Health Care Reform Review Committee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SUGGESTED 2017-18 LEGISLATIVE INTERIM COMMITTEES with LEGISLATOR PREFERENCES COMMITTEE WORKING DOCUMENT All Choices
June 13, 2017 11:00 a.m. SUGGESTED 2017-18 LEGISLATIVE INTERIM COMMITTEES WITH LEGISLATOR PREFERENCES COMMITTEE WORKING DOCUMENT All Choices Administrative Rules R Representative Greg Westlind 4 (1 From Each House or Senate Standing Committee) R Representative Randy Boehning 1 Budget Section R Representative Bill Devlin 1 Membership consists of leadership R Representative Kim Koppelman 1 R Representative Larry Bellew R Representative Scott Louser 1 R Representative Randy Boehning R Representative Jay Seibel 1 R Representative Roger Brabandt D Senator Joan Heckaman 1 R Representative Mike Brandenburg R Representative Nathan Toman 2 R Representative Al Carlson R Representative Robin Weisz 2 R Representative Jeff Delzer R Representative Brandy Pyle 3 R Representative Tom Kading D Representative Joshua Boschee 3 R Representative Keith Kempenich R Senator Kelly Armstrong 3 R Senator Jerry Klein 3 R Representative Gary Kreidt R Senator Nicole Poolman 4 R Representative Bob Martinson D Representative Mary Schneider R Representative Lisa Meier R Senator Howard Anderson R Representative David Monson R Senator Ralph Kilzer R Representative Mike Nathe R Senator Scott Meyer R Representative Jon Nelson R Senator David Rust R Representative Chet Pollert 18 Members R Representative Mark Sanford 15 Republicans 3 Democrats R Representative Mike Schatz R Representative Ben Koppelman 2 R Representative Jim Schmidt R Representative Karen Rohr 4 R Representative Roscoe Streyle R Representative Gary Sukut 4 R Representative Donald Vigesaa D Representative -

House of Rep Daily Journal
Page 1 1st DAY MONDAY, DECEMBER 3, 2018 1 Organizational and Orientation Session December 3, 4, 5, 2018 JOURNAL OF THE HOUSE Sixty-sixth Legislative Assembly * * * * * Bismarck, December 3, 2018 The House convened at 1:00 p.m., with Speaker Bellew presiding. The prayer was offered by Rev. Rich Wyatt, Living Hope Church of the Nazarene, Bismarck. COMMUNICATION FROM SECRETARY OF STATE ALVIN A. JAEGER December 3, 2018 In accordance with Section 54-03-03 of the North Dakota Century Code, I certify the enclosed list is a true and correct record of members of the House of Representatives elected in the General Election held on November 6, 2018. The State Canvassing Board certified the results of the election on November 16, 2018. As specified in Section 16.1-15-45 of the North Dakota Century Code, Certificates of Election were then prepared by the Secretary of State and signed by the Governor, the Clerk of the Supreme Court (as the designated representative of the State Canvassing Board), and the Secretary of State. Each newly elected member of the Legislative Assembly was then issued their Certificate of Election (copies enclosed), as specified in Section 16.1-15-46 of the North Dakota Century Code. In addition, in accordance with Section 4, Article XI, of the North Dakota Constitution, an Oath of Office (or affirmation) form was provided to each Representative, with instructions to execute the Oath before a Notary Public and file it with the Secretary of State before he or she assumes the duties of their office. IN TESTIMONY WHEREOF, I have set my hand and affixed the Great Seal of the State of North Dakota at the Capitol in the City of Bismarck on this date. -

Northern Sights Newsletter
Northern Sights Newsletter North Dakota Vol. 30 Issue 4 August 2018 Optometric Association President’s Message ~ Dr. Darin Johnson 921 South 9th Street, Ste. 120 Bismarck, ND 58504 Phone: 701-258-6766 Wow, summer is Secondly, we are working on the health Fax: 701-258-9005 flying by. I hope eve- care trust. This could be a great option for E-mail: [email protected] ryone has had the our members to have a potential cost saving Website: www.ndeyecare.com opportunity to get out alternative for reliable health insurance. and enjoy the beauti- Nancy has been working hard to make sure 2018 NDOA OFFICERS ful North Dakota we can offer this benefit, and keep it afforda- Dr. Darin Johnson weather. I feel as if ble for our members and their employees. time is slipping by, President Lastly, I am working on a more consistent and I have not accom- 1525 31st