Motion Sickness Traveler Summary Key Points Motion Sickness Consists of a Group of Signs and Symptoms That Develop in Response to Real Or Perceived Motion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Antimuscarinic) Drugs?
© July - August 2018 How well do you know your anticholinergic (antimuscarinic) drugs? nticholinergic drugs, prescribed for a variety of clini- Acal conditions, are amongst the most frequently used prescription drugs in BC (Table 1). Also referred to as “an- timuscarinics,” such drugs specifically block muscarinic receptors for acetylcholine (ACh).1 Muscarinic ACh recep- tors are important in the parasympathetic nervous system that governs heart rate, exocrine glands, smooth muscles, clude drugs whose active metabolites are potent- as well as brain function. In contrast, nicotinic ACh recep- ly antimuscarinic,5 or which often cause typical tors stimulate contraction of striated muscles. This Letter is AC adverse effects such as dry mouth or urinary intended to remind clinicians of commonly used drugs that retention.6 People taking antihistamines, antide- have anticholinergic (AC), or technically, antimuscarinic pressants, antipsychotics, opioids, antimuscarinic properties, and of their potential adverse effects. inhalers, or many other drugs need to know that Beneficial and harmful effects of anticholinergic drugs have blockade of ACh receptors can cause bothersome been known for centuries. In Homer’s Odyssey, the nymph or even dangerous adverse effects (Table 3). pharmacologist Circe utilized central effects of atropinics Subtle and not-so-subtle toxicity in the common plant jimson weed (Datura stramonium) to cause delusions in the crew of Odysseus. Believing they Students often learn the adverse effects of anticho- had been turned into pigs, they could be herded.2 linergics from a mnemonic, e.g.: “Blind as a bat, Sometimes a drug is recommended specifically for its an- mad as a hatter, red as a beet, hot as a hare, dry as ticholinergic potency. -

Drugs That Can Cause Delirium (Anticholinergic / Toxic Metabolites)
Drugs that can Cause Delirium (anticholinergic / toxic metabolites) Deliriants (drugs causing delirium) Prescription drugs . Central acting agents – Sedative hypnotics (e.g., benzodiazepines) – Anticonvulsants (e.g., barbiturates) – Antiparkinsonian agents (e.g., benztropine, trihexyphenidyl) . Analgesics – Narcotics (NB. meperidine*) – Non-steroidal anti-inflammatory drugs* . Antihistamines (first generation, e.g., hydroxyzine) . Gastrointestinal agents – Antispasmodics – H2-blockers* . Antinauseants – Scopolamine – Dimenhydrinate . Antibiotics – Fluoroquinolones* . Psychotropic medications – Tricyclic antidepressants – Lithium* . Cardiac medications – Antiarrhythmics – Digitalis* – Antihypertensives (b-blockers, methyldopa) . Miscellaneous – Skeletal muscle relaxants – Steroids Over the counter medications and complementary/alternative medications . Antihistamines (NB. first generation) – diphenhydramine, chlorpheniramine). Antinauseants – dimenhydrinate, scopolamine . Liquid medications containing alcohol . Mandrake . Henbane . Jimson weed . Atropa belladonna extract * Requires adjustment in renal impairment. From: K Alagiakrishnan, C A Wiens. (2004). An approach to drug induced delirium in the elderly. Postgrad Med J, 80, 388–393. Delirium in the Older Person: A Medical Emergency. Island Health www.viha.ca/mhas/resources/delirium/ Drugs that can cause delirium. Reviewed: 8-2014 Some commonly used medications with moderate to high anticholinergic properties and alternative suggestions Type of medication Alternatives with less deliriogenic -

Adverse Reactions to Hallucinogenic Drugs. 1Rnstttutton National Test
DOCUMENT RESUME ED 034 696 SE 007 743 AUTROP Meyer, Roger E. , Fd. TITLE Adverse Reactions to Hallucinogenic Drugs. 1rNSTTTUTTON National Test. of Mental Health (DHEW), Bethesda, Md. PUB DATP Sep 67 NOTE 118p.; Conference held at the National Institute of Mental Health, Chevy Chase, Maryland, September 29, 1967 AVATLABLE FROM Superintendent of Documents, Government Printing Office, Washington, D. C. 20402 ($1.25). FDPS PRICE FDPS Price MFc0.50 HC Not Available from EDRS. DESCPTPTOPS Conference Reports, *Drug Abuse, Health Education, *Lysergic Acid Diethylamide, *Medical Research, *Mental Health IDENTIFIEPS Hallucinogenic Drugs ABSTPACT This reports a conference of psychologists, psychiatrists, geneticists and others concerned with the biological and psychological effects of lysergic acid diethylamide and other hallucinogenic drugs. Clinical data are presented on adverse drug reactions. The difficulty of determining the causes of adverse reactions is discussed, as are different methods of therapy. Data are also presented on the psychological and physiolcgical effects of L.S.D. given as a treatment under controlled medical conditions. Possible genetic effects of L.S.D. and other drugs are discussed on the basis of data from laboratory animals and humans. Also discussed are needs for futher research. The necessity to aviod scare techniques in disseminating information about drugs is emphasized. An aprentlix includes seven background papers reprinted from professional journals, and a bibliography of current articles on the possible genetic effects of drugs. (EB) National Clearinghouse for Mental Health Information VA-w. Alb alb !bAm I.S. MOMS Of NAM MON tMAN IONE Of NMI 105 NUNN NU IN WINES UAWAS RCM NIN 01 NUN N ONMININI 01011110 0. -

Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the Use of Antiemetics Author(S): Dr Annette Edwards (Chai
Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the use of Antiemetics Author(s): Dr Annette Edwards (Chair) and Deborah Royle on behalf of the Yorkshire Palliative Medicine Clinical Guidelines Group Overall objective : To provide guidance on the evidence for the use of antiemetics in specialist palliative care. Search Strategy: Search strategy: Medline, Embase and Cinahl databases were searched using the words nausea, vomit$, emesis, antiemetic and drug name. Review Date: March 2008 Competing interests: None declared Disclaimer: These guidelines are the property of the Yorkshire Palliative Medicine Clinical Guidelines Group. They are intended to be used by qualified, specialist palliative care professionals as an information resource. They should be used in the clinical context of each individual patient’s needs. The clinical guidelines group takes no responsibility for any consequences of any actions taken as a result of using these guidelines. Contact Details: Dr Annette Edwards, Macmillan Consultant in Palliative Medicine, Department of Palliative Medicine, Pinderfields General Hospital, Aberford Road, Wakefield, WF1 4DG Tel: 01924 212290 E-mail: [email protected] 1 Introduction: Nausea and vomiting are common symptoms in patients with advanced cancer. A careful history, examination and appropriate investigations may help to infer the pathophysiological mechanism involved. Where possible and clinically appropriate aetiological factors should be corrected. Antiemetics are chosen based on the likely mechanism and the neurotransmitters involved in the emetic pathway. However, a recent systematic review has highlighted that evidence for the management of nausea and vomiting in advanced cancer is sparse. (Glare 2004) The following drug and non-drug treatments were reviewed to assess the strength of evidence for their use as antiemetics with particular emphasis on their use in the palliative care population. -

