Abdullah Et Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Problems and Potential of Agriculture for Improving Livelihood in Malakand Division, Pakistan
Pakistan Journal of Agricultural Research Review Article Problems and Potential of Agriculture for Improving Livelihood in Malakand Division, Pakistan Ghani Akbar Climate, Energy and Water Research Institute (CEWRI), National Agricultural Research Centre (NARC), Islamabad, Pakistan. Abstract | Malakand division has rich natural resources, having large potential for agriculture and tourism development, while its strategic location indicates a tendency of increasing importance of this region in the near future. Agriculture, one of the main sources of income of 52% of population of Malakand division, is less profitable due to traditional farming methods. Therefore, this paper is aimed to investigate the key agricultural issues and to identify strategies for utilizing the full potential of agriculture for improving livelihood in this region. This study indicated that climate change induced hazards of land degradation and water scarcity due to frequent floods and droughts, decline in traditional springfed Kuhl (gravity channel) irrigation system, low productivity of crops and horticulture, less productive livestock, large postharvest losses and lack of value addition facilities are the main hurdles in utilizing the full potential of agriculture for achieving improved food security and better livelihood in this region. Lack of government spending and less available research facilities are considered the main hindrance in agricultural development in this region. Therefore, this review study was focussed on identification of strategies for the conservation of natural resources, improvement of crops, horticulture, livestock, postharvest management and farm operation sectors in Malakand division. The study illustrated the potential for agricultural improvement, explored key issues and identified strategies and recommendations for agriculture sustainability and improved food security that may lead to better livelihood in Malakand division of Khyber Pakhtunkhwa (KP). -

Ethnoecological Study of Acacia Modesta of Dargai
African Journal of Agricultural Research Vol. 7(36), pp. 5083-5091, 18 September, 2012 Available online at http://www.academicjournals.org/AJAR DOI: 10.5897/AJAR12.665 ISSN 1991-637X © 2012 Academic Journals Full Length Research Paper Ethnoecological appraisal of Acacia modesta Wall. common tree of dry ecosystem in Pakistan Hassan Sher1*, Ali Aldosari2 and Shabir Ahmad1 1Institute of Plant Sciences and Biodiversity, University of Swat, Pakistan. 2Department of Geography, College of Arts, King Saud University, Riyadh, Saudi Arabia. Accepted 24 August, 2012 Ethnoecological studies on Acacia modesta Wall. (Mimosaceae) growing wild in Dargai area of Malakand District (Pakistan), demonstrated a great demand due to the medicinal value of its flowers oil, gum, resins and sticks for honey bee. The plant as a whole is also valuable as fuel-wood and as construction material for income. Locally, common folk used it as fodder, timber, fencing, and household items and as a source of honey bee production. The tree was found to be abundant in some villages of Dargai area. The frequency being: 35% in Jaban, 15% in Kot, 25% in Mehrdi, 10% in Wartair, and 15% in Qaldara villages of Dargai. Interestingly, a great variation was noticed in the local selling prices of the gum which were also found higher in national as well as international markets. Ecological studies showed that A. modesta trees growing on all ranges of soils including: dry to wet, sandy to calcareous and acidic soils along with association of Olea cuspidata, Ziziphus jujuba, Zizyphus nummularia, and Acacia arabica. Phonological studies revealed all the three stages of trees from juvenile, young and rare older trees, in the region under study. -