Ave. SW, Ste. E and repeatable sponsorship form. There is plished much for the Minot, ND 58701 some stress about our questionable future of NDOA this summer, 701-857-6050 sponsorship, and support from members in but we have many irons in the fire. We [email protected] our industry. It is our obligation as optome- would like to say thank you to our members trists to make sure we recognize our spon- Dr. Nate Shilman who were able to make the NDOA spon- sors, and thank them for their continued sup- President Elect sored golf outing in Bismarck. It was a suc- port of the NDOA. Please speak to all your 2273 3rd Ave West cess as far as the number of attendees, and Dickinson, ND 58601 vendors, and always mention how much we we always have great sponsorship for this 701-225-7886 appreciate their continued support and en- event. -
Party Ballot
GENERAL ELECTION BALLOT NOVEMBER 6, 2018 A STATE OF NORTH DAKOTAB CASS COUNTY C To vote for the candidate of your choice, you must darken the oval ( R ) next to the name of State Senator State Representative that candidate. District 45 District 27 Vote for no more than ONE name Vote for no more than TWO names To vote for a person whose name is not printed on the ballot, you must darken the oval ( R ) next to the blank line provided and write that Ronald Sorvaag Jon Kitzman person's name on the blank line. Republican Party Democratic-NPL Party PARTY BALLOT Danielle Pinnick Thomas Beadle Democratic-NPL Party Republican Party United States Senator Randy G Boehning Vote for no more than ONE name Republican Party Heidi Heitkamp State Representative Ruth Buffalo Democratic-NPL Party District 11 Democratic-NPL Party Kevin Cramer Vote for no more than TWO names Republican Party Gretchen Dobervich Democratic-NPL Party Representative in Congress Kathy Jorgenson State Representative Vote for no more than ONE name Republican Party District 41 Mac Schneider Ron Guggisberg Vote for no more than TWO names Democratic-NPL Party Democratic-NPL Party Kelly Armstrong Bridget Ertelt Michelle Strinden Republican Party Republican Party Republican Party Charles Tuttle Pamela Anderson independent nomination Democratic-NPL Party Al Carlson Republican Party State Senator State Representative Brandon Medenwald District 11 District 13 Democratic-NPL Party Vote for no more than ONE name Vote for no more than TWO names Tim Mathern Austen Schauer Democratic-NPL Party -

May 26, 2017 Kimberly D. Bose, Secretary Federal Energy Regulatory Commission 888 First Street, NE Washington, DC 20426 Re
1250 West Century Avenue Mailing Address: P.O. Box 5601 Bismarck, ND 58506-5601 (701) 530-1600 May 26, 2017 Kimberly D. Bose, Secretary Federal Energy Regulatory Commission 888 First Street, N.E. Washington, D.C. 20426 Re: WBI Energy Transmission, Inc. Updated Landowner List Docket No. CP17-257-000 Dear Ms. Bose: WBI Energy Transmission, Inc. (WBI Energy), pursuant to Section 157.6(d)(5) of the Federal Energy Regulatory Commission’s (Commission) regulations, respectfully submits for filing an updated list of affected landowners for its Valley Expansion Project (Project). As with the original landowner list filed on April 26, 2017, in the above referenced docket, WBI Energy requests privileged treatment of this information, which is labeled: “CUI//PRIV.” Additionally, as of this filing date, only one landowner notice was returned as undeliverable. Upon further review, a correct address was found and notification was sent to the landowner. WBI Energy will continue to update the landowner list if any further undeliverable returned notices are received and provide such updates to the Commission as they become available. As a courtesy, WBI Energy is also providing an updated Project stakeholder list. The information contained in the stakeholder list is public. Any questions regarding this filing should be addressed to the undersigned at (701) 530-1563. Sincerely, /s/ Lori Myerchin Lori Myerchin Manager, Regulatory Affairs Attachments Cc: via email Robin Griffin, FERC Project Manager Valley Expansion Project Resource Report 1 APPENDIX 1I Other -

North Dakota United Announces 2018 Legislative Endorsements
