Snake and Snakebite Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SINGITA SABI SAND, SOUTH AFRICA for the Month of December, Two Thousand and Fifteen
WILDLIFE REPORT SINGITA SABI SAND, SOUTH AFRICA For the month of December, Two Thousand and Fifteen Temperature Rainfall Recorded Sunrise & Sunset Average minimum: 22˚C (71.6˚F) For the month: 36 mm Sunrise 05:05 Average maximum: 34.2˚C (93.6˚F) For the year to date: 286 mm Sunset 18:46 Minimum recorded: 18◦C (64.4˚F) For the season to date: 173.2 mm Maximum recorded: 41˚C (105.8˚F) With a maximum record of 41˚C, the vegetation has been scorched by the hot conditions. Fortunately with the light rain that we did receive it’s allowed some of the flowering plants to blossom. Here's a highlights package of the month's sightings: Hyenas: It's such a joy when hyena cubs are about - they're curios and like to investigate everything around them. Lions: Lion sightings currently could not get any better! Two male lions of the Matimba coalition have been sighted on a few occasions, and they are gradually expanding their current territorial zone north of the river. The Mhangene pride continue to dominate the central area of Singita Sabi Sand. We watched a few interactions between the Majingalane male lions and the sub-adult males of the Mhangene pride that resulted in the young males being dispersed from the pride temporarily. One of the lionesses from the Mhangene pride has been seen with prominent suckle marks indicating that she has given birth. The lionesses has been seen moving in front of the lodges during the early morning and we suspect that the cubs are hidden in the river just east of Boulders Lodge. -

Snake Charming and the Exploitation of Snakes in Morocco
Snake charming and the exploitation of snakes in Morocco J UAN M. PLEGUEZUELOS,MÓNICA F ERICHE,JOSÉ C. BRITO and S OUMÍA F AHD Abstract Traditional activities that potentially threaten bio- also for clothing, tools, medicine and pets, as well as in diversity represent a challenge to conservationists as they try magic and religious activities (review in Alves & Rosa, to reconcile the cultural dimensions of such activities. ). Vertebrates, particularly reptiles, have frequently Quantifying the impact of traditional activities on biodiver- been used for traditional medicine. Alves et al. () iden- sity is always helpful for decision making in conservation. In tified reptile species ( families, genera) currently the case of snake charming in Morocco, the practice was in- used in traditional folk medicine, % of which are included troduced there years ago by the religious order the on the IUCN Red List (IUCN, ) and/or the CITES Aissawas, and is now an attraction in the country’s growing Appendices (CITES, ). Among the reptile species tourism industry. As a consequence wild snake populations being used for medicine, % are snakes. may be threatened by overexploitation. The focal species for Snakes have always both fascinated and repelled people, snake charming, the Egyptian cobra Naja haje, is undergo- and the reported use of snakes in magic and religious activ- ing both range and population declines. We estimated the ities is global (Alves et al., ). The sacred role of snakes level of exploitation of snakes based on field surveys and may be related to a traditional association with health and questionnaires administered to Aissawas during – eternity in some cultures (Angeletti et al., ) and many , and compared our results with those of a study con- species are under pressure from exploitation as a result ducted years previously. -

Dendroaspis Viridis
Dendroaspis viridis The western green mamba (Dendroaspis viridis), also known as the West African green mamba or Hallowell's green mamba, is a long, thin, and highly venomous snake of the mamba genus, Dendroaspis. This species was first described in 1844 by the American herpetologist Edward Hallowell. The western green mamba is a fairly large and predominantly arboreal species, capable of navigating through trees swiftly and gracefully. It will also descend to ground level to pursue prey such as rodents and other small mammals. The western green mamba is a very alert, nervous, and extremely agile snake that lives mainly in the coastal tropical rainforest, thicket, Scientific Classification and woodland regions of western Africa. Like all the other mambas, the western green mamba is a highly venomous elapid species. Its Kingdom: Anamalia venom is a highly potent mixture of rapid-acting presynaptic and Phylum: Cordata postsynaptic neurotoxins (dendrotoxins), cardiotoxins and fasciculins. Class: Reptilia Some consider this species to not be a particularly aggressive snake, Order: Squamata but others have suggested that they are extremely nervous and are Suborder: Serpentes prone to attack aggressively when cornered. Conflict with humans is Family: Elapidae low compared to some other species found in the region. Bites to Geunus Dendroaspis people by this species are quite uncommon. Their mortality rate, Species D.Viridis however, is high; many of the recorded bites have been fatal. Rapid progression of severe, life-threatening symptoms are hallmarks of Binomial Name mamba bites. Bites with envenomation can be rapidly fatal. Dendroaspis viridis (Hallowell, 1844)[2] Taxonomy Dendroaspis viridis was first described by the American herpetologist and physician Edward Hallowell in 1844.[2][5] In addition to being called the western green mamba, this species is also commonly known as [6] the West African green mamba or Hallowell's green mamba. -

