared Range What does it stand for? LASER 3 Components: – L Light – Pumping system – A Amplification . Energy source/power supply – S Stimulated – Lasing medium – E Emission – Optical cavity – R Radiation Lasing Medium Supplies electrons for the stimulated emission of radiation Determines wavelength of laser – Expressed in nm 3 Mediums: – Gaseous (CO2, argon, copper vapor) – Solid (diode, ruby, Neodymium:Yag) – Liquid (tunable dye, pulse dye) Laser vs. IPL LASER – coherent, monochromatic light IPL = intense pulsed light – non coherent light – 515‐1000nm Monochromatc Laser light is a single color – color = specific wavelength of each laser Wavelength Wavelength determines – Chromophore specificity . Chromophore = tissue target that absorbs a specific wavelength of light – Depth pulse travels Chromophore & Absorption Spectra Chromophore/Target Wavelength Abs. Spectra – Hemoglobin – Blue-green and yellow light – DNA, RNA, protein – UV light – Melanin – Ultraviolet > Visible >> near IR – Black ink tattoo – Visible and IR – Water – IR Absorption Curves Terms to Know Energy – Joules, the capacity to do work Power – Rate of energy delivery (Watts = J/sec) Fluence – Energy density (J/cm2) Thermal Relaxation Time (TRT) – time required for an object to lose 50% of its absorbed heat (cooling time) to surrounding tissues Thermal Relaxation Time Thermal Relaxation Time (TRT) – time required for an object to lose 50% of its absorbed heat (cooling time) to surrounding tissues – directly proportional to size of an object (proportional to square of its size) – smaller objects cool faster (shorter TRT) than larger ones (longer TRT) Selective Photothermolysis by Anderson and Parrish (Science, 1983) Selective Photothermolysis – Thermocoagulation of specific tissue target with minimum damage to surrounding tissue Requirements: – 1. -

Medical Treatment of Operative Corneal Perforation Caused By
CASE REPORTS AND SMALL CASE SERIES and clinical course of a patient with the stromal bed was thin; in the left Medical Treatment a LASIK-induced corneal perfora- eye, the corneal flap was very edema- of Operative Corneal tion that affected the final visual acu- tous and a space was visible between Perforation Caused ity. We believe that this report on the the corneal flap and the stromal bed treatment and recovery of the cor- (Figure 1, left). The anterior cham- by Laser In Situ neal perforation will be valuable in- ber was very shallow, and aqueous Keratomileusis formation for refractive surgeons. humor was observed to leak onto the ocular surface with blinking (Figure Laser in situ keratomileusis (LASIK) Report of a Case. A 33-year-old man 1, right). A round, 0.25-mm diam- is an effective procedure to treat a was referred to us with a complaint eter perforation site was observed in wide range of myopia.1 The advan- of decreased visual acuity in the left the center of the stromal bed by slit- tages of LASIK over photorefrac- eye after bilateral simultaneous lamp examination. tive keratectomy (PRK) are rapid vi- LASIK performed 3 days previ- We treated the corneal perfo- sual recovery, lower risk of corneal ously at a different facility. A cor- ration by applying a therapeutic soft haze, greater regression of myopia, neal perforation was noticed in the contact lens with topical antibiot- and less postoperative pain.1-3 How- left eye during LASIK laser abla- ics, oral carbonic anhydrase inhibi- ever, LASIK requires more skillful tion in this eye. -