The Use of Cyclizine in Patients Receiving Parenteral Nutrition
DRAFT - The use of cyclizine in patients receiving parenteral nutrition Jeremy Nightingale, Uchu Meade, Gavin Leahy and the BIFA committee Cyclizine is a piperazine derivative that was discovered in 1947 while researching new antihistamine drugs (H1 blockers) and was first sold 1965. It is marketed for the treatment or prevention of nausea, vomiting, and labyrinthine disorders including vertigo and motion sickness. This includes nausea after a general anaesthetic and that caused by opioid use. In the United Kingdom the oral formulation is classified as a Pharmacy (P) medicine and can be sold from a registered pharmacy premises by or under the supervision of a pharmacist. The intravenous formulation is classified as a Prescription Only Medicine (POM). There is increasing recognition that the intravenous formulation of cyclizine may cause euphoria and dependence (addiction); these side effects may not be reported by patients and be under recognised by healthcare professionals. It has many associated problems when used by patients receiving long-term parenteral nutrition. This position paper highlights the risks associated with its long-term intravenous use. Actions/pharmacology (1) Cyclizine has both anti-histamine (H1) and anti-cholinergic (anti-muscarinic M1) effects. It is a class 1 drug in the biopharmaceutical classification (high permeability and solubility) with a peak plasma concentration of about 70 ng/ ml reached approximately 2 hours after oral ingestion, as measured in healthy adult patients. Its quoted elimination (biological) half-life is 20 hours when given orally (1) and 13 hours when given intravenously (2). Cyclizine is metabolised to its N-demethylated derivative, norcyclizine, which has little anti-histaminic (H1) activity compared to cyclizine. -
Stability and Compatibility of Combinations of Hydromorphone
The Canadian Journal of Hospital Pharmacy - Volume 46, No. 2, April 1993 61 Stability and Compatibility of Combinations oman of Hydromorphone and Dimenhydrinate, ations Lorazepam or Prochlorperazine Jnally >hoto- Scott E. Walker, John Iazzetta, Carlo De Angelis and Danny W.C. Lau laser :ii, in figure ABSTRACT RESUME .Each The stability and compatibility of combinations of hydro On a melange diverses solutions d'hydromorphone .rabic morphone (2, 10 and 40 mg/ml) admixed separately with (2, 10 et 40 mg/ml) avec, separemen( un volume egal :onse- dimenhydrinate (50 mg/ml), prochlorperazine (5 mg/ml), d'une solution soit de dimenhydrate (50 mglmL), de 1ld be or lorazepam (4 mg/ml) were tested over a seven-day prochlorperazine (5 mglmL) ou de lorazepam (4 mglmL), Jarate period at 4°C, 23°C and 37°C In addition to visual pour verifier la compatibilite de ces trois medicaments avec lished inspection and pH, the concentration of each component l'hydromorphone et determiner la stabilite du melange ie ac in the binary mixture was determined by a stability binaire pendant sept jours a 4°C, a 23°C et a 37°C ion to indi.cating lifjuid chromatographic method Each test was En plus d'effectuer wz examen visuel et de deter ipt. completed at time zero, one, four, six and seven days after miner le pH, on a dose !es composants des melanges par mixing equal volumes of each medication. une methode de chromatographie en phase lifjuide indi The hydromorphone-dimenhydrinate combination was quant la stabilite. On a analyse !es melanges au moment compatible and stable for 24 hours. -

Chapter 34 • Drugs Used to Treat Nausea and Vomiting
• Chapter 34 • Drugs Used to Treat Nausea and Vomiting • Learning Objectives • Compare the purposes of using antiemetic products • State the therapeutic classes of antiemetics • Discuss scheduling of antiemetics for maximum benefit • Nausea and Vomiting • Nausea : the sensation of abdominal discomfort that is intermittently accompanied by a desire to vomit • Vomiting (emesis): the forceful expulsion of gastric contents up the esophagus and out of the mouth • Regurgitation : the rising of gastric or esophageal contents to the pharynx as a result of stomach pressure • Common Causes of Nausea and Vomiting • Postoperative nausea and vomiting • Motion sickness • Pregnancy Hyperemesis gravidarum: a condition in pregnancy in which starvation, dehydration, and acidosis are superimposed on the vomiting syndrome • Common Causes of Nausea and Vomiting (cont’d) • Psychogenic vomiting: self-induced or involuntary vomiting in response to threatening or distasteful situations • Chemotherapy-induced emesis (CIE) Anticipatory nausea and vomiting: triggered by sight and smell associated with treatment Acute CIE: stimulated directly by chemotherapy 1 to 6 hours after treatment Delayed emesis: occurs 24 to 120 hours after treatment; may be induced by metabolic by-products of chemotherapy • Drug Therapy for Selected Causes of Nausea and Vomiting • Postoperative nausea and vomiting (PONV) • Antiemetics include: Dopamine antagonists Anticholinergic agents Serotonin antagonists H2 antagonists (cimetidine, ranitidine) • Nursing Process for Nausea and Vomiting -

