Transplant Chronicles
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of Intuitive Knowledge in the Diagnostic Reasoning of Hospital Specialists: a Focus Group Study
Open access Research BMJ Open: first published as 10.1136/bmjopen-2018-022724 on 28 January 2019. Downloaded from Role of intuitive knowledge in the diagnostic reasoning of hospital specialists: a focus group study Nydia Van den Brink,1 Birgit Holbrechts,1 Paul L P Brand,2 Erik C F Stolper,1,3 Paul Van Royen3 To cite: Van den Brink N, ABSTRACT Strengths and limitations of this study Holbrechts B, Brand PLP, et al. Background and objective Intuition is an important part Role of intuitive knowledge of human decision-making and can be explained by the ► This is the first study exploring the role of intuition in in the diagnostic reasoning dual-process theory where analytical and non-analytical of hospital specialists: a hospital specialists’ diagnostic reasoning. reasoning processes continually interact. These processes focus group study. BMJ Open ► The study was performed in two European countries. can also be identified in physicians’ diagnostic reasoning. 2019;9:e022724. doi:10.1136/ ► The used qualitative approach enabled the re- The valuable role of intuition, including gut feelings, has bmjopen-2018-022724 searchers to study the views of specialists on the been shown among general practitioners and nurses, but topic and the meanings they attach to the concept. ► Prepublication history for less is known about its role among hospital specialists. ► It was not the aim of the researchers to gather data this paper is available online. This study focused on the diagnostic reasoning of hospital To view these files, please visit for the calculation of predictive values of intuitive specialists, how they value, experience and use intuition. -

Full Version of Cv
Adrian David Cheok AM Phone: +61423977539 or +60128791271 19A Robe Terrace Email: [email protected] Medindie, 5081 Homepage: https://www.adriancheok.info Australia https://www.imagineeringinstitute.org Personal Date of Birth: December 18, 1971. Place of birth: Adelaide, Australia Australian Citizen. Summary of Career Adrian David Cheok AM is Director of the Imagineering Institute, Malaysia, Full Professor at i-University Tokyo, Visiting Professor at Raffles University, Malaysia, Visiting Professor at University of Novi Sad-Serbia, on Technical faculty \Mihailo Pupin", Serbia, Faculty of Ducere Business School, and CEO of Nikola Tesla Technologies Corporation. He is Founder and Director of the Mixed Reality Lab, Singapore. He was formerly Professor of Pervasive Computing, University of London, Full Professor and Executive Dean at Keio University, Graduate School of Media Design and Associate Professor in the National University of Singapore. He has previously worked in real-time systems, soft computing, and embedded computing in Mitsubishi Electric Research Labs, Japan. In 2019, The Governor General of Australia, Representative of Her Majesty the Queen Elizabeth II, has awarded Australia's highest honour the Order of Australia to Adrian David Cheok for his contribution to international education and research. He has been working on research covering mixed reality, human-computer interfaces, wearable computers and ubiquitous computing, fuzzy systems, embedded systems, power electronics. He has successfully obtained approximately $130 million dollars in funding for externally funded projects in the area of wearable computers and mixed reality from Daiwa Foundation, Khazanah National (Malaysian Government), Media Development Authority, Nike, National Oilwell Varco, Defence Science Technology Agency, Ministry of Defence, Ministry of Communications and Arts, National Arts Council, Singapore Sci- ence Center, and Hougang Primary School. -

Doctor Who: Frayed
FRAYED Tara Samms First published in England in 2003 by Telos Publishing Ltd 61 Elgar Avenue, Tolworth, Surrey KT5 9JP, England www.telos.co.uk ISBN: 1-903889-22-7 (standard hardback) Frayed © 2003 Tara Samms Foreword © 2003 Stephen Laws Icon © 2003 Nathan Skreslet ISBN: 1-903889-23-5 (deluxe hardback) Frayed © 2003 Tara Samms Foreword © 2003 Stephen Laws Frontispiece © 2003 Chris Moore Icon © 2003 Nathan Skreslet The moral rights of the author have been asserted 'DOCTOR WHO' word mark, device mark and logo are trade marks of the British Broadcasting Corporation and are used under licence from BBC Worldwide Limited. Doctor Who logo © BBC 1996. Certain character names and characters within this book appeared in the BBC television series 'DOCTOR WHO'. Licensed by BBC Worldwide Limited Font design by Comicraft. Copyright © 1998 Active Images/Comicraft 430 Colorado Avenue # 302, Santa Monica, Ca 90401 Fax (001) 310 451 9761/Tel (001) 310 458 9094 w: www.comicbookfonts.com e: [email protected] Typeset by TTA Press, 5 Martins Lane, Witcham, Ely, Cambs CB6 2LB, England w: www.ttapress.com e: [email protected] Printed in England by Antony Rowe Ltd, Bumper's Farm Industrial Estate, Chippenham, Wilts SN14 6LH 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 British Library Cataloguing in Publication Data. A catalogued record for this book is available from the British Library. This book is sold subject to the condition that it shall not by way of trade or otherwise, be lent, resold, hired out or otherwise circulated without the publisher's prior written consent in any form of binding or cover other than that in which it is published and without a similar condition including this condition being imposed on the subsequent purchaser. -