An in Vivo Examination of the Differences Between Rapid
www.nature.com/scientificreports OPEN An in vivo examination of the diferences between rapid cardiovascular collapse and prolonged hypotension induced by snake venom Rahini Kakumanu1, Barbara K. Kemp-Harper1, Anjana Silva 1,2, Sanjaya Kuruppu3, Geofrey K. Isbister 1,4 & Wayne C. Hodgson1* We investigated the cardiovascular efects of venoms from seven medically important species of snakes: Australian Eastern Brown snake (Pseudonaja textilis), Sri Lankan Russell’s viper (Daboia russelii), Javanese Russell’s viper (D. siamensis), Gaboon viper (Bitis gabonica), Uracoan rattlesnake (Crotalus vegrandis), Carpet viper (Echis ocellatus) and Puf adder (Bitis arietans), and identifed two distinct patterns of efects: i.e. rapid cardiovascular collapse and prolonged hypotension. P. textilis (5 µg/kg, i.v.) and E. ocellatus (50 µg/kg, i.v.) venoms induced rapid (i.e. within 2 min) cardiovascular collapse in anaesthetised rats. P. textilis (20 mg/kg, i.m.) caused collapse within 10 min. D. russelii (100 µg/kg, i.v.) and D. siamensis (100 µg/kg, i.v.) venoms caused ‘prolonged hypotension’, characterised by a persistent decrease in blood pressure with recovery. D. russelii venom (50 mg/kg and 100 mg/kg, i.m.) also caused prolonged hypotension. A priming dose of P. textilis venom (2 µg/kg, i.v.) prevented collapse by E. ocellatus venom (50 µg/kg, i.v.), but had no signifcant efect on subsequent addition of D. russelii venom (1 mg/kg, i.v). Two priming doses (1 µg/kg, i.v.) of E. ocellatus venom prevented collapse by E. ocellatus venom (50 µg/kg, i.v.). B. gabonica, C. vegrandis and B. -

The Medical Threat of Mamba Envenoming in Sub-Saharan Africa
Downloaded from orbit.dtu.dk on: Oct 06, 2021 The medical threat of mamba envenoming in sub-Saharan Africa revealed by genus- wide analysis of venom composition, toxicity and antivenomics profiling of available antivenoms Ainsworth, Stuart; Petras, Daniel; Engmark, Mikael; Süssmuth, Roderich D.; Whiteley, Gareth; Albulescu, Laura-Oana; Kazandjian, Taline D.; Wagstaff, Simon C.; Rowley, Paul; Wüster, Wolfgang Total number of authors: 16 Published in: Journal of Proteomics Link to article, DOI: 10.1016/j.jprot.2017.08.016 Publication date: 2018 Document Version Peer reviewed version Link back to DTU Orbit Citation (APA): Ainsworth, S., Petras, D., Engmark, M., Süssmuth, R. D., Whiteley, G., Albulescu, L-O., Kazandjian, T. D., Wagstaff, S. C., Rowley, P., Wüster, W., Dorrestein, P. C., Arias, A. S., M. Gutierrez, J., Harrison, R., Casewell, N. R., & Calvete, J. J. (2018). The medical threat of mamba envenoming in sub-Saharan Africa revealed by genus-wide analysis of venom composition, toxicity and antivenomics profiling of available antivenoms. Journal of Proteomics, 172, 173-189. https://doi.org/10.1016/j.jprot.2017.08.016 General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Users may download and print one copy of any publication from the public portal for the purpose of private study or research. You may not further distribute the material or use it for any profit-making activity or commercial gain You may freely distribute the URL identifying the publication in the public portal If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -
