Building a Healthier St. Louis” for April 2003 Release
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

First and Second Generations of Urban Black Mayors: Atlanta, Detroit, and St
Western Michigan University ScholarWorks at WMU Master's Theses Graduate College 12-2001 First and Second Generations of Urban Black Mayors: Atlanta, Detroit, and St. Louis Harold Eugene Core Follow this and additional works at: https://scholarworks.wmich.edu/masters_theses Part of the Political Science Commons Recommended Citation Core, Harold Eugene, "First and Second Generations of Urban Black Mayors: Atlanta, Detroit, and St. Louis" (2001). Master's Theses. 3883. https://scholarworks.wmich.edu/masters_theses/3883 This Masters Thesis-Open Access is brought to you for free and open access by the Graduate College at ScholarWorks at WMU. It has been accepted for inclusion in Master's Theses by an authorized administrator of ScholarWorks at WMU. For more information, please contact [email protected]. FIRST AND SECOND GENERATIONS OF URBAN BLACK MAYORS: ATLANTA, DETROIT, AND ST. LOUIS by Harold Eugene Core, Jr A Thesis Submitted to the Faculty of The Graduate College In partial fulfillmentof the Requirements for the Degree of Master of Arts Department of Political Science Western Michigan University Kalamazoo, Michigan December 2001 © 2001 Harold Eugene Core, Jr ACKNOWLEDGEMENTS I would like to first acknowledge the courage and leadership of those very first urban black mayors. Without their bravery, hard work, and accomplishments this research, and possibly even this researcher would not exist. In many ways they served as the flagship for the validity of black political empowerment as they struggled to balance their roles as leaders of large cities and spokespersons for the African American cause. Secondly I would like to thank the members of my thesis committee, specifically Dr. -

1 Race and the Reelection of the Longest Serving Mayor of St. Louis
Race and the Reelection of the Longest Serving Mayor of St. Louis P. Frances Gouzien David C. Kimball St. Louis City Primary Election Candidates, March 2013 Francis G. Slay Lewis Reed Age: 57 Age: 50 Sex: Male Sex: Male Race: White Race: African American Religion: Catholic Religion: Not reported Education: Law degree from St. Louis Education: Attended Southern Illinois University Law School, B.S. in political University and studied mathematics and science from Quincy College computer science Occupation: Attorney Occupation: Corporate management and information technology Political Experience: St. Louis Alderman for Political Experience: St. Louis Alderman for 23rd Ward, 1985-1995; President of the St. the 6th Ward, 1999-2007; President of the St. Louis Board of Aldermen, 1995-2001; Mayor Louis Board of Aldermen, 2007-present. of St. Louis, 2001-present. In 2013 Mayor Francis Slay was elected to a record fourth term and he is now the longest serving mayor in St. Louis history. Mayor Slay has maintained a winning electoral coalition since his first election in 2001, although that coalition was tested in the 2013 election. While Mayor Slay’s electoral coalition has several features of an urban regime, his record-setting reelection does not guarantee that major items on his agenda will be implemented. Characteristics of the City Many institutional features of St. Louis government weaken the mayor’s power and foster political factionalism. The city has a mayor-council form of government with a weak mayor. City budgets and contracts are controlled by the three-person Board of Estimate and Apportionment (BEA), which includes the mayor and the separately elected Comptroller and President of the Board of Aldermen. -

Missouri Blue Ribbon Panel on Hyperloop
Chairman Lt. Governor Mike Kehoe Vice Chairman Andrew G. Smith Panelists Jeff Aboussie Cathy Bennett Tom Blair Travis Brown Mun Choi Tom Dempsey Rob Dixon Warren Erdman Rep. Travis Fitzwater Michael X. Gallagher Rep. Derek Grier Chris Gutierrez Rhonda Hamm-Niebruegge Mike Lally Mary Lamie Elizabeth Loboa Sen. Tony Luetkemeyer MISSOURI BLUE RIBBON Patrick McKenna Dan Mehan Joe Reagan Clint Robinson PANEL ON HYPERLOOP Sen. Caleb Rowden Greg Steinhoff Report prepared for The Honorable Elijah Haahr Tariq Taherbhai Leonard Toenjes Speaker of the Missouri House of Representatives Bill Turpin Austin Walker Ryan Weber Sen. Brian Williams Contents Introduction ................................................................................................................................................ 3 Executive Summary .................................................................................................................................... 5 A National Certification Track in Missouri .................................................................................................. 8 Track Specifications .............................................................................................................................. 10 SECTION 1: International Tube Transport Center of Excellence (ITTCE) ..................................... 12 Center Objectives .............................................................................................................................. 12 Research Areas ................................................................................................................................. -