NEWS RELEASE For Release: For More Information, Contact: Feb. 28, 2018 Kelly Hagen Communications Director North Dakota United Phone: 701-223-0450 E-mail: [email protected] North Dakota United Announces 2018 Legislative Endorsements BISMARCK, N.D. – North Dakota United is proud to endorse the following North Dakota state legislators for re-election in 2018. “Their advocacy and support of legislation to strengthen our great public schools, higher education and outstanding public service over the past two legislative sessions is something of which they can be very proud,” said NDU President Nick Archuleta. “Their willingness to work together, regardless of political persuasion, to find solutions to challenges is inspiring and much appreciated by our members and the people of North Dakota.” Representative Andy Maragos (R-3) Senator Nicole Poolman (R-7) Representative Tracy Boe (D-9) Representative Marvin Nelson (D-9) Senator Richard Marcellais (D-9) Representative Gretchen Dobervich (D-11) Representative Ron Guggisberg (D-11) Senator Tim Mathern (D-11) Senator Judy Lee (R-13) Senator Dave Oehlke (R-15) Representative Greg Westlind (R-15) Senator Ray Holmberg (R-17) Representative Kathy Hogan (D-21) for Senate Representative Mary Schneider (D-21) Senator Joan Heckaman (D-23) Representative Alisa Mitskog (D-25) Representative Tom Beadle (R-27) for Senate Representative Bob Martinson (R-35) 301 N. Fourth St., Bismarck, ND 58501 Phone: 701-223-0450 or 800-369-6332 E-mail: [email protected] Visit us online at www.ndunited.org Facebook: www.facebook.com/ndunited Twitter: www.twitter.com/ndunited Senator Erin Oban (D-35) Senator Rich Wardner (R-37) Representative Pam Anderson (D-41) Representative Mary Johnson (R-45) Senator Ron Sorvaag (R-45) These legislators received our endorsement based on their voting records during the 2015 and 2017 legislative sessions, and their proven commitment to the priorities and values of our members. -

2021 FPA-ND Legislative Scorecard
2021 NORTH DAKOTA LEGISLATIVE REPORT CARD 67th LEGISLATIVE SESSION ABOUT THE SCORECARD We are pleased to share this scorecard for the 2021 North Dakota state legislative session. This is a snapshot of how lawmakers voted on key social and moral legislation related to life, education, family, religious freedom, and similar issues. Guided by our mission of building a state where God is honored, religious freedom flourishes, families thrive, and life is cherished, the scorecard focuses on seven bills. This scorecard is not an endorsement of any candidate or political party. It does not measure any lawmakers’ integrity, commitment to their faith, work ethic, or rapport with Family Policy Alliance of North Dakota. It is only a report on how each lawmaker voted. Please continue to hold our legislators accountable for their voting records and please pray that they may always vote in ways that uphold your biblical values as they make important decisions for our state. Sincerely, Mark Jorritsma Executive Director, Family Policy Alliance of North Dakota HOW WE FIGURED THE GRADES A bill is typically passed by a simple majority in the Senate (24 votes out of 47 senators) and the House (48 votes out of 94 Representatives.) Lawmakers earned percentage grades ranging from 0% to 100%, based upon dividing the candidate’s number of good votes cast by the number of total bills he/she voted on. The higher the score, the better their ranking. Not all lawmakers voted on every bill; the number of absences on these key bills is also noted and we encourage you to review whether your legislator actually voted on these important bills. -

Career Workforce Academy
CAREER WORKFORCE ACADEMY Secondary Early Entry • Post-Secondary • Incumbent Worker Information Health Sciences Technology Cass-Clay Transportation Workforce Communication Academy Arts and and Manufacturing Engineering Business/Finance Entrepreneurship Marketing Collaboration • Innovation • Career Preparation Workforce Entry • Technical and Academic Education The Right Student, in the Right Program, for the Right Reasons CAREER ACADEMY: COLLABORATING TO FILL A NEED The Career Academy, proposed by the North Dakota State College of Science (NDSCS), will be a collaborative partnership that includes private sector companies, K-12 school districts in Cass and Clay counties, other two-year educational institutions, the FMWF Chamber of Commerce, and the Greater Fargo-Moorhead Economic Development Corporation and the cities of Fargo and West Fargo. Career and technical education and training will focus on grades 10-14 and also industry incumbent worker skill attainment. Collaboration will occur with other regional and state organizations when deemed relevant.1 EXTENDING EDUCATIONAL AND CAREER BUILDING A DREAM AWARENESS OPPORTUNITIES Funding and partnership support is key to making the Career The Career Academy will provide educational opportunities Academy a reality. The process below identifies the path to beyond what is offered at high schools, such as: success: ◆ ◆ Early Entry options for Career and Technical Education Engage and secure financial support from business, (CTE) or certificate programs. industry and other sources. ◆ Public Communication expounding a new approach ◆ Opportunities to graduate from high school with a to CTE education to advance education and training completed training certificate or program. opportunities that will expand the regions workforce for ◆ Career awareness educational opportunities for secondary residents to live, work and raise a family. -

Directory Governor Doug Burgum North Dakota Legislative Hotline: Lt Governor Brent Sanford for 1-888-635-3447 Attorney General Wayne Stenehjem
North Dakota Elected Officials Reach Your Legislators Directory Governor Doug Burgum North Dakota Legislative Hotline: Lt Governor Brent Sanford for 1-888-635-3447 Attorney General Wayne Stenehjem Secretary of Al Jaeger Bismarck Area: 328-3373 State Legislative Web Site: Treasurer Kelly Schmidt www.legis.nd.gov 66th North Dakota Auditor Josh Gallion Legislative Assembly and Superintendent Kirsten Baesler of Public Join the North Dakota Catholic Elected Officials Instruction Conference Legislative Action Agricultural Doug Goehring Network Commissioner Sign-up at: ndcatholic.org/ Insurance Jon Godfread registration/ Commissioner Or contact the North Dakota Tax Ryan Rauschenberger Catholic Conference at: Commissioner (701) 223-2519 Public Service Brian Kroshus Commissioners Julie Fedorchak 1-888-419-1237 Randy Christmann [email protected] North Dakota Catholic Conference 103 South Third Street, No. 10 Bismarck, North Dakota 58501 U.S. Senator John Hoeven Christopher T. Dodson U.S. Senator Kevin Cramer Follow Us Executive Director U.S. Kelly Armstrong Representative (701) 223-2519 1-888-419-1237 Get contact information for all [email protected] state officials at nd.gov. www.facebook.com/ndcatholic ndcatholic.org Senate House of Representatives Howard C. Anderson, [email protected] 8 Patrick Hatlestad [email protected] 1 Dwight Kiefert [email protected] 24 JoNell A. Bakke [email protected] 43 David Richter [email protected] 1 Alisa Mitskog [email protected] 25 Brad Bekkedahl [email protected] 1 Bert Anderson [email protected] 2 Cynthia Schreiber-Beck [email protected] 25 Randy Burckhard [email protected] 5 Donald W. Longmuir [email protected] 2 Sebastian Ertelt [email protected] 26 David A. -

Nextera Energy PAC 2018 Contributions to State Candidates
NextEra Energy PAC 2018 Contributions to State Candidates Recipient 2018 Amount Chamber State Party Gretchen Whitmer for Governor $ 10,000 Governor MI D Thompson for Senate 2018$ 10,000 STATE SENATE OK R Friends of John Michael Montgomery 2018$ 8,000 STATE SENATE OK R Caldwell for State House$ 7,500 STATE HOUSE OK R Friends of Scott Fetgatter$ 7,500 STATE HOUSE OK R Ken Paxton Campaign$ 7,500 ATTORNEY GENERAL TX R Trey Caldwell for State House 2018$ 7,000 STATE HOUSE OK R Dana Murphy for Lt. Governor$ 5,000 LT. GOVERNOR OK R Friends of Charles McCall $ 5,000 STATE HOUSE OK R Friends of Larry Householder $ 5,000 STATE HOUSE OH R Friends of Todd Russ $ 5,000 STATE HOUSE OK R Stitt for Governor $ 5,000 GOVERNOR OK R Tony for Wisconsin $ 5,000 GOVERNOR WI D Tom Wolf for Governor $ 3,500 GOVERNOR PA D Charles Perry Campaign $ 3,000 STATE SENATE TX R Dawn Buckingham Campaign $ 3,000 STATE SENATE TX R Drew Darby Campaign $ 3,000 STATE HOUSE TX R Four Price Campaign $ 3,000 STATE HOUSE TX R Friends of Greg Babinec $ 3,000 STATE HOUSE OK R Kristi for Governor $ 3,000 GOVERNOR SD R Angela Paxton Campaign $ 2,500 STATE SENATE TX R Brian Birdwell Campaign $ 2,500 STATE SENATE TX R Citizens for Pat Grassley $ 2,500 STATE HOUSE IA R Dennis Bonnen Campaign $ 2,500 STATE HOUSE TX R Friends of James Leewright 2018 $ 2,500 STATE SENATE OK R Friends of John Zerwas $ 2,500 STATE HOUSE TX R Friends of Kim David $ 2,500 STATE SENATE OK R Friends of Stephanie Bice 2018 $ 2,500 STATE SENATE OK R Jacob Rosecrants for HD 46$ 2,500 STATE HOUSE OK D Ken King Campaign $ 2,500 STATE HOUSE TX R Parson for Missouri $ 2,500 GOVERNOR MO R Perryman in 2018 $ 2,500 STATE HOUSE OK D Phil King Campaign $ 2,500 STATE HOUSE TX R Robert Nichols Campaign $ 2,500 STATE SENATE TX R Texans for Kelly Hancock SPAC $ 2,500 STATE SENATE TX R William Casey Murdock 2018 $ 2,500 STATE HOUSE OK R Ana Maria Rodriguez Campaign $ 2,000 STATE HOUSE FL R Ardian Zika Campaign$ 2,000 STATE HOUSE FL R Brett Hage Campaign$ 2,000 STATE HOUSE FL R Bryan Hill for House 2018 $ 2,000 STATE HOUSE OK R Charles Clemons Sr. -