On the Approximation of the Laws of the Member States Relating to Cosmetic Products (76/768/EEC )
27 . 9 . 76 Official Journal of the European Communities No L 262/169 COUNCIL DIRECTIVE of 27 July 1976 on the approximation of the laws of the Member States relating to cosmetic products (76/768/EEC ) THE COUNCIL OF THE EUROPEAN COMMUNITIES, regards the composition, labelling and packaging of cosmetic products ; Having regard to the Treaty establishing the Euro pean Economic Community, and in particular Whereas this Directive relates only to cosmetic prod Article 100 thereof, ucts and not to pharmaceutical specialities and medicinal products ; whereas for this purpose it is necessary to define the scope of the Directive by Having regard to the proposal from the Commission, delimiting the field of cosmetics from that of phar maceuticals ; whereas this delimitation follows in particular from the detailed definition of cosmetic Having regard to the opinion of the European Parlia products, which refers both to their areas of appli ment ( 1 ), cation and to the purposes of their use; whereas this Directive is not applicable to the products that fall Having regard to the opinion of the Economic and under the definition of cosmetic product but are Social Committee (2 ), exclusively intended to protect from disease; whereas, moreover, it is advisable to specify that certain prod ucts come under this definition, whilst products Whereas the provisions laid down by law, regulation containing substances or preparations intended to be or administrative action in force in the Member ingested, inhaled, injected or implanted in the human States -

Medicines Classification Committee
Medicines Classification Committee Meeting date 1 May 2017 58th Meeting Title Reclassification of Sedating Antihistamines Medsafe Pharmacovigilance Submitted by Paper type For decision Team Proposal for The Medicines Adverse Reactions Committee (MARC) recommended that the reclassification to committee consider reclassifying sedating antihistamines to prescription prescription medicines when used in children under 6 years of age for the treatment of medicine for some nausea and vomiting and travel sickness [exact wording to be determined by indications the committee]. Reason for The purpose of this document is to provide the committee with an overview submission of the information provided to the MARC about safety concerns associated with sedating antihistamines and reasons for recommendations. Associated March 2013 Children and Sedating Antihistamines Prescriber Update articles February 2010 Cough and cold medicines clarification – antihistamines Medsafe website Safety information: Use of cough and cold medicines in children – new advice Medicines for Alimemazine Diphenhydramine consideration Brompheniramine Doxylamine Chlorpheniramine Meclozine Cyclizine Promethazine Dexchlorpheniramine New Zealand Some oral sedating antihistamines available without exposure to a prescription (pharmacist-only and pharmacy only), sedating therefore usage data is not easily available. antihistamines Table of Contents 1.0 PURPOSE ...................................................................................................................................... -