St. Louis Currents: the Fifth Edition
Southern Illinois University Edwardsville SPARK SIUE Faculty Research, Scholarship, and Creative Activity 2018 St. Louis Currents: The Fifth Edition Andrew Theising [email protected] E. Terrence Jones Ph.D. University of Missouri-St. Louis Follow this and additional works at: https://spark.siue.edu/siue_fac Part of the American Politics Commons, Cultural History Commons, Economic History Commons, Environmental Studies Commons, Leisure Studies Commons, Other History Commons, Other Political Science Commons, Public Economics Commons, Social Justice Commons, Taxation Commons, and the Urban Studies and Planning Commons Recommended Citation Theising, Andrew and Jones, E. Terrence Ph.D., "St. Louis Currents: The Fifth Edition" (2018). SIUE Faculty Research, Scholarship, and Creative Activity. 136. https://spark.siue.edu/siue_fac/136 This Book is brought to you for free and open access by SPARK. It has been accepted for inclusion in SIUE Faculty Research, Scholarship, and Creative Activity by an authorized administrator of SPARK. For more information, please contact [email protected],[email protected]. St. Louis Currents The Fifth Edition Edited by Andrew J. Theising Southern Illinois University Edwardsville and E. Terrence Jones University of Missouri–St. Louis Managing Editors: Heather Birdsell and Hugh Pavitt SIUE Institute for Urban Research © 2016 The Board of Trustees of Southern Illinois University, Edwardsville, IL All Rights Reserved. No portion of this book or its illustrations may be reproduced in any form without the expressed written -

Hssu President's Report 08 Web.Pdf
Pivotal Years in the Evolution of Harris-Stowe State University 1857 Harris Teachers College The St. Louis Board of Education founds Harris Teachers College to prepare white teachers for white elementary schools. 1890 Stowe Teachers College The St. Louis Board of Education founds Stowe Teachers College to prepare black teachers for black elementary schools. 1938 Both colleges reorganize themselves and form two academic levels: a junior college division and a senior college division. 1954 Harris Teachers College The St. Louis Board of Education merges the two colleges, which became Harris Teachers College. 1977 Harris-Stowe College The St. Louis Board of Education changes the name to Harris-Stowe College. 1979 The state of Missouri passes legislation that makes Harris-Stowe College a part of the state’s system of Public Higher Education. 1981 The state of Missouri approves baccalaureate degree programs in Early Childhood Education, Middle School Education and Urban Education. 1987 Historically Black College Harris-Stowe College is named one of the nation’s Historically Black Colleges and Universities under the U.S. Department of Education. 1993 Harris-Stowe State College The state of Missouri authorizes the college to expand its mission by offering baccalaureate degree programs in Business Administration, Secondary Teacher Education and Criminal Justice, as well as to add the word “state” to its title. 1996 The city of St. Louis gives the college nearly 18 acres of land, formerly Laclede Town site, for just $10. 1998 AT&T Library and Technology Resource Center Construction of this building, formerly the Southwestern Bell Library and Technology Resource Center, begins. -

Missouri Info OM Ch 9
CHAPTER 9 Missouri Information Harvesting wheat at the O.E. Clark farm, c1910 Gill Photograph Collection Missouri State Archives 894 OFFICIAL MANUAL ND DIV TA ID S E D E E PLU UM RI BU N S U W W E D F E A T I L N L SALUS U X ESTO LE P O P A U L I S UP R E M M D C C C X X Newspaper Organizations Missouri Press Association 802 Locust St. Columbia 65201 DOUG CREWS Teletelephone: (573) 449-4167 / FAX: (573) 874-5894 Executive Director www.mopress.com Missouri Press Association The Missouri Press Association is an organi- On the occasion of its 100th anniversary in zation of newspapers in the state. 1966, the association re-established the old Organized May 17, 1867, as the Editors and Saline County Herald newspaper office in his- Publishers Association of Missouri, the name toric Arrow Rock and maintains a newspaper was changed in 1877 to the Missouri Press Asso- equipment museum in connection with it. ciation. In 1922, the association became a non- The Missouri Press Foundation administers profit corporation; a central office was opened and funds seminars and workshops for newspa- under a field manager whose job it was to travel per people, supports Newspapers In Education the state and help newspapers with problems. programs, and funds scholarships and intern- The association, located in Columbia, became ships for Missouri students studying community the fifth press association in the nation to finance journalism in college. its headquarters through member contributions. Membership in the association is voluntary. -