New Media for New Organs: a Virtual Community For
462-469 CON342344 Bers_CON 170x242mm 06/10/2009 16:29 Page 462 Convergence: The International Journal of Research into New Media Technologies Copyright © The Author(s), 2009. Reprints and permissions http://www.sagepub.co.uk/journalsPermissions.nav FEATURE REPORT London, Los Angeles, New Delhi, Singapore, and Washington DC Vol 15(4): 462–469 DOI: 10.1177/1354856509342344 http://con.sagepub.com New Media for New Organs A Virtual Community for Pediatric Post-Transplant Patients Marina U. Bers Tufts University, USA Abstract / This article describes an eight-month pilot study in which 19 pediatric post-transplant patients at Children’s Hospital Boston, ages 11 to 15, used a computer-based psychosocial inter- vention developed on the Zora 3D multiuser environment. Zora provides tools to create an online virtual city and populate it with houses and personally-meaningful objects. Users can communicate with each other via real-time chat and participate in open-ended guided activities to create a social network of peers. Preliminary results support the idea that innovative technologies can help adoles- cent patients to create a support network of peers when face-to-face interactions are impossible. Key Words / children’s virtual community / health care / multi-user virtual environment / online games / real-time chat Introduction New media is having an impact in the way children learn, play and communicate. From video-games to virtual tutors, from I-pods to on-line shopping, today’s children are immersed in a culture in which computers and the internet are vastly used for most of their needs (Subrahmanyam et al., 2001). Most recently, these needs have also started to expand to health care. -

World Series of Cars
FREEFREE WWEEEEKLYKLY The People’s Paper. A Division of Chautauqua Marketing Solutions • Vol: 03, Number: 29 • July 22, 2013 World Series of Cars - A Home Run Every Year Editor Walter Pickut with Krista Bellardo The World Series of Cars returns on July 28 to team up with Jamestown’s Babe Ruth World Series. The Chautauqua Lake Dine on the Lake Region Antique Automobile Club of America (AACA), founded Serving Lunch & Dinner in 1957, will once again host this famous car show in Jamestown’s 11:30 am - 9:30 pm (May - Oct.) 716-753-2900 Bergman Park. 2013 is the 26th year of their sponsorship. Great Steaks, Fresh Seafood The national AACA, founded in 1935, is now the largest antique Signature Salads automobile club in the world, with more than 50,000 members in Pastas & Sandwiches all 50 states and more than 50 countries. Homemade Desserts 188 S. Erie Street (Rte. 394) World Series of Cars and the City of Jamestown help raise Mayville, NY 14757 revenue for the Babe Ruth World Series. “When the show is all watermarkrestaurant.net Organization and Der Kobblers. over and the dust is cleared we turn over a check to the World Mention this ad for “The oldest car we’ve ever seen here was a 1902 Ford,” said Russ 15% off on entree Series of Baseball,” Frank Tantillo, CLRAACA Club President, explained. Diedrick, AACA committee member and 1997 Babe Ruth Hall of Famer. “Many of the other cars will be from the early 1900s.” “We have been a part of the World Series of Cars in Jamestown for many years. -

