Electronic Medical Record in the Simulation Hospital: Does It Improve Accuracy in Charting Vital Signs, Intake, and Output? Carel M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Licensed Practical Nurse
HEALTH CAREER INFORMATION SHEETS Licensed Practical Nurse Professional Activities Licensed practical nurses (LPNs), or licensed vocational nurses (LVNs), care for people who are sick, injured, convalescent, or disabled under the direction of physicians and registered nurses. LPNs care for patients in many ways. Often, they provide basic bedside care. Many LPNs measure and record patients' vital signs such as height, weight, temperature, blood pressure, pulse, and respiration. They also prepare and give injections and enemas, monitor catheters, dress wounds, and give alcohol rubs and massages. As part of their work, LPNs collect samples for testing, perform routine laboratory tests, and record food and fluid intake and output. They clean and monitor medical equipment. Sometimes, they help physicians and registered nurses perform tests and procedures. Some LPNs help to deliver, care for, and feed infants. LPNs also monitor their patients and report adverse reactions to medications or treatments. LPNs gather information from patients, including their health history and how they are currently feeling. They may use this information to complete insurance forms, pre-authorizations, and referrals, and they share information with registered nurses and doctors to help determine the best course of care for a patient. LPNs often teach family members how to care for a relative or teach patients about good health habits. Most LPNs are generalists and will work in any area of healthcare. However, some work in a specialized setting, such as a nursing home, a doctor's office, or in home healthcare. LPNs in nursing care facilities help to evaluate residents' needs, develop care plans, and supervise the care provided by nursing aides. -

Creating a Successful Transcultural On-Boarding Program
JOURNAL FOR NURSES IN STAFF DEVELOPMENT Volume 25, Number 5, 222–226 Copyright A 2009 Wolters Kluwer Health | Lippincott Williams & Wilkins . A diverse workforce enables an . organization to reflect and respond to . Creating a Successful community diversity. With an increase in . the number of nurses educated outside of . the United States seeking licensure and . Transcultural employment within U.S. hospitals, the . development of an approach to assimilate . On-Boarding Program these international nurses is essential. A . thorough and holistic approach will ensure . Beth Nease, MSN, RN, BC an ethical and safe introduction into the U.S. nursing workforce. This article describes a . program based on the hospital’s nursing . professional practice model that was . developed to address the challenges of skill . transfer, role definition, and communication. ................................................. atient safety requires a qualified and committed care. Working to mirror the population served by Pnursing staff competent in skill and effective in providing a healthcare team reflective of the commu- communication. A transcultural on-boarding program nity can be an effective strategy for meeting the needs based on the hospital’s nursing professional practice of the increasing diversity seen in U.S. hospitals. Mutha model was developed to address the challenges of skill and Karliner (2006) defined culturally competent care transfer, role definition, and communication. On- as ‘‘the ability to deliver effective medical care to pa- boarding provides a focus on complete integration tients regardless of culture or language differences and assimilation of newly hired employees. On- between them and their provider’’ (p. 47). Further- boarding includes all processes and activities related more, Mutha and Karliner defined culture as the lens to new staff, including the recruitment and selection through which we view and organize an understand- process. -

Nursing Students' Perspectives on Telenursing in Patient Care After
