Urine Drug Testing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Review Officer Manual
Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Substance Abuse Prevention Medical Review Officer Manual for Federal Agency Workplace Drug Testing Programs EFFECTIVE OCTOBER 1, 2010 Note: This manual applies to Federal agency drug testing programs that come under Executive Order 12564 dated September 15, 1986, section 503 of Public Law 100-71, 5 U.S.C. section 7301 note dated July 11, 1987, and the Department of Health and Human Services Mandatory Guidelines for Federal Workplace Drug Testing Programs (73 FR 71858) dated November 25, 2008 (effective October 1, 2010). This manual does not apply to specimens submitted for testing under U.S. Department of Transportation (DOT) Procedures for Transportation Workplace Drug and Alcohol Testing Programs (49 CFR Part 40). The current version of this manual and other information including MRO Case Studies are available on the Drug Testing page under Medical Review Officer (MRO) Resources on the SAMHSA website: http://www.workplace.samhsa.gov Previous Versions of this Manual are Obsolete 3 Table of Contents Chapter 1. The Medical Review Officer (MRO)........................................................................... 6 Chapter 2. The Federal Drug Testing Custody and Control Form ................................................ 7 Chapter 3. Urine Drug Testing ...................................................................................................... 9 A. Federal Workplace Drug Testing Overview.................................................................. -
Quantitative Drug Test Menu Section 2
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Substance Abuse in the Workplace Policy
Substance Abuse in the Workplace Policy Rexnord (herein referred to as “Rexnord” or the “Company”) has a strong commitment to its employees to provide a safe work environment and to promote high standards of employee performance. Consistent with the spirit and intent of this commitment, the Company has established a policy regarding substance abuse in the workplace. Further, the Company is committed to maintaining a drug-free workplace as required by “The Drug-Free Workplace Act of 1988.” Therefore, compliance with this Policy is a condition of continued employment with Rexnord. I. PURPOSE To outline the procedures to be followed by each location in order to ensure that the safety and performance of employees is not impaired by alcohol, illegal drugs or other substances. II. APPLICABILITY This policy shall apply to all employees (full-time, part-time, exempt, and non-exempt employees) as well as to all applicants who have received a conditional offer of employment. Personnel who perform their services on Company property or on a third party’s property at the request of the Company (e.g., a Company customer site), as provided under a contract either directly with the Company or through the services of an outside firm, are required to abide by this policy. It is the responsibility of the contracting firm (at its cost and expense) to ensure that its personnel are tested in conformance with this policy prior to working at / on behalf of Rexnord. III. SUBSTANCE ABUSE It is the Company’s policy that the following is prohibited and will result in discipline up to and including termination: A. -
Drug & Alcohol Testing Be a Driver in the Know
Controlled Substances Consequences FEDERAL The regulations require 5-panel testing for the 3 A positive test result or a following classes of substances: refusal requires the driver to be immediately removed from Drug & Marijuana n operating any CMV on public n Cocaine roadways. The employer must provide you with a list of Alcohol n Opiates — opium and acceptable SAPs from which to codeine derivatives choose to begin the “return-to- ” n Amphetamines and duty process. This process must Testing meth amphetamines be completed before a positive or REGULATIONS refusal driver can legally return to n Phencyclidine — PCP driving CMVs for any employer, including himself. For more information, visit www.usdoj.gov/dea/concern 3 The impact of testing positive or refusing to test can be devastating for a driver and his family. It often results in extended periods of unemployment, due to the time necessary to complete the “return-to-duty” process with a qualified SAP and the tendency of employers not to hire drivers with drug or alcohol histories. 3 Even after completing the “return- to-duty” process and finding employment, the additional return- to-duty and follow-up testing often adds increased stress and financial strain on the driver. For additional research and reading on the Federal Motor Carrier Safety Administration’s Drug and Be a Alcohol Testing Regulations, please visit our web site at: www.fmcsa.dot.gov/ Driver In rules-regulations/topics/drug/drug.htm the Know... FMCSA-E-06-003 Revised July 2010 The U.S. Department of Transportation (DOT) whenever they are involved in a fatal accident, or professional (SAP) drug and alcohol testing regulations for receive a traffic citation resulting from an injury or who signs the return- commercial driver licensed (CDL) employees are vehicle-disabling accident. -