Experts Describe the Gold Standard in Medical
Christopher Zachary, MBBS, FRCP Experts describe the gold standard in Professor and Chair Department of Dermatology medical and aesthetic laser therapy, University of California-Irvine sharing their experiences using clinically- effective, time-proven technologies. asers have without question revolutionized the practice Expanding the Level of Service and ® of dermatology, permitting clinicians to treat conditions Patient Satisfaction with Gemini for which no medical therapies exist or offering results Efficient Management of Rosacea and Photodamage that exceed those of conventional therapeutics. From with the Gemini Laser medical conditions like acne and rosacea to cosmetic Lrejuvenation, laser systems can address a variety of the most Photorejuvenation in Asian Skin Tones: common presentations that bring patients to the dermatolo- Role of the Gemini Laser gist’s office. Gemini for Photorejuvenation: Given their remarkable utility, well-designed and manufac- A Cornerstone of the Cosmetic Practice tured lasers can be a tremendous asset to dermatologists. Yet, often physicians are overwhelmed by the prospect of incorpo- Targeting Patients’ Aesthetic Goals with the VariLite™ rating laser procedures into practice. Technology is costly, and there may be a tremendous sense of pressure to attract The VariLite for Fundamental Cosmetic Applications patients and, as important, provide treatment that meets their VariLite: A Reliable, Predictable Tool for Vascular and goals. There may also be a learning curve, as residency pro- Pigmented Lesions grams currently offer little training in aesthetic dermatology, Continued on page 3 Expert Contributors William Baugh, MD C. William Hanke, MD, MPH Assistant Clinical Professor, Visiting Professor of Dermatology, Western School of Medicine University of Iowa, Carver College of Medicine Medical Director Clinical Professor of Otolaryngology Head and Full Spectrum Dermatology, Neck Surgery, Fullerton, CA Indiana University School of Medicine Carmel, IN Henry H. -

A Practical Comparison of Ipls and the Copper Bromide Laser for Photorejuvenation, Acne and the Treatment of Vascular & Pigmented Lesions
A practical comparison of IPLs and the Copper Bromide Laser for photorejuvenation, acne and the treatment of vascular & pigmented lesions. Authors: Peter Davis, Adelaide, Australia, Godfrey Town, Laser Protection Adviser, Haywards Heath, United Kingdom Abstract: The recent rapid growth in demand for non-invasive light-based cosmetic treatments such as removal of unwanted facial and body hair, skin rejuvenation, removal of age-related and sun induced blemishes including pigment and vascular lesions as well as lines and wrinkles has led to a boom in the sale of medical devices that claim to treat these conditions. The often onerous safety regulations governing the sale and use of Class 4 lasers has contributed disproportionately to the popularity of similarly powerful non-laser Intense Pulse Light sources (“IPL”), particularly in the salon and spa sector. The practical science-based comparisons made in this review and the well- documented case studies in peer reviewed literature show that single treatment success in eradicating vascular and pigmented lesions may only be achieved by high fluence, wavelength-specific laser treatment and without the need for skin cooling. Introduction: hair removal with IPL The recent success of IPL in delaying hair re-growth (“hair management”) and permanent hair reduction (“photo-waxing”) is dependant upon using high energy settings for the former and is thought to work primarily because melanin absorbs energy across a wide spectrum of wavelengths. Cumulatively enough energy is absorbed to damage the hair follicle. It is also suggested that the longer wavelengths absorbed by blood and tissue water may also collectively damage hair follicle support structures such as the blood supply to the hair bulb aided by the overall temperature rise in the adjacent tissue. -

Evaluating the Relation of Refractive Surgery and Glaucoma
Editorial Remedy Open Access Published: 25 Jul, 2017 Evaluating the Relation of Refractive Surgery and Glaucoma Kozobolis V*, Kostantinidis A and Labiris G Department of Ophthalmology, University of Thrace, Greece Editorial Laser-assisted refractive corrections constitute a large part of the ophthalmic surgeries that take place every year. It is estimated that about 4 million refractive procedures were performed in 2014 throughout the world. On the other hand, glaucoma is an optic neuropathy, the incidence of which is increasing steadily over time. Given the frequency of refractive surgeries and the incidence of glaucoma in the general population it becomes necessary for the ophthalmologist to assess the risks of a refractive surgery in a glaucoma patient or a patient at a risk of developing glaucoma in the future. The factors to take into consideration are: the family history of glaucoma, intraocular pressure (IOP), myopia, high vertical cup-to-disc ratio, central corneal thickness, and race, other ophthalmic diseases, hypermetropia, previous antiglaucoma procedure, visual fields and modern imaging modalities. The advantages of these modalities include objective and reproducible measurements that can be compared with future measurements. The disadvantage is that their databases (although constantly enriched) include limited number of people, while "unusual" discs (tilted, high ametropias) are excluded from the databases. Unfortunately many candidates for refractive surgery have optic discs with “unusual” appearance that cannot be meaningfully compared with the “normal” optic discs of the databases. In these cases the digital photographing of the optic disc and the comparison with future photos will give valuable information about the changes of both the optic nerve and retinal nerve fibers. -