House Standing Committees
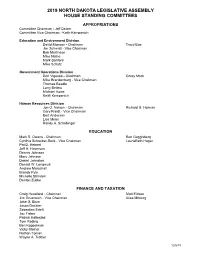
2019 NORTH DAKOTA LEGISLATIVE ASSEMBLY HOUSE STANDING COMMITTEES APPROPRIATIONS Committee Chairman - Jeff Delzer Committee Vice Chairman - Keith Kempenich Education and Environment Division David Monson - Chairman Tracy Boe Jim Schmidt - Vice Chairman Bob Martinson Mike Nathe Mark Sanford Mike Schatz Government Operations Division Don Vigesaa - Chairman Corey Mock Mike Brandenburg - Vice Chairman Thomas Beadle Larry Bellew Michael Howe Keith Kempenich Human Resources Division Jon O. Nelson - Chairman Richard G. Holman Gary Kreidt - Vice Chairman Bert Anderson Lisa Meier Randy A. Schobinger EDUCATION Mark S. Owens - Chairman Ron Guggisberg Cynthia Schreiber-Beck - Vice Chairman LaurieBeth Hager Pat D. Heinert Jeff A. Hoverson Dennis Johnson Mary Johnson Daniel Johnston Donald W. Longmuir Andrew Marschall Brandy Pyle Michelle Strinden Denton Zubke FINANCE AND TAXATION Craig Headland - Chairman Matt Eidson Jim Grueneich - Vice Chairman Alisa Mitskog Jake G. Blum Jason Dockter Sebastian Ertelt Jay Fisher Patrick Hatlestad Tom Kading Ben Koppelman Vicky Steiner Nathan Toman Wayne A. Trottier 12/6/18 HUMAN SERVICES Robin Weisz - Chairman Gretchen Dobervich Karen M. Rohr - Vice Chairman Mary Schneider Dick Anderson Chuck Damschen Bill Devlin Clayton Fegley Dwight Kiefert Todd Porter Matthew Ruby Bill Tveit Greg Westlind Kathy Skroch INDUSTRY, BUSINESS AND LABOR George Keiser - Chairman Mary Adams Mike Lefor - Vice Chairman Pamela Anderson Glenn Bosch Marvin E. Nelson Craig Johnson Jim Kasper Vernon Laning Scott Louser Emily O’Brien David Richter Dan Ruby Austen Schauer JUDICIARY Kim Koppelman - Chairman Ruth Buffalo Karen Karls - Vice Chairman Karla Rose Hanson Rick Becker Terry B. Jones Jeffery J. Magrum Aaron McWilliams Bob Paulson Gary Paur Shannon Roers Jones Bernie Satrom Luke Simons Steve Vetter AGRICULTURE Dennis Johnson - Chairman Ruth Buffalo Wayne A. -
Aicpa Fall Meeting of Council by Patrick Kautzman, AICPA Council Member
January 2019 | Volume XXXVI | No. 1 aicpa fall meeting of council By Patrick Kautzman, AICPA Council Member Since TCJA passed last December, we have heard from a multitude of professionals with varying levels of concern regarding the continued existence of the food and beverage deduction in light of the fate of entertainment expenses. Well, Notice 2018-76, issued October 3, 2018, clarifies that taxpayers generally may continue to deduct 50% of the food and beverage expenses associated with operating their trade or business. Professional Issues Update by Barry Meloncon, President and CEO of AICPA Barry’s professional issues update included his recurring reminders of the rapid pace of innovation and disruption in our world and our industry. • Since the year 2000, 41% of S&P consumer-centric companies have been acquired 2019 or gone out of business and 39% of the 5th to 85th largest firms no longer exist as standalone firms. Conference dates • The World Economic Forum’s Future of Jobs Report shows that of the top 10 de- clining jobs by 2022, #2 is Accounting, Bookkeeping, and Payroll Clerks and #7 is Accountants and Auditors. Barry’s response: They are referring to an industry that Management Conference is unwilling to change and adapt! He broke a future ready strategy down into 3 parts: May 22-23 • Technology – Master it before it masters you Fargo Holiday Inn • Trust – Build on CPAs expertise • Talent – Think broader Summer variety pack Technology – CPAs must embrace “Software as a Service” through client accounting June 17-19 services and virtual CFO services, “Big Data and Analytics”, “Artificial Intelligence” through Bismarck Ramkota machine learning and virtual assistance, and “Blockchain”.