Government of Khyber Pakhtunkhwa
GOVERNMENT OF KHYBER PAKHTUNKHWA Public Disclosure Authorized Public Disclosure Authorized Qabail Led Community Support Project (QLCSP) Environmental and Social Management Framework (ESMF) Public Disclosure Authorized December 21, 2019 To be executed By Planning & Development Department (GoKP) Through Public Disclosure Authorized Directorate of Projects under the Merged Areas Secretariat (MAS) EXECUTIVE SUMMARY Introduction The Government of Khyber Pakhtunkhwa (GoKP), through Directorate of Projects Planning & Development Department (DP&DD), intends to implement “Qabail Led Community Support Program (QLCSP”) in Khyber district of merged areas (MA) – the erstwhile Federally Administered Tribal Areas (FATA)1 – and Peshawar and Nowshera districts of KP with the proposed assistance of the World Bank (WB).2 This Environmental and Social Management Framework (ESMF) has been prepared to meet requirements of national legislation of Pakistan and World Bank environmental and social policy requirements to address potential negative impacts from the proposed project. Project Overview Background The Central Asia-South Asia Electricity Transmission and Trade Project (CASA1000) aims to facilitate electricity trade between Central Asia and countries in South Asia by putting in place transmission infrastructure. As part of CASA1000 project, each participating country3 is implementing Community Support Programs (CSPs) to share the benefits associated with the project and to generate support among local communities. Project Area In Pakistan, the CASA1000 transmission line (TL) will pass through approximately 100 kilometer long territory passing through various parts of KP province. The project area accordingly lies in/includes Peshawar and Nowshera districts and Khyber district4 of merged areas (MA). Project Components The Project has four components as briefly described below; and its Project Development Objective (PDO) is “improve access to local infrastructure and strengthen community engagement in the project areas”. -
Technical Assistance Layout with Instructions
Initial Environmental Examination December 2014 PAK: Pakistan Power Transmission Enhancement Program Tranche-IV (220 kV Chakdarra Grid Station and Allied Transmission Line) Prepared by Environment and Social Impact Cell (ESIC), NTDC for the Asian Development Bank. 220 kV Chakdarra Grid Station and Allied Transmission Line IEE TABLE OF CONTENTS EXECUTIVE SUMMARY i 1. INTRODUCTION 1 1.1 Overview 1 1.2 Background 1 1.3 Scope of the IEE Study and Personnel 2 2. POLICY LEGAL AND ADMINISTRATIVE FRAMEWORK 4 2.1 Statutory Framework 4 2.1.1 Pakistan Environmental Protection Act, 1997 4 2.1.2 Pakistan Environmental Protection Agency Review of IEE and EIA Regulations, 2000 4 2.1.3 National Environmental Quality Standards (NEQS) 6 2.1.4 Other Relevant Laws 6 2.2 Structure of Report 6 3. DESCRIPTION OF THE PROJECT 8 3.1 Type of Project 8 3.2 Categorization of the Project 8 3.3 Need for the Project 8 3.4 Location and Scale of Project 9 3.5 Analysis of Alternatives 11 3.5.1 Do Nothing Scenario 11 3.5.2 Alternative Construction Methods 11 3.5.3 Alternative Geometry 11 3.6 Proposed Schedule for Implementation 11 3.7 Construction Material 11 4. DESCRIPTION OF ENVIRONMENTAL AND SOCIAL BASELINE CONDITIONS 13 4.1 Project Area 13 4.1.1 General Characteristics of Project Area 13 4.1.2 Affected Administrative Units 13 4.2 Physical Resources 13 4.2.1 Topography, Geography, Geology, and Soils 13 4.2.2 Climate, Temperature and Rainfall 14 4.2.3 Groundwater and Water Supply 15 4.2.4 Surface Water 15 i 220 kV Chakdarra Grid Station and Allied Transmission Line IEE 4.2.5 Air Quality 16 4.2.6 Noise 16 4.3 Biological Resources 16 4.3.1 Wildlife, Fisheries and Aquatic Biology 16 4.3.2 Terrestrial Habitats, Forests and Protected Species 17 4.3.3 Protected areas / National Sanctuaries 17 4.4 Economic Development 17 4.4.1 Agriculture, Livestock and Industries 17 4.4.2 Energy Sources 18 4.5 Social and Cultural Resources 18 4.5.1 Population Communities and Employment 18 4.5.2 Education and Literacy 19 4.5.3 Cultural Heritage and Community Structure 19 5. -

R Functional 2 345003 BHU BRAH Dargai I
DISTRICT MALAKAND BASIC HEALTH UNITS S.No ID No Inst Name Tehsil/ Class Beds Locality Status 1 345002 BHU ASHAKI Dargai I - R Functional 2 345003 BHU BRAH Dargai I - R Functional 3 345004 BHU HERYANKOT Dargai I - R Functional 4 345005 BHU KHARKAI DHERI Dargai I - R Functional 5 345009 BHU GUNYAR THANA Batkhela I - R Functional 6 345010 BHU KHAR Batkhela I - R Functional 7 345011 BHU MEIKH BAND Batkhela I - R Functional 8 345013 BHU TOTAI Dargai I - R Functional 9 345014 BHU Gari Usman Khel Sum ranizai 1 - R Functional 10 345015 BHU MURA BANDA Swat Ranizai I - R Functional 11 345016 BHU NARI OBU Sum ranizai I - R Functional 12 345017 BHU PIRKHEL Swat Ranizai I - R Functional 13 345018 BHU SHINGRAI Sum ranizai I - R Functional 14 345019 BHU TAND GHOUND AGRA Swat Ranizai I - R Functional 15 345020 BHU WARTAIR Sum ranizai I - R Functional 16 345021 BHU BOOTANO KHAPA THANA Sum ranizai I - R Functional 17 345041 BHU KHARKAI DARGAI Sum ranizai I - R Functional 18 345042 BHU INZARGAI AGRA Swat Ranizai I - R Functional 19 345043 BHU MISHTA AGRA Swat Ranizai I - R Functional 20 345045 BHU WAZIR ABAD DARGAI Sum ranizai I - R Functional DISPENSARIES 1 345022 Civil Dispy: Sadullah khan kalay Sum ranizai I - R Functional 2 345024 Civil Dispy: Null thana Swat Ranizai I - R Functional 3 345025 Civil Dispy Bazdara bala palai Swat Ranizai I - R Functional 4 345026 Civil Dispy Badraga Sum ranizai I - R Functional 5 345027 Civil Dispy: Hero shah Sum ranizai I - R Functional 6 345028 Civil Dispy Manzari Baba Kot Swat Ranizai I - R Functional 7 345029 Civil -
UPDATED CAMPSITES LIST for EECP PHASE-2.Xlsx
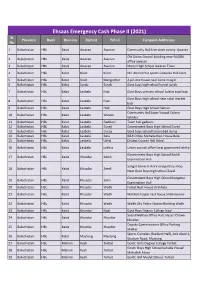
Ehsaas Emergency Cash Phase II (2021) Sr. Province Bank Division Distrcit Tehsil Campsite Addresses No. 1 Balochistan HBL Kalat Awaran Awaran Community Hall Live stock colony Awaran Old Union Council building near NADRA 2 Balochistan HBL Kalat Awaran Awaran office awaran 3 Balochistan HBL Kalat Awaran Awaran Model High School Awaran Town 4 Balochistan HBL Kalat Kalat Kalat Mir Ahmed Yar sports Complex Hall kalat 5 Balochistan HBL Kalat Kalat Mangochar A private house near Jame masjid 6 Balochistan HBL Kalat Surab Surab Govt boys high school hostel surab 7 Balochistan HBL Kalat Lasbela Hub Govt Boys primary school Adalat road hub Govt Boys high school near sabzi market 8 Balochistan HBL Kalat Lasbela Hub hub 9 Balochistan HBL Kalat Lasbela Hub Govt Boys High School Sakran Community Hall Jaam Yousuf Colony 10 Balochistan HBL Kalat Lasbela Winder Winder 11 Balochistan HBL Kalat Lasbela Gaddani Town hall gaddani 12 Balochistan HBL Kalat Lasbela Dureji Government Boys High School Dureji 13 Balochistan HBL Kalat Lasbela Dureji Govt boys school hasanabad dureji 14 Balochistan HBL Kalat Lasbela Bela B&R Office Mohalla Rest House Bela 15 Balochistan HBL Kalat Lasbela Uthal District Council Hall Uthal 16 Balochistan HBL