Clinical Simulation in Nursing (2015) 11, 244-250 www.elsevier.com/locate/ecsn Featured Article Nursing Students’ Perspectives on Telenursing in Patient Care After Simulation Inger Ase Reierson, RN, MNSca,*, Hilde Solli, RN, MNSc, CCNa, Ida Torunn Bjørk, RN, MNSc, Dr.polit.a,b aFaculty of Health and Social Studies, Institute of Health Studies, Telemark University College, 3901 Porsgrunn, Norway bFaculty of Medicine, Institute of Health and Society, Department of Nursing Science, University of Oslo, 0318 Oslo, Norway KEYWORDS Abstract telenursing; Background: This article presents the perspectives of undergraduate nursing students on telenursing simulation; in patient care after simulating three telenursing scenarios using real-time video and audio nursing education; technology. information and Methods: An exploratory design using focus group interviews was performed; data were analyzed us- communication ing qualitative content analysis. technology; Results: Five main categories arose: learning a different nursing role, influence on nursing assessment qualitative content and decision making, reflections on the quality of remote comforting and care, empowering the pa- analysis tient, and ethical and economic reflections. Conclusions: Delivering telenursing care was regarded as important yet complex activity. Telenursing simulation should be integrated into undergraduate nursing education. Cite this article: Reierson, I. A., Solli, H., & Bjørk, I. T. (2015, April). Nursing students’ perspectives on telenursing in patient care after simulation. Clinical Simulation in Nursing, 11(4), 244-250. http://dx.doi.org/ 10.1016/j.ecns.2015.02.003. Ó 2015 International Nursing Association for Clinical Simulation and Learning. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/ by-nc-nd/4.0/). -
Msc Nursing SYLLABUS.Pdf
Syllabus for Courses affiliated to the Kerala University of Health Sciences Thrissur 680596 2016 MASTER OF SCIENCE IN NURSING Medical Surgical Nursing Course Code 271 (2016‐17 admission onwards) 2016 REGULATIONS 2. COURSE CONTENT 2.1 Title of course: MASTER OF SCIENCE IN NURSING – MSc Medical Surgical Nursing Sub specialties :‐ a. Cardio Vascular & Thoracic Nursing b. Critical care Nursing, Oncology Nursing c. Neurosciences Nursing d. Nephro‐Urology Nursing e. Orthopedic Nursing f. GastroEnterology Nursing. 2.2 AIM & OBJECTIVES OF THE COURSE AIM Aim of the postgraduate programme in nursing is to prepare graduates to assume responsibilities as Clinical Nurse Specialists, Nurse Practitioners, Consultants, Educators, Researchers and Administrators in a wide variety of professional settings. OBJECTIVES On completion of the 2 year M.Sc Nursing programme, the graduates will be able to:‐ 1. Apply the concepts, theories and principles of nursing science. 2. Demonstrate competencies in nursing practice. 3. Practice as Clinical Nurse Specialist. 4. Establish collaborative relationship with the members of other disciplines. 5. Assume leadership in various care settings. 6. Participate in health planning, implementation and evaluation at different levels of health care system. 7. Function as effective nurse educators and nurse managers. 8. Conduct independent nursing research and utilize the research findings in nursing practice and education. 1 9. Critically evaluate various educational programmes in nursing. 10. Demonstrate interest and positive attitude in continuing education for personal and professional growth. 11. Demonstrate advanced skills and competence in the nursing management of patients with various medical and surgical conditions. 12. Incorporate evidence based nursing practice and identify the areas of research in the field of medical and surgical nursing. -
Nurse Educators' Consensus Opinion on Using an Academic Electronic Health Record: a Delphi Study Darlene S
University of North Dakota UND Scholarly Commons Theses and Dissertations Theses, Dissertations, and Senior Projects January 2013 Nurse Educators' Consensus Opinion On Using An Academic Electronic Health Record: A Delphi Study Darlene S. Hanson Follow this and additional works at: https://commons.und.edu/theses Recommended Citation Hanson, Darlene S., "Nurse Educators' Consensus Opinion On Using An Academic Electronic Health Record: A Delphi Study" (2013). Theses and Dissertations. 1429. https://commons.und.edu/theses/1429 This Dissertation is brought to you for free and open access by the Theses, Dissertations, and Senior Projects at UND Scholarly Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. NURSE EDUCATORS’ CONSENSUS OPINION ON USING AN ACADEMIC ELECTRONIC HEALTH RECORD: A DELPHI STUDY by Darlene S. Hanson Bachelor of Science, Minot State University, 1978 Master of Science, University of North Dakota, 1987 A Dissertation Submitted to the Graduate Faculty of the University of North Dakota In partial fulfillment of the requirements for the degree of Doctor of Philosophy Grand Forks, North Dakota August 2013 Copyright 2013 Darlene S. Hanson ii This dissertation, submitted by Darlene S. Hanson, in partial fulfillment of the requirements for the Degree of Doctor of Philosophy from the University of North Dakota, has been read by the Faculty Advisory Committee under whom the work has been done, and is hereby approved. ____________________________________ Dr, Myrna R. Olson, Chair ____________________________________ Dr. Margaret Zidon ____________________________________ Dr. Kathy Smart ____________________________________ Dr. Steven D. LeMire This dissertation is being submitted by the appointed advisory committee as having met all of the requirements of the Graduate School at the University of North Dakota and is hereby approved. -

Care of the Pediatric Patient in Surgery: Neonatal Through Adolescence ”
CARE OF THE PEDIATRIC PATIENT IN SURGERY : NEONATAL THROUGH ADOLESCENCE 1961 1961 CARE OF THE PEDIATRIC PATIENT IN SURGERY : NEONATAL THROUGH ADOLESCENCE STUDY GUIDE Disclaimer AORN and its logo are registered trademarks of AORN, Inc. AORN does not endorse any commercial company’s products or services. Although all commercial products in this course are expected to conform to professional medical/nursing standards, inclusion in this course does not constitute a guarantee or endorsement by AORN of the quality or value of such products or of the claims made by the manufacturers. No responsibility is assumed by AORN, Inc, for any injury and/or damage to persons or property as a matter of product liability, negligence or otherwise, or from any use or operation of any standards, recommended practices, methods, products, instructions, or ideas contained in the material herein. Because of rapid advances in the health care sciences in particular, independent verification of diagnoses, medication dosages, and individualized care and treatment should be made. The material contained herein is not intended to be a substitute for the exercise of professional medical or nursing judgment. The content in this publication is provided on an “as is” basis. TO THE FULLEST EXTENT PERMITTED BY LAW, AORN, INC, DISCLAIMS ALL WARRANTIES, EITHER EXPRESSED OR IMPLIED, STATUTORY OR OTHERWISE, INCLUDING BUT NOT LIMITED TO THE IMPLIED WARRANTIES OF MERCHANTABILITY, NON-INFRINGEMENT OF THIRD PARTIES’ RIGHTS, AND FITNESS FOR A PARTICULAR PURPOSE. This publication may be photocopied for noncommercial purposes of scientific use or educational advancement. The following credit line must appear on the front page of the photocopied document: Reprinted with permission from The Association of periOperative Registered Nurses, Inc. -

Nurse Education Graduates
NURSE EDUCATION GRADUATES CLASS OF 2020 THE PINNING CEREMONY 2020 Graduates The pin is a tradition in nursing. Every school of nursing Marie Andrews Alyssa Hall has its unique pin. Frequently, the pin embodies the Samantha Bahantka Carissa Hamilton school seal, and some, like SUNY Corning Community College, Vanessa Barnes Ryleigh Hancock incorporate the school colors. Erica Barrett Jessica Hand Sinead Bond Shannon Havens The book and lamp of knowledge were to represent Ashley Boyer Cassandra Hayes the educational foundation on which the “new” associate Sarah Braveman Samantha Held degree nursing programs were to be based. Melanie Cartegena Raymond Homolka Taylor Crawford Emily Houghtaling The scroll, quill, and ink bottle, which were to represent Alyssa Crout Natalie Hughes Florence Nightingale’s Notes on Nursing, should be the Amanda Denson Yasmin Hussain basis for the nursing education portion of the curriculum. Stephanie Deubler Anthony Malmquist Adam DuBois Daniel Mantz Lydia Fillmore Cassandra Miller Kristina Foglia Tyler Morehouse Meredith Foster Nicole Jayne Hannah Fox Emily Jerzak Diane Frampton Cheyenne Kepner Diane Galbraith Emilee Knapp Kristine Gessner Melissa Krause Shaylene Graves Sara Kuhnel 2020 Graduates CLASS OF 2020 NURSING SOCIETY OFFICERS Gretchen Larrison Katherine Rominger Erika Lewis Faith Scalia Marie Andrews, President Lindsey Putney, Vice-President Virginia Livermore-Johnson Ann Scott Adam DuBois, Secretary Kristi Manuilow Corin Smith Hillary Millard, Treasurer Tari McCallum Kayla Smith John Tucker, Senator Alice McDonald Samantha Snyder AWARD RECIPIENTS Brian McLinko Samantha Taylor Academic Excellence Carissa Miller Rachel Thurston Kristina E. Foglia Crystal Miller Simone Trimble Matthew Miller Christopher Vanderpoel Clinical Excellence Brian J. McLinko Hillary Millerd Tanya Vennel Shannon Nugent Jennifer Wattles Pauline J. -

Failure to Complete BSN Nursing Programs: Students' Views
101 Failure to Complete BSN Nursing Programs: Students’ Views Nancy Elkins, Marshall University Abstract This phenomenological research study investigated the lived experiences of students who did not succeed in completing a 4-year baccalaureate nursing school (BSN) program. The sample for this study included students who failed to completed baccalaureate nursing programs within the last ten years. The geographical area of the sample included students who attended schools in the central and south-western Appalachian counties of the state of West Virginia and the bordering counties in Ohio, Kentucky, and Virginia. A total of 18 participants were interviewed and the interviews were recorded so the data would be collected in a systematic way to facilitate data analysis. There is little empirical data regarding retention in a BSN program and students’ views as to why they were unable to complete their BSN program. Further research is needed to understand nursing student attrition, especially students’ perceptions, which would help nurse educators identify nursing students’ needs, review program’s policies, and possible curriculum changes needed to help students successfully complete their nursing program. Keywords: Nursing Education, Persistence, Student Perceptions and Motivations Introduction A nursing shortage has been predicted in the United States due to the aging nursing workforce and the future needs of the baby-boomers as they age. The Government Affairs Committee of the American Nurses Association (ANA) predict that by 2022 that the United States will need to produce more than one million additional nurses to fill both new nursing jobs and replace the wave of retiring nurses. The premise of this study is that if we better understood why students fail nursing schools, faculty could support program or policy changes, or initiate admission procedures that would better predict student success in baccalaureate nursing programs; thereby, the predicted nursing shortage could be mitigated. -
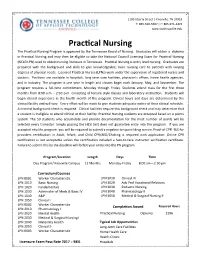
Practical Nursing the Practical Nursing Program Is Approved by the Tennessee Board of Nursing
1100 Liberty Street | Knoxville, TN 37919 T: 865-546-5567 | F: 865-971-4474 www.tcatknoxville.edu Practical Nursing The Practical Nursing Program is approved by the Tennessee Board of Nursing. Graduates will obtain a diploma in Practical Nursing and may then be eligible to take the National Council Licensing Exam for Practical Nursing (NCLEX-PN) used to obtain nursing licensure in Tennessee. Practical Nursing is entry level nursing. Graduates are prepared with the background and skills to give knowledgeable, basic nursing care to patients with varying degrees of physical needs. Licensed Practical Nurses (LPNs) work under the supervision of registered nurses and doctors. Positions are available in hospitals, long term care facilities, physician's offices, home health agencies, and in industry. The program is one year in length and classes begin each January, May, and September. The program requires a full-time commitment, Monday through Friday. Students attend class for the first three months from 8:00 a.m. - 2:30 p.m. consisting of lecture style classes and laboratory instruction. Students will begin clinical experience in the fourth month of the program. Clinical hours and days are determined by the clinical facility and will vary. Every effort will be made to give students adequate notice of their clinical schedule. A criminal background check is required. Clinical facilities require this background check and may determine that a student is ineligible to attend clinical at their facility. Practical Nursing students are accepted based on a points system. The 50 students who accumulate and provide documentation for the most number of points will be selected every trimester. -

Role Development of the CRNA Clinical Educator Utilizing an On-Line Resource
St. Catherine University SOPHIA Doctor of Nursing Practice Projects Nursing 5-2013 Role Development of the CRNA Clinical Educator Utilizing an On- Line Resource Ann Bernice Sullivan St. Catherine University Follow this and additional works at: https://sophia.stkate.edu/dnp_projects Recommended Citation Sullivan, Ann Bernice. (2013). Role Development of the CRNA Clinical Educator Utilizing an On-Line Resource. Retrieved from Sophia, the St. Catherine University repository website: https://sophia.stkate.edu/dnp_projects/36 This Doctor of Nursing Practice Project is brought to you for free and open access by the Nursing at SOPHIA. It has been accepted for inclusion in Doctor of Nursing Practice Projects by an authorized administrator of SOPHIA. For more information, please contact [email protected]. Role Development of the CRNA Clinical Educator Utilizing an On-Line Resource Systems Change Project Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Nursing Practice St. Catherine University St. Paul, Minnesota Ann Bernice Sullivan March 2013 i Role Development of the CRNA Clinical Educator Utilizing an On-line Resource ST. CATHERINE UNIVERSITY ST. PAUL, MINNESOTA This is to certify that I have examined this Doctor of Nursing Practice systems change project written by Ann Bernice Sullivan And have found that it is complete and satisfactory in all respects, and that any and all revisions required by the final examining committee have been made. Graduate Program Faculty Name of Faculty Project Advisor __________________5/20/13__________________ Date DEPARTMENT OF NURSING ii Role Development of the CRNA Clinical Educator Utilizing an On-line Resource © Ann Bernice Sullivan March 2013 All Rights Reserved iii Role Development of the CRNA Clinical Educator Utilizing an On-line Resource Executive Summary Clinical education is an essential component of nurse anesthesia education. -

Overview of Pediatric Nursing Care
© Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR UNITSALE OR I DISTRIBUTION NOT FOR SALE OR DISTRIBUTION Overview© Jonesof & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC PediatricNOT Nursing FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION Care© Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION © Rawpixel.com/Shutterstock NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC CHAPTER 1 NOTIntroduction FOR SALE ORto Children’sDISTRIBUTION Health Care NOT FOR SALE OR DISTRIBUTION CHAPTER 2 Care Across Clinical Settings © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC. NOT FOR SALE OR DISTRIBUTION. 9781284375473_CH01_001_013.indd 1 06/07/17 2:03 PM © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, -

New Technology in Nursing Education and Practice
IOSR Journal of Nursing and Health Science (IOSR-JNHS) e-ISSN: 2320–1959.p- ISSN: 2320–1940 Volume 6, Issue 6 Ver. I. (Nov. Dec .2017), PP 29-38 www.iosrjournals.org New Technology in Nursing Education and Practice Ragaa Gasim Ahmed Mohmmed1, Hanan Mohammed Mohammed2,4, Abeer El-Said Hassane El-sol3,4 1 (Assistant professor of Pediatric Nursing, Faculty of Applied Medical Sciences, Nursing Department, Al-Baha University, Saudi – Arabia) 2 (Assistant Professor of Medical-Surgical Nursing Department, Faculty of Nursing, Ain Shams University, Egypt) 3 (Lecturer of Medical-Surgical Nursing, Medical Surgical Department, Faculty of Nursing, Shibin Elkom, Menoufia University, Egypt) 4 (Faculty of Applied Medical Sciences, Nursing Department, Al-Baha University, Saudi – Arabia) Ragaa Gasim Ahmed Mohmmed Corresponding Author: [email protected] Abstract: Technology is changing the world at warp speed and nowhere is this clearer than in health care settings. In an increasingly crowded world, people rightly expect health care to meet their needs quickly and, where possible, tailored to their needs. Technology helps to deliver these elements, putting the power back in the hands of the patient. Health care is growing increasingly complex, and most clinical research focuses on new approaches to diagnosis and treatment. In contrast, relatively little effort has been targeted at the perfection of operational systems, which are partly responsible for the well-documented problems with medical safety. If medicine is to achieve major gains in quality, it must be transformed, and information technology will play a key part, especially with respect to safety. Technological innovation in health care is an important driver of cost growth.