The Times of Skinker Debaliviere April-May 1999
The TIMES of.... SKINKERDEBALIVIERE Vol. 30 No. 1 April-May 1999 FREE The oldest neighborhood newspaper in St. Louis Independent and all volunteer-run since 1970 Rebuilding Communities Bill Goes to Senate Joe Edwards Hopes to Spread by JoAnn Vatcha An important legislative initiative, the "Rebuilding Communities" bill, House bill 246, is currently under consideration by the State Senate, which will vote His Magic East of Skin ker during the session ending May 15. This law is designed to build on the state historic credit that became law in January of 1998, which is already having Joe Edwards, neighborhood resident and highly successful entrepreneur in tangible effects on rehab in many historic neighborhoods, including Skinker- the University City Loop, hopes to help redevelop the 6100 block of Delmar. DeBaliviere. Edwards, owner of Blueberry Hill and the Tivoli, along with partner Pat The new law also builds on the 1998 "Rebuilding Communities Law", which Hagin, wants to develop a concert hall/night club at 6161 Delmar. This is on gives incentives to certain types of businesses to locate in distressed communi- the north side of the street where the Wabash Triangle Cafe once stood. The ties (defined to include the entire City of St. Louis). Businesses which start up or venue will be called the Pageant. The name is taken from a movie theatre that locate in the City obtain 3 years of state tax credits, more than offsetting the city used to stand a short distance east on Delmar from the proposed site. earnings tax for the company and its employees. -

A History of Health Care for the Indigent in St. Louis: 1904–2001
CORE Metadata, citation and similar papers at core.ac.uk Provided by Saint Louis University School of Law Research: Scholarship Commons Saint Louis University Law Journal Volume 48 Number 1 Unequal Treatment: Racial and Ethnic Article 9 Disparities in Health Care (Fall 2003) 12-1-2003 A History of Health Care for the Indigent in St. Louis: 1904–2001 Daniel R. Berg, M.D. Follow this and additional works at: https://scholarship.law.slu.edu/lj Part of the Law Commons Recommended Citation Daniel R. Berg, M.D., A History of Health Care for the Indigent in St. Louis: 1904–2001, 48 St. Louis U. L.J. (2003). Available at: https://scholarship.law.slu.edu/lj/vol48/iss1/9 This Article is brought to you for free and open access by Scholarship Commons. It has been accepted for inclusion in Saint Louis University Law Journal by an authorized editor of Scholarship Commons. For more information, please contact Susie Lee. SAINT LOUIS UNIVERSITY SCHOOL OF LAW A HISTORY OF HEALTH CARE FOR THE INDIGENT IN ST. LOUIS: 1904–2001 DANIEL R. BERG, M.D.* I. INTRODUCTION The city of St. Louis assumes the responsibility to “provide for the support, maintenance and care of children and sick, aged or insane poor persons and paupers.”1 Despite this bold statement in the City Charter, infant mortality in north St. Louis is still more than double the United States’ average, and higher than many Third World countries.2 In fact, there is an entire underclass within the city that suffers from health outcomes more comparable to the Third World countries than to their neighbors in west St. -
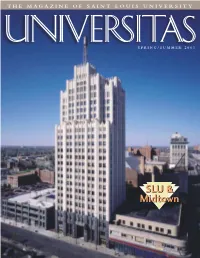
NEW Utas Fall
THE MAGAZINE OF SAINT LOUIS UNIVERSITY SPRING/SUMMER 2003 SLUSLU && MidtownMidtown By Lawrence Biondi, S.J. Saint Louis University President t’s official: After extensive research and planning, Saint The need for a dedicated research facility has become a ILouis University is moving forward on plans for two excit- necessity as external funding for SLU research has expanded ing projects — an arena and a research building. You can read significantly and successfully during the past decade. The ini- more about the details elsewhere in this issue, but I wanted to tiative for a new research building at our Health Sciences share my perspective on these monumental undertakings and Center is part of an overall $80 million investment in new what they mean for SLU. and renovated research space that will represent the largest Let’s start with the arena. This project has generated much single building project since the University’s founding in discussion over the years, especially among our Billiken faith- 1818. (For more details, see page 2.) ful. Although SLU has been eager to put the pieces in place The new research building will provide state-of-the-art for a top-notch athletic facility for some time now, funding facilities for health sciences research that directly touches lives proved to be a major obstacle. We also maintained that a while providing additional services to the community. The new arena should serve much more than our Billiken men’s facility will allow for the consolidation of laboratories scat- basketball program. tered in different locations at the Health Yes, we envision a 13,000-seat basket- Sciences Center. -