Ncaa Drug Policies
MEDICAL EXCEPTIONS APPEALS The NCAA recognizes that some banned substances The NCAA drug-testing program allows an are used for legitimate medical purposes. According- institution to appeal a positive drug test on behalf ly, the NCAA allows exception to be made for those of a student-athlete who has tested positive or who student-athletes with a documented medical history violated NCAA drug-testing protocol. demonstrating the need for regular use of such a drug. Exceptions may be granted for substances • The institution must submit in writing the included in the following classes of banned drugs: grounds for the appeal and a summary of the stimulants (including those used to treat ADHD), institutional drug-education program. beta blockers, beta-2 agonists, diuretics, peptide • At least three members of the drug- hormones, anabolic agents and anti-estrogens. education and drug-testing subcommittee of the • Pre-approval is required for the use of peptide NCAA Committee on Competitive hormones or anabolic agents. The institution Safeguards and Medical Aspects of Sports must submit required documents to the NCAA (CSMAS) hear appeals. ([email protected]) prior to the student-athlete competing while using medications containing • Appeals are conducted by telephone these substances. conference. • For all other drug classes, the institution should • The director of athletics or designee and the maintain documents from the prescribing student-athlete must be on the appeal call. physician in the student-athlete’s medical record on campus that include the diagnosis, course of • The NCAA does not restrict the nature of the treatment and current prescription. appeal, that is to say that the NCAA will not restrict access for any reason to an institution that wishes • In the event that a student-athlete tests positive to appeal and has satisfied the appeal procedures. -

Frequently Asked Questions About Marijuana
Frequently Asked Questions Marijuana Q: What is marijuana? A: Marijuana is the product of the hemp plant, Cannabis sativa, containing the psychoactive chemical delta-9-tetrahydrocannabinol (THC) and other related compounds. Popular names/slang for the drug include weed, pot, or cannabis. Q: How do people use marijuana? A: Marijuana is typically smoked using rolled paper cigarettes (joints), pipes, water pipes (bongs), and vaporizers. However, the drug is also mixed into edibles and drinks and extracted into oils and waxes. Q: How does marijuana affect users? A: Marijuana use impacts the human body both physically and mentally. The “high” from the drug can include distorted senses, impaired judgment, lack of balance and coordination, increased appetite, elevated heart rate, and sometimes anxiety and panic. Q: How many people use marijuana? A: Below is the most current data estimating marijuana use. • The National Survey on Drug Use and Health (NSDUH) reports more than 26 million Americans aged 12 or older, or 9.6% of the total population, were current users of marijuana in 2017. • The World Drug Report 2019 estimates that there were 188 million global cannabis users in 2017. • Marijuana comprised the most common substance use disorder, impacting an estimated 4.1 million Americans in 2017, according to the NSDUH. Q: Can an employer drug test for marijuana? A: Yes. There are currently no restrictions (other than New York City which is expected to implement restrictions beginning in May 2020) limiting an employer’s ability to drug test for marijuana, although there may be limitations on permissible disciplinary action that an employer may take if an employee is using marijuana in accordance with that state’s marijuana laws. -
Fact Sheet: Drug Testing in the Criminal Justice System
DOJ/OJP logo, Adobe Illustrator, 11/89 T O EN F J TM U R ST A I U.S. Department of Justice P C E E D B O J C S F A V M F O Office of Justice Programs A I N C I J S R E BJ G O OJJ DP O F PR Bureau of Justice Statistics JUSTICE Drugs & Crime Data March 1992 Fact Sheet: Drug Testing in the Criminal Justice System As part of ongoing research the Drugs & tion hearings. Drug tests in prisons can that a positive immunoassay be retested Crime Data Center & Clearinghouse pre- also assist in monitoring drug use in cor- and confirmed, preferably by a different pared this fact sheet on drug testing in rectional facilities and by inmates during technique of equal or greater sensitivity, the criminal justice system. “Drug test- temporary absences from the institution. such as gas chromatography/mass ing” in this fact sheet refers to urinalysis, spectrometry.4 ● Identify persons in need of treatment. since that is the testing methodology Drug tests can identify drug users who Chromatography involves separating typically used throughout the criminal can be placed in treatment. Drug testing and identifying the components of a justice system. is also used to monitor persons undergo- specimen. GC/MS (gas chromatogra- ▲ ing drug treatment. phy/mass spectrometry) is considered to Who is tested? be “the most legally defensible” method ▲ Drug testing can take place in all stages Drug testing technology of urinalysis.5 GC/MS testing, however, of the criminal justice system: arrest, in is more expensive than immunoassay There are two primary methods of the pretrial phase, and during incarcera- testing (typically between $25 and $100 detecting drugs in the urine: immunoas- tion, probation, and parole. -
Mandatory Drug and Alcohol Testing (MDAT) Frequently Asked Questions
Mandatory Drug and Alcohol Testing (MDAT) Frequently Asked Questions Why is drug and alcohol testing required? Individuals seeking employment in “safety-sensitive” positions shall be subject to drug testing. Per the Child and Youth, Safety and Health Omnibus Amendment Act of 2004 (D.C. Law 15-353, D.C. Official Code § 1-620.31 et seq.), a “safety- sensitive” position is defined as “employment in which the District employee has direct contact with children or youth; is entrusted with the direct care and custody of children or youth; and whose performance of his or her duties in the normal course of employment may affect the health, welfare, or safety of children or youth.” Who is subject to testing? All employees in school-based positions, both instructional and non-instructional, are subject to testing. Which substances does DCPS test for? The drug test is used to determine the presence of the following illegal drugs/controlled substances – marijuana, cocaine, opiates, amphetamines, and phencyclidine. Employees are also tested for the presence of alcohol. Are employees required to disclose to DCPS any prescription medications that they are taking? If the results are positive, you will receive a call from The Medical Review Officer (MRO). The MRO will contact you to determine whether there is a legitimate reason for the positive test, and that’s where you will present your prescription. The MRO will then contact the employee’s physician to verify the prescription. If you are currently registered in a medical marijuana program, please send that evidence to the DCPS Mandatory Drug and Alcohol Testing program at [email protected]. -

Chronic Opioid Therapy in Chronic Noncancer Pain
Guidelines on Use of Long-term Opioid Therapy for Chronic Non- cancer Pain Roger Chou, MD Associate Professor of Medicine Oregon Health & Science University Director of Clinical Guidelines Development, the American Pain S o c i e t y Acknowledgments APS/AAPM Opioids Panel: Perry Fine (co-c hair), Gilbert Fanciullo (co-chair), Chris Miaskowski (APS Guidelines chair), Jeremy Adler, Jane Ballantyne, Pam Davies, Marilee Donovan, David Fishbain, Kathy Foley, Jeff Fudin, Aaron Gilson, Alex Kelter, Alexander Mauskop, Patrick O’Connor, Steve Passik, Gavril Pasternak, Russell Portenoy, Ben Rich, Richard Roberts, Knox Todd OHSU EPC Pain Project Team: Laurie Huffman, Michelle Pappas, Jayne Schablaske, Tracy Dana Conflict of interest disclosure Dr. Chou has received research funding from the Agency for Healthcare Research and Quality and the Drug Effectiveness Review Project, and has received honoraria from the American Pain Foundation Purpose • Understand evidence-based guidelines for risk assessment to guide patient selection for opioids • Understand evidence-based guidelines for initiation and titration of long-term opioid therapy • Understand evidence-based guidelines for monitoring of patients on long-term opioid therapy Background • Chronic noncancer pain is highly prevalent, with substantial burdens • Opioids are increasingly prescribed for chronic noncancer pain • Opioids are associated with potential harms, both to patients and to society • Lack of guidelines based on a rigorous evidence - based process • Large practice variations 6 Prescription drug abuse In 2006, nearly 7 million Americans estimated to be abusing prescription drugs Prescription opioids cause more drug overdose deaths than cocaine and heroin combined Overdose deaths often associated with use of multiple opioids and/or illicit substances Nearly 1 in 10 high school seniors admit to abusing prescription painkillers. -
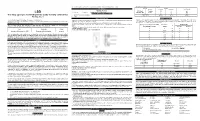
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

Drug Testing in the Era of Legalized Marijuana and CBD
Drug Testing in the Era of Legalized Marijuana and CBD Patti Darbishire, PharmD Associate Dean Purdue University College of Pharmacy Bruce Mueller, PharmD Associate Dean University of Michigan College of Pharmacy Tom TenHoeve, PhD Associate Dean University of Illinois-Chicago Conflict of Interest Disclosure Patti Darbishire, Bruce Mueller and Tom Tenhoeve have no conflict of interests or relevant financial relationships with a commercial interest pertaining to the content of this presentation. Objectives By the end of this program, participants will be able to: 1. Describe pharmacy students’ risk for substance abuse and perspectives on drug screening. 2. Describe the College responsibilities to sites, students, and society about marijuana use in a state where it has been “legalized”. 3. Describe the changes necessary for an established drug testing policy to maintain its integrity in an era of legalized recreational marijuana. Is this really a problem for our for students? National Survey of Drug Use and Health Self-reports from college-age adults Aged 21-25, legally use • 68% ALCOHOL • 32% TOBACCO Aged 18-25, Illicit Drug Use (23%) • 21% MARIJUANA • 5% RX DRUGS FOR ILLICIT USE • e.g., stimulants, opioids, benzodiazepines • 2% HALLUCINOGENS • 2% COCAINE https://www.samhsa.gov/data/sites/default/files/NSDUH -DetTabs-2016/NSDUH-DetTabs-2016.htm#tab1-7B. Accessed 4.29.18 Substance Use by Student Pharmacists Hazardous and/or illicit use of: Alcohol (25-36%) Tobacco (5-58%) • 2016 review of 16 articles Marijuana (6-33%) published between 1985- Stimulants (3-19%) 2014 at University of Cocaine (3-7%) Georgia Sedatives (3-9%) Opioids (8-15%) • Summarizes findings of Heroin (<3%) student pharmacists’ use Hallucinogens (3-14%) of illicit substances *Ranges are indicative of study age and report of current or lifetime use https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5221842/. -

Marijuana Please Read All the Information in This Package Insert Before Performing the Test
PROFESSIONAL DRUG TEST DrugTest Marijuana Please read all the information in this package insert before performing the test. The Drug Test Marijuana Rapid Test Cassette (Urine) is a rapid urine screening test that can be performed without the use of expensive instruments. The test utilizes a monoclonal antibody to selectively detect elevated levels of marijuana in urine. The THC Rapid Test Cassette yields a positive result when the concentration of marijuana in urine exceeds 50ng/ml. This assay provides a preliminary analytical test result. A more specific alternate chemical method must be used to obtain a confirmed analytical result. Gas chromatography/mass spectrophotometry (GC/MS) is the preferred confirmatory method. Clinical consideration and professional judgment should be applied to any drug of abuse test result, particularly when preliminary positive results are used. THC (Δ9-tetrahydrocannabinol) is the primary active ingredient in cannabinoids (marijuana). When smoked or orally administered, it produces euphoric effects. Users have impaired short term memory and slowed learning. Users may also experience transient episodes of confusion and anxiety. Long term relatively heavy use may be associated with behavioural disorders. The peak effect of smoking marijuana occurs in 20-30 minutes and the duration is 90-120 minutes after one cigarette. Elevated levels of urinary metabolites are found within hours of exposure and remain detectable for 3-10 days after smoking. The main metabolite excreted in the urine is 11-nor-Δ9-tetrahydrocannabinol-9- carboxylic acid (Δ9-THC-COOH). PRECAUTIONS • Do not use after the expiration date. • The test should remain in the sealed pouch until use. SPECIMEN COLLECTION AND PREPARATION • The urine must be collected in a clean and dry container.