Nicole Marie Psaltis, O.D. WJB Dorn VAMC, Columbia SC Residents Day Proposal August 30, 2010
Nicole Marie Psaltis, O.D. WJB Dorn VAMC, Columbia SC Residents Day Proposal August 30, 2010 • Abstract ‐ Retinitis pigmentosa (RP) is a group of inheritable eye conditions, constituting retinal and RPE dystrophies, which progress to vision loss. Patients with identical genetic mutations can manifest different phenotypic presentations. This case describes an atypical presentation of RP. • Case History ‐ A 57‐year‐old Caucasian male veteran presented to the Wm. Jennings Bryan Dorn VA Eye Cinic in Columbia, South Carolina on June 23, 2009 ‐ Chief Complaint Decreasing peripheral field of vision The patient had a secondary complaint of painless blurred vision distance and near of gradual onset ‐ Ocular History Hyperopic astigmatism OU Unremarkable ocular health history per patient’s account Last eye exam was 2.5 years ago ‐ Medical History Alcohol abuse Esophageal reflux Hypercholesterolemia Hypothyroidism Depression PTSD Substance Abuse ‐ Medications Citalopram Hydrobromide Hydrochlorothiazide Nicotine Patch Omeprazole Simvastatin Trazodone ‐ Allergies Naproxen ‐ Family Ocular History Unremarkable ‐ Pertinent Findings Entering VA: 20/25+2 OD, 20/25 OS cc Pupils: PERRL (‐) APD EOM: FROM OU CVF: Constricted OU Subjective Refraction: +2.00‐2.00x109 OD +2.25‐1.25x065 OS Anterior Segment Evaluation: WNL OU Tap: 13 mmHg OD, 14 mmHg OS @ 1109 AM DFE: Atrophic presentation with distinct cessation perifoveally OU. Coalesced hyperplastic lesions, rarely in bone spicule appearance, scattered throughout posterior pole OU. Scattered areas of atrophy of scalloped appearance in far periphery to ora serrata. Vessels are mildly narrow and attenuated OU. Maculae were flat and intact OU. The optic nerve cup‐to‐disc ratios are 0.10, round OU. The presentation is symmetrical. -
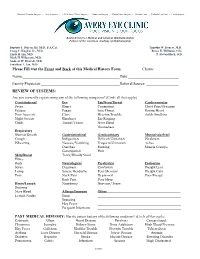
Please Fill out the Front and Back of This Medical History Form. Chart#: Name: Date: Family Physician: Referral Source: REVI
Advanced Cataract Surgery • Lens Implants • LASIK Laser Vision Surgery • Glaucoma Surgery • Retina Laser Surgery • Contact Lens • Pediatric Eye Care • Eyelid Surgery Board-Certifie d Medical and Surgical Ophthalmologists Fellows of the American Academy of Ophthalmology Baptiste J. Dejean, III, M.D., F.A.C.S. Timothy W. Doucet, M.D. Craig C. Kuglen, Jr., M.D. Renee E. Williams, O.D. Linda H. Lin, M.D. P. Steven Black, O.D. Mark H. Wilkerson, M.D. Andrew W. Dvorak, M.D. Jonathan T. Jan, M.D. Please Fill Out the Front and Back of this Medical History Form. Chart#: Name: Date: Family Physician: Referral Source: REVIEW OF SYSTEMS: Are you currently experiencing any of the following symptoms? (Circle all that apply) Constitutional Eye Ear/Nose/Throat Cardiovascular Fever Blurry Congestion Chest Pain/Pressure Fatigue Foggy Sore Throat Racing Heart Poor Appetite Glare Hearing Trouble Ankle Swelling Night Sweats Blindness Ear Ringing Chills Tunnel Vision Nose Bleed Hoarseness Respiratory Short of Breath Gastrointestinal Genitourinary Musculoskeletal Cough Indigestion Difficult Urination Weakness Wheezing Nausea/Vomiting Frequent Urination Aches Diarrhea Burning Muscle Cramps Constipation Pain Skin/Breast Tarry/Bloody Stool Hives Rash Neurological Psychiatric Endocrine Sores Dizziness Confusion Weight Loss Lump Severe Headache Poor Memory Weight Gain Pain Neck Pain Depressed Poor Energy Back Pain Poor Sleep Heme/Lymph Numbness Nervous/Tense Bruising Nose Bleed Allergy/Immune Other: Lymph Nodes Sinus Sneezing Hay Fever Frequent Infections PAST MEDICAL HISTORY: Has the patient had any of the following conditions? (Circle all that apply) Cataracts Ulcer Heart Disease Paralysis Cancer (type): Glaucoma Jaundice Kidney Stone Drug Addiction High Blood Pressure Hay Fever Gallstone Bladder Trouble Prostate Trouble Tuberculosis Asthma Liver Disease Thyroid Disease Nerve Disease Anemia Diabetes Hepatitis Stroke Muscle Disease Bleeding Disorder Pneumonia Colitis Infections Seizure High Cholesterol (over) OTHER EYE OR MEDICAL PROBLEM: Eye/Medical Issue Date Eye/Medical Issue Date 1. -
Setting High Standards of Care for Low Vision
Low Vision Treatment Setting High Standards of Care for Low Vision www.neoretina.com Thousands of Indians suer from low vision. Are you one among them? Low Vision is a condition of visual impairment that cannot be corrected through glasses, medicines or surgical treatments. The condition is often characterized by partial sight, blurred vision, tunnel vision or blind spots. Low vision impacts both adults and children but mostly occurs among adults above 60 years of age. Losing the ability to perform basic activities: drive, read, watch or view, etc. can make one feel shut o from living a normal life. What causes low vision? Generally, the low vision condition is caused by eye diseases or health conditions such as Age-related Macular Degeneration (AMD), Cataract, Diabetic Retinopathy, Retinitis Pigmentosa, Stargardt's Disease (juvenile Macular Degeneration) and Glaucoma. Eye injuries, congenital disabilities and brain damages are some other causes. The chances to restore eyesight due to low vision are unlikely, but it can be managed with proper devices and vision rehabilitation. How do you know if you have low vision? A person with low vision condition has poor eyesight, where he is unable to perform routine duties, despite regular glasses, medicine, and surgery. Commonly individuals with low vision can have diculty in: Reading and writing Using a Computer/Tablet or watching Reading trac signals, Television name boards, etc. Spotting switches, dials or other Recognizing familiar faces mechanical controls Neoretina: Comprehensive & Technologically Enhanced Centre for Low Vision Treatment Neoretina Eyecare Institute, Hyderabad oers world-class treatment in the management of the low vision and other eye conditions. -

Frequency of Low Vision Patient and Their Causes Presenting in Madinah Teaching Hospital, Pakistan
Advances in Ophthalmology & Visual System Research Article Open Access Frequency of low vision patient and their causes presenting in Madinah Teaching Hospital, Pakistan Abstract Volume 9 Issue 6 - 2019 Aim: The aim of our study to determine the frequency of low vision patient and their causes presenting in Madinah Teaching Hospital. Fatima Iqbal,1 Iqra Khalil,1 Hafiza Ayesha Khalil,2 Mariam Sadiq,3 Hafiza Azka Noor,3 Methods: 400 patients were screened in the duration of five month from JAN to MAY Mawra Zahid 2019.80 subjects were taken as a low vision patient according to WHO, whose visual 1 acuity was less than 6/18 with correction. The main causes of low vision were observed Lecturer in School of Optometry, University of Faisalabad, Pakistan high refractive errors, retinitis pigmentosa, cataract, glaucoma and diabetic retinopathy all 2Optometrist, Fred Hollow Foundation, Pakistan patients presenting in ophthalmology department with either gender and age ranging from 3Optometrist, LRBT Toba Tek Singh, Pakistan 10-80 years. Uncooperative and mentally retarded persons were excluded in our study. 4Demonstrator, University of Lahore, Pakistan After complete history, we examined the all individual’s visual acuity with log-mar chart, color vision with ishihara and contrast sensitivity with Pelli-robson chart. Data was entered Correspondence: Fatima Iqbal, Lecturer in School of in to SPSS latest version and analyzed by descriptive analysis. Optometry, University of Faisalabad, Pakistan, Tel 03315538865, Email [email protected] Results: -