Kalat Lasbela Lakhra Union council office local goverment lakhra Government Boys High School Karkh 17 Balochistan HBL Kalat Khuzdar Karkh Examination Hall Sangat General store and poltary shop 18 Balochistan HBL Kalat Khuzdar Zeedi Near Govt Boys high school Zeedi Government Boys High School Norgama 19 Balochistan HBL Kalat Khuzdar Zehri Examination Hall 20 Balochistan HBL Kalat Khuzdar Wadh Forest Rest House Drakhala 21 Balochistan HBL Kalat Khuzdar Wadh Mohbat Faqeer rest house Shahnoorani 22 Balochistan HBL Kalat Khuzdar Wadh Wadh City Police Station Building Wadh 23 Balochistan HBL Kalat Khuzdar Naal Govt Boys Degree College Naal Social Welfare Office Hall, Hazari Chowk 24 Balochistan HBL Kalat Khuzdar Khuzdar khuzdar. -

Check List of First Recorded Dragonfly (Odonata: Anisoptera) Fauna of District Lower Dir, Khyber Pakhtunkhwa, Pakistan
Arthropods, 2014, 3(2): 120-126 Article Check list of first recorded dragonfly (Odonata: Anisoptera) fauna of District Lower Dir, Khyber Pakhtunkhwa, Pakistan Farzana Perveen1, Anzela Khan2, Sayed Abdul Rauf3 1Departments of Zoology, Shaheed Benazir Bhutto University (SBBU), Main Campus, Sheringal, Khyber Pakhtunkhwa, Pakistan 2Beaconhouse School System, Margalla Campus (BMI-G), H-8, Islamabad, Pakistan 3Departments of Zoology, Shaheed Benazir Bhutto University (SBBU), Main Campus, Sheringal, Khyber Pakhtunkhwa, Pakistan E-mail: [email protected] Received 5 March 2014; Accepted 10 April 2014; Published online 1 June 2014 Abstract The dragonflies (Odonata: Anisoptera) are large, intermediate to small size, having different colours and variable morphological characters. They also carry ornamental and environmental indicator values. The first recorded, the collection of 318 dragonflies was made during May-July 2011 from district Lower Dir, Khyber Pakhtunkhwa, Pakistan. Among them 11 species of dragonflies were identified belonging to 3 families. The golden-ringed, Cordulegaster brevistigma brevistigma Selys is belonging to family Cordulegasteridae and Clubtails, Onychogomphus bistrigatus Selys is belonging to family Gomophidaed. The spine-legged redbolt, Rhodothemis rufa (Rambur); black-tailed skimmer, Orthetrum cancellatum Linnaeus; blue or black-percher, Diplacodes lefebvrei (Ramber); ground-skimmer, Diplacodes trivialis Rambur; common red-skimmer, Orthetrum pruinosum neglectum (Rambur); triangle-skimmer, Orthetrum triangulare triangulare -

Download Download
University of Chitral ISSN: 2616-9150 Journal of Botany |UOCHJB| 2017: Vol. 01:Issue No. 01: Page No.29-44 doi: https://doi.org/10.33195/uochjb-v1i1322017 https://jb.uoch.edu.pk/index.php/j1 Research Paper OPEN ACCESS Floristic Composition and Biological Spectrum of Hazarnoe Forest of District Malakand, Khyber Pakhtunkhwa ASGHAR KHAN*1, NASRULLAH KHAN2 1Degree College Totakan, District Malakand, Khyber Pakhtunkhwa, Pakistan 2Department of Botany University of Malakand, Pakistan *Corresponding author: Email: [email protected] Article Published on: 23 September 2019 Abstract: The plant species of Hazarnoe Forest of District Malakand, Khyber Pakhtunkhwa, were evaluated floristically from April 2016 to November 2017. Of the total 240 reported plant species, 38 were monocots, 196 dicots which belongs to 85 families and 188 genera respectively. Poaceae was the leading family contributed 20 species. Family Asteraceae contributed (14 spp.), Lamiaceae (13 spp.) while Papilionaceae and Solanaceae each with 10 species. Of the total plant taxa perennials were 161 species compared to annuals (73 spp.) and biennials (06 spp.). The dominant growth form was herbs that contributed (108 spp.) followed by trees (50 spp.) and shrubs (45 spp.) respectively. Phanerophytes were the dominant life-form (92 spp.) whereas leaf size spectrum of microphyll was reported as abundant in the overall floristic. Phanerophytes and microphyll leaf size was the dominant life forms which show typical climate of subtropical region governing the area. Conclusion of study was that the vegetation of the area is under heavy biotic pressure and need proper conservation. Keywords— Floristic composition; Life form; Leaf size spectrum 29 University of Chitral Journl of Botany |UOCHJB| INTRODUCTION Floristic composition is reflection of diversity of vegetation of a specific geographic location and provides a platform to plant species for their correct identification and sustainable utilization (Rafay et al., 2013). -

ADP 2021-22 Planning and Development Department, Govt of Khyber Pakhtunkhwa Page 1 of 446 NEW PROGRAMME
ONGOING PROGRAMME SECTOR : Agriculture SUB-SECTOR : Agriculture Extension 1.KP (Rs. In Million) Allocation for 2021-22 Code, Name of the Scheme, Cost TF ADP (Status) with forum and Exp. upto Beyond S.#. Local June 21 2021-22 date of last approval Local Foreign Foreign Cap. Rev. Total 1 170071 - Improvement of Govt Seed 288.052 0.000 230.220 23.615 34.217 57.832 0.000 0.000 Production Units in Khyber Pakhtunkhwa. (A) /PDWP /30-11-2017 2 180406 - Strengthening & Improvement of 60.000 0.000 41.457 8.306 10.237 18.543 0.000 0.000 Existing Govt Fruit Nursery Farms (A) /DDWP /01-01-2019 3 180407 - Provision of Offices for newly 172.866 0.000 80.000 25.000 5.296 30.296 0.000 62.570 created Directorates and repair of ATI building damaged through terrorist attack. (A) /PDWP /28-05-2021 4 190097 - Wheat Productivity Enhancement 929.299 0.000 378.000 0.000 108.000 108.000 0.000 443.299 Project in Khyber Pakhtunkhwa (Provincial Share-PM's Agriculture Emergency Program). (A) /ECNEC /29-08-2019 5 190099 - Productivity Enhancement of 173.270 0.000 98.000 0.000 36.000 36.000 0.000 39.270 Rice in the Potential Areas of Khyber Pakhtunkhwa (Provincial Share-PM's Agriculture Emergency Program). (A) /ECNEC /29-08-2019 6 190100 - National Oil Seed Crops 305.228 0.000 113.000 0.000 52.075 52.075 0.000 140.153 Enhancement Programme in Khyber Pakhtunkhwa (Provincial Share-PM's Agriculture Emergency Program). -
Swat: a Dangerous Flashpoint in the Making
Pakistan Security Research Unit (PSRU) Brief Number 25 Swat: A Dangerous Flashpoint in the Making Syed Adnan Ali Shah Bukhari 6th December 2007 About the Pakistan Security Research Unit (PSRU) The Pakistan Security Research Unit (PSRU) was established in the Department of Peace Studies at the University of Bradford, UK, in March 2007. It serves as an independent portal and neutral platform for interdisciplinary research on all aspects of Pakistani security, dealing with Pakistan's impact on regional and global security, internal security issues within Pakistan, and the interplay of the two. PSRU provides information about, and critical analysis of, Pakistani security with particular emphasis on extremism/terrorism, nuclear weapons issues, and the internal stability and cohesion of the state. PSRU is intended as a resource for anyone interested in the security of Pakistan and provides: • Briefing papers; • Reports; • Datasets; • Consultancy; • Academic, institutional and media links; • An open space for those working for positive change in Pakistan and for those currently without a voice. PSRU welcomes collaboration from individuals, groups and organisations, which share our broad objectives. Please contact us at [email protected] We welcome you to look at the website available through: http://spaces.brad.ac.uk:8080/display/ssispsru/Home Other PSRU Publications The following papers are amongst those freely available through the Pakistan Security Research Unit (PSRU) • Brief number 12. Lashkar-e-Tayyeba • Brief number 13. Pakistan – The Threat From Within • Brief number 14. Is the Crescent Waxing Eastwards? • Brief number 15. Is Pakistan a Failed State? • Brief number 16. Kashmir and The Process Of Conflict Resolution. -
Khyber Pakhtunkhwa Reconstruction Program: Mid-Term Performance Evaluation Report
Khyber Pakhtunkhwa Reconstruction Program: Mid-Term Performance Evaluation Report October 20, 2014 This publication was produced at the request of the United States Agency for International Development by Tariq Husain, Aftab Ismail Khan, David Garner, and Ahmed Ali Khattak. It was prepared independently by Management Systems International (MSI) under the Monitoring and Evaluation Program (MEP). ACKNOWLEDGMENTS The authors would like to express their thanks to all those who facilitated the work of the team and enabled it to complete this evaluation. These include, but are not limited to, the following: Jamshed ul Hasan, Peshawar office Director of the Monitoring and Evaluation Program, who participated in evaluation team meetings, provided information and insight on institutional and infrastructure issues, and facilitated secondary data collection; Maqsood Jan, Shehla Said, and Hina Tabassum, who worked diligently under challenging conditions to collect qualitative data for the evaluation through individual interviews and focus group discussions; Officials of the Provincial Reconstruction, Rehabilitation and Settlement Authority (PaRRSA), Government of Khyber Pakhtunkhwa, who shared their valuable time and insights with the evaluation team, provided a wealth of information through discussion and relevant documents and arranged successful field visits in three districts of Malakand Division; Officials of the Elementary and Secondary Education Department, who provided school-level data from the Education Management Information System; -

Pavement of Goat Walla Irrigationchannel, Thana Bandajat." 333,780
District. Project Description BE 2016-17 MALAKAND MD15D00286-"Pavement of Goat Walla IrrigationChannel, Thana Bandajat." 333,780 MALAKAND MD15D00287-Clearance of silts at Thana Bandajat. 333,780 MALAKAND MD15D00288-"Construction of GI wire, D/wall C/OAriq ur Rehman, Shawi Bund, U/C 278,150 Dheri Julagram." MALAKAND MD15D00291-Pavement of Street at Sultan Khat SaidraJeward U/C GU Khel 222,520 MALAKAND MD15D00292-"Protection wall to agriculture lands atV/C Anar Tangey, U/C GU 222,520 Khel." MALAKAND MD15D00293-Construction of R/Wall VC Palonow U/CHero Shah 111,260 MALAKAND MD15D00294-"Construction of Water channels atTotai, U/C Selai Patay." 166,890 MALAKAND MD15D00295-Construction of R/Wall at Quresh KalayU/C Badraga 139,070 MALAKAND MD15D00296-Construction of R/Wall at Abbas KallayU/C Badraga 166,890 MALAKAND MD15D00297-Construction of Irrigation Channel atQadar Kallai Union Council 111,260 Badraga MALAKAND MD15D00298-Construction of Irrigation Channel atGulo Shah Union Council Koper 278,150 MALAKAND MD15D00299-Construction of R/Wall at U/C SakhakotKhass. 144,630 MALAKAND MD15D00300-"Construction of D/Wall, Slab at JabanBala, near Power House, U/C 166,890 Dargai." MALAKAND MD15D00301-Construction of D/Wall at Saman Abad U/CLower Batkhela District 400,000 Malakand. MALAKAND MD15D00302-"Construction of D/Wall in U/C UpperBatkhela, PK-99, Malakand" 273,000 MALAKAND MD15D00303-Construction of PCC Irrigation ChannelN/H/O Ehsan Ullah U/C Dheri 222,520 Julagram. MALAKAND MD15D00304-Construction of PCC Irrigation channelChena-I U/C Dheri Julagram