Vitreoretinal Surgery for Macular Hole After Laser Assisted in Situ
1423 Br J Ophthalmol: first published as 10.1136/bjo.2005.074542 on 18 October 2005. Downloaded from SCIENTIFIC REPORT Vitreoretinal surgery for macular hole after laser assisted in situ keratomileusis for the correction of myopia J F Arevalo, F J Rodriguez, J L Rosales-Meneses, A Dessouki, C K Chan, R A Mittra, J M Ruiz- Moreno ............................................................................................................................... Br J Ophthalmol 2005;89:1423–1426. doi: 10.1136/bjo.2005.074542 macular hole between March 1996 and March 2003 at seven Ams: To describe the characteristics and surgical outcomes institutions in Venezuela, Colombia, Spain, and the United of full thickness macular hole surgery after laser assisted in States. Preoperative examination including a thorough situ keratomileusis (LASIK) for the correction of myopia. dilated funduscopy with indirect ophthalmoscopy, and slit Methods: 13 patients (14 eyes) who developed a macular lamp biomicroscopy was performed by a retina specialist and/ hole after bilateral LASIK for the correction of myopia or a refractive surgeon. Patients were female in 60.7% of participated in the study. cases, and underwent surgical correction of myopia ranging Results: Macular hole formed 1–83 months after LASIK from 20.75 to 229.00 dioptres (D) (mean 26.19 D). Patients (mean 13 months). 11 out of 13 (84.6%) patients were were followed for a mean of 65 months after LASIK (range female. Mean age was 45.5 years old (25–65). All eyes 6–84 months). Patients who underwent vitreoretinal surgery were myopic (range 20.50 to 219.75 dioptres (D); mean to repair the macular hole were included in the study 28.4 D). -

Second Harmonic Generation Microscopy: a Tool for Quantitative Analysis of Tissues
Chapter 5 Second Harmonic Generation Microscopy: A Tool for Quantitative Analysis of Tissues Juan M. Bueno, Francisco J. Ávila, and Pablo Artal Additional information is available at the end of the chapter http://dx.doi.org/10.5772/63493 Abstract Second harmonic generation (SHG) is a second‐order non‐linear optical process produced in birefringent crystals or in biological tissues with non‐centrosymmetric structure such as collagen or microtubules structures. SHG signal originates from two excitation photons which interact with the material and are “reconverted” to form a new emitted photon with half of wavelength. Although theoretically predicted by Maria Göpert‐Mayer in 1930s, the experimental SHG demonstration arrived with the invention of the laser in the 1960s. SHG was first obtained in ruby by using a high excitation oscillator. After that starting point, the harmonic generation reached an increasing interest and importance, based on its applications to characterize biological tissues using multiphoton microscopes. In particular, collagen has been one of the most often analyzed structures since it provides an efficient SHG signal. In late 1970s, it was discovered that SHG signal took place in three‐dimensional optical interaction at the focal point of a microscope objective with high numerical aperture. This finding allowed researchers to develop microscopes with 3D submicron resolution and an in depth analysis of biological specimens. Since SHG is a polarization‐sensitive non‐linear optical process, the implementation of polarization into multiphoton microscopes has allowed the study of both molecular architecture and fibrilar distribution of type‐I collagen fibers. The analysis of collagen‐based structures is particularly interesting since they represent 80% of the connective tissue of the human body.