The 1857 Project This Special Issue Examines the History of Slavery, Segregation and Racism in Our Region
The 1857 Project This special issue examines the history of slavery, segregation and racism in our region. It was produced with the help and financial support of the Pulitzer Center on Crisis Reporting. 2020• Volume 49 Number 356 • $8 CONTRIBUTORS PUBLISHED BY: School of Journalism College WILLIAM H. FREIVOGEL of Mass Communication and PUBLISHER Media Arts William H. Freivogel is a former editorial page Deborah Tudor, Interim Dean deputy editor for the St. Louis Post-Dispatch and Jan Thompson, Director contributes to St. Louis Public Radio. He is a member of the Missouri Bar. HARPER BARNES Harper Barnes, a former critic-at-large of the St. BOARD OF ADVISERS: Louis Post-Dispatch, is the author of “Standing on Jim Kirchherr, Don Corrigan, JACKIE SPINNER EDITOR a Volcano: The Life add Times of David Rowland Lisa Bedian, Tammy Merrett, Jackie Spinner is an Associate Professor at Columbia Francis” (Missouri Historical Society Press) as well Rita Csapo-Sweet, Steve Perron, College in Chicago; freelance independent journalist as “Never Been a Time” (Walker). Eileen Duggan, Michael D. specializing on the Middle East; former Baghdad Sorkin, David P. Garino, Rick Bureau Chief Washington Post. KAYLA CHAMNESS Stoff, Ted Gest, Fred Sweet, Kayla Chamness, senior at SIUC and reporter on William Greenblatt, Lynn GJR staff. Venhaus, Daniel Hellinger, Robert MANAGING EDITOR ZAHEDUR R. ARMAN A. Cohn, Michael E. Kahn, John Zahedur R. Arman is the founding president of BD PERCY GREEN P. Dubinsky, Gerald Early, Paul Fact Check. He is a doctoral student in the SIUC Schoomer, Moisy Shopper, Ray Percy Green led the ACTION civil rights group, College of Mass Communication and Media Arts. -

Resilient St. Louis
Resilient St. Louis Mayor Lyda Krewson Table of Contents Executive Summary 6 Introduction 8 100RC Background 8 Adapting 100 Resilient Cities for St. Louis 9 Resilient St. Louis Background 10 The 100 Resilient Cities Network 12 St. Louis’s Resilience Challenges 14 Toward a More Resilient St. Louis 30 Pillar 1: Residents 36 Pillar 2: Neighborhoods 46 Pillar 3: Systems 60 Appendix: Resilient St. Louis Actions Summary 72 Photo Credits 82 Acknowledgements 83 Letter from Mayor Lyda Krewson Over the past 250 years the City of St. Louis has faced great challenges, from record-breaking floods and tornadoes to drastic depopulation and systemic racial inequity. To thrive over the next 250 years St. Louis must position itself to face the next set of issues as the global climate changes and cities adapt to meet new social norms. A more resilient St. Louis means more than just concentrated vacant land and abandoned properties bolstering our physical infrastructure to withstand that divide and devalue our neighborhoods — issues storms and floods. For St. Louis to truly build resilience that make our residents more vulnerable to crime and we have to begin by supporting people. Residents are other hardships. Climate change will also challenge us in the most important asset our city has, and we must the years to come. We can expect warmer temperatures ensure that all St. Louisans — particularly those whom and more frequent and more extreme weather events. we know to be our most vulnerable — are prepared for The effects of these challenges may again fall and capable of facing personal and community-level disproportionately on our city’s most vulnerable, unless our challenges when they arise. -

New Master Page 4A
PAGE 4A • THE ST. LOUIS EVENING WHIRL • TUESDAY, MARCH 24-31, 2015 • @thewhirlonline The Truth Hurts Sometimes: The St. Louis Evening Whirl’s Editorials & Opinions You Still Must Tell It! By Rev. Rodrick Burton COMMUNITY MATTERS Jonathan Capehart is an African American writer, blogger, and substitute-anchor on MSNBC’s “UP with Steve Kornac- ki.” Capehart strongly protested the injustice of the Michael Brown killing everywhere he Roadmap to Empowerment: Fruitful For STL Urban League Clients & Sponsors could until March the 16th when he wrote this piece, ‘Hands Up Don’t Shoot’ was built on a lie. He did not retreat one bit from calling for an end to police profiling, militarization, and bru- tality. Caphart did not step back from calling for an end to state sponsored debtor’s prison with unjust ticketing and incarceration. He still called and demands that America value black lives as much as everyone else, but he apologized for using Michael Brown’s case as an example after he read the exhaustive Department of Justice Report on his shooting. Before we go any further, we must note that many welcome and cite the Department of Justice Report on Ferguson’s sys- tematic racism in governance, policing, and courts. Many hold it up as undeniable, verifiable, factual truth; proving what blacks have been saying all along about Ferguson. On the flip side, that same army of investigators, FBI agents, and forensic researchers in an 86 page report found that Offic- LEFT: STL Mayor Francis Slay; former U.S. Secretary of Labor Alexis Herman; Keynoter Dr.