K Robinson, M Byers. Diving Medicine
J R Army Med Corps 2005; 151: 256-263 J R Army Med Corps: first published as 10.1136/jramc-151-04-07 on 1 December 2005. Downloaded from Diving Medicine K Robinson, M Byers with diving. This article aims to review the physics and physiology of diving, discuss the common medical conditions that occur whilst diving, and consider the current thinking in relation to aetiol- ogy and treatment. A Brief History of Diving Breath-hold diving has probably been around from before written history. Divers were reportedly used in the Trojan Wars (1194-1184 BC) to disrupt the enemy navies. Aristotle described ruptured tympan- ic membranes and ear infections in sponge divers, and Marco Polo wrote of pearl divers reaching depths of 27 metres. Alexander the Great is supposed to have made a dive in a primitive diving bell, Roger Bacon described men walking on the seabed in 1240, and in 1535 Guglielmo de Lorena developed the first true diving bell (3). In 1774 Freminet used a bellows to deliv- er air from the surface to a diver and Siebe Introduction developed the diving suit in 1819 (3). This It could be argued that diving is the most consisted of a copper helmet and jacket, extreme sport of all. Survival in such a which was modified in 1839 to resemble the hostile underwater environment is waterproof suit recognised and in regular use http://militaryhealth.bmj.com/ dependent on sophisticated breathing to the present day. apparatus and an understanding of the Self-contained underwater breathing inherent risks. Diving incidents are well apparatus (SCUBA) was also developed in publicised, not least because of the the 19th century and in 1943 Jacques severe injuries that ensue, but remain an Cousteau and Emile Gagnan demonstrated uncommon occurrence. -

American Squares Vol. 19, No. 10
.■111■1.1■1, RMERICRN JUNE 1964 mimes 19th ANNIVERSARY YEAF S mist 1$ goyim DANCING HERBIE GAUDREAU A MODEL VP-20 the most versatile portable available 20 watt output • 2 mike jacks 29 thru 86 R.P.M. • Radio 8 tape jacks G.E. Cartridge • Special features ... MONITOR OUTPUT Write for specification sheet List Price: 5184.20 ONLY $140." PREPAID ANYWHERE IN U.S. OR A.P.O. ADDRESS IF CHECK ACCOMPANIES ORDER. BOGEN VP 40 UNIQUE VARIABLE SPEED CONTROL HIGH-FIDELITY REPRODUCTION. PROFESSIONAL CONSTRUCTION. Precision turntable with 40 watt full fidelity amplifier. GE cartridge with dual styli. Compact 2-speaker 12" sound unit that packs easily, is built for long wear. Will cover an armory or your living room ! DANCE RECORD CENTER 1159 BROAD STREET NEWARK 14, NEW JERSEY INSTANT RECORD SERVICE - • 941.-' Ixolopursit QUICK AS A SHOT WELL NOT REALLY! BUT TO GIVE YOU FASTER SERVICE WE WOULD HAVE TO SHOOT THEM AT YOU! Our truck goes to the Post Office every hour to give you this Instant Record Service. 99% of our orders are shipped the same day they are received. We have the biggest AIR MAIL stock of Square and Round Dance Records in the U. S. — over a quarter of a million. Drop in and count 'em NEEDLE sometime. SERVICE FOR EMERGENCY SERVICE YOU MAY PHONE DIAMOND NEEDLE $3. DIAMOND CARTRIDGE $6. AREA CODE (201) 622-0025 AND BY AIR MAIL P.P. RECEIVE PROMPT AIR MAIL SHIPMENT. DANCE RECORD CENTER 1159 BROAD STREET NEWARK 14, NEW JERSEY THIS MONTH SPECIAL FEATURES VOLUME 19 JUNE 1964 8 A Message From the Publisher and NUMBER 10 Editor 10 How To Call a Contra -

The Use of the Bow No
Sermon #1694 Metropolitan Tabernacle Pulpit 1 THE USE OF THE BOW NO. 1694 DELIVERED AT THE THURSDAY EVENING LECTURE, BY C. H. SPURGEON, AT THE METROPOLITAN TABERNACLE, NEWINGTON. “And David lamented with this lamentation over Saul and over Jonathan his son: (Also he bade them teach the children of Judah the use of the bow: behold, it is written in the book of Jasher).” 2 Samuel 1:17, 18. THE translators have acted very properly in inserting the words, “the use of,” for that is what the passage means. But if you read it without those words, the sense is still the same— “He bade them teach the chil- dren of Judah the bow,” that is to say, how to use the bow. In modern times, critics have said that by the expression, “the bow,” is meant the song which David composed. And to sustain their notion, they quote from the Koran of Mahomet in which they tell us that there is a certain chapter called, “the Bow,” and, therefore, David called his song, “the bow,” as if so late an instance of oriental usage was at all to the point. I declare that there is nothing whatever in Scripture to justify the state- ment that the words, “the bow,” can be applied to David’s lament! No doubt, some of the Psalms have titles given to them, but there is never an instance of a Psalm being quoted by its title. It is quoted by its number, never by its name. I accept the passage as our learned transla- tors understood it—David bade them teach the children of Judah the bow.