Post‐Operative Nausea & Vomiting ‐ Use of Anti‐Emetic
© 2012 Scottish Universities Medical Journal, Vol 1 Issue 1: page 89-97 Dundee Published online: Feb 2012 Rother C ‘Post-Operative Nausea & Vomiting – use of anti-emetic agents in anaesthesia’ Post‐Operative Nausea & Vomiting ‐ Use of Anti‐Emetic Agents in Anaesthesia Catriona Rother (4th Year MBChB, BMSc) University of Dundee Correspondence to: [email protected] ABSTRACT Post‐operative nausea and vomiting (PONV) is a recurrent problem in the field of anaesthetics. It is usually defined as nausea, retching or vomiting within 24 hours of surgery and affects 20‐30% of patients. Although often considered merely an unpleasant side effect of general anaesthesia or surgery, PONV can result in many unwanted and potentially serious outcomes and increases healthcare expenditure considerably. Background Post‐operative nausea and vomiting (PONV) usually defined as nausea, retching or vomiting within 24 hours of surgery and affects 20‐30% of patients.1, 2, 3 PONV is an important problem and can lead to potentially serious outcomes and an increase healthcare expenditure.2 Post‐operative nausea and vomiting increases recovery room time, requiring expanded levels of nursing care,4, 5 and delays mobilisation following surgery as movement often exacerbates PONV.3 As a result, the early discharge of ambulatory surgery patients is frequently delayed,1 with around 1% requiring overnight admission.6 Persistent vomiting can result in dehydration, electrolyte imbalance and metabolic alkalosis.7, 8 The oral administration of drugs, nutrition and fluids may also be delayed5 and the level of post‐operative analgesia that can be obtained may be limited if effective doses of opiate cannot be administered orally. -
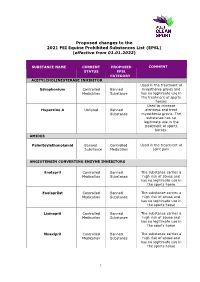
Proposed Changes to the 2021 FEI Equine Prohibited Substances List (EPSL) (Effective from 01.01.2022)
Proposed changes to the 2021 FEI Equine Prohibited Substances List (EPSL) (effective from 01.01.2022) SUBSTANCE NAME CURRENT PROPOSED COMMENT STATUS EPSL CATEGORY ACETYLCHOLINESTERASE INHIBITOR Used in the treatment of Edrophonium Controlled Banned myasthenia gravis and Medication Substance has no legitimate use in the treatment of sports horses Used to increase Huperzine A Unlisted Banned alertness and treat Substance myasthenia gravis. The substance has no legitimate use in the treatment of sports horses. AMIDES Palmitoylethanolamid Banned Controlled Used in the treatment of Substance Medication joint pain ANGIOTENSIN CONVERTING ENZYME INHIBITORS Enalapril Controlled Banned The substance carries a Medication Substance high risk of abuse and has no legitimate use in the sports horse Enalaprilat Controlled Banned The substance carries a Medication Substance high risk of abuse and has no legitimate use in the sports horse Lisinopril Controlled Banned The substance carries a Medication Substance high risk of abuse and has no legitimate use in the sports horse Moexipril Controlled Banned The substance carries a Medication Substance high risk of abuse and has no legitimate use in the sports horse 1 Perindoprilat Controlled Banned The substance carries a Medication Substance high risk of abuse and has no legitimate use in the sports horse ANTIHISTAMINES Antazoline Controlled Banned The substance has no Medication Substance legitimate use in the sports horse Azatadine Controlled Banned The substance has Medication Substance sedative effects -

A Comparison of the Anti-Emetic Effects of Dimenhydrinate, Promethazine
A COMPARISON OF THE ANTI-EMETIC EFFECTS OF DIMENHYDRINATE, PROMETHAZINE HYD]ROCHLORIDE AND CHLORPROMAZINE FOLLOWING ANAESTHESIA DOREEN CAPLIN, M.D.*, and CODE SMXTH, 1VLD.*= Vo~rriNc during the immediate postoperalave period is a frequent complica- tion of anaesthesia m children Dimenhydrinate, promethazme hydrochloride, and chlorpromazine have all been recommended as effeclave anti-emetic drugs (1, 2, 3). A comparison o; the chmcal efficacy of these three agents was made with a carefully selected and controlled group of patients. A group of patients undergoing operalaon for correction of squint was chosen for this study for the following reasons: 1. They were reputed to have a relatively high incidence of post-anaesthetic vomzlang, a prerequisite for ~he demonstratmn of anti-emetic action in a relatively small series of cases 2. There was no operatJve interference with or disease of the gastro-intestinal tract. 3. All operations lasted between one-half and one hour. 4. All pataents were on the same ward with the result that observations were made by the same nursing personnel throughout the proleet, 5. All cases were electave and had receaved nothing by mouth for at least four hours prior to induction, ~md had received no solid food since the evening prior to operation. The cases used in the study were drawn from both public and private patients of certain eye-surgeons and were elther treated or placed in the control group on a completely random basis. The first comparison was made between 40 cases treated with dimenhydrinate and 40 untreated controls. Towards the completaon of this series, optimistic reports of the effectiveness of promethazine hydrochlorlde and chlorpromazine prompted us to conduct a second serms consislang ~f 20 cases treated with promethazme hydrochlorlde, 25 casestreated with chlorpromazine and 20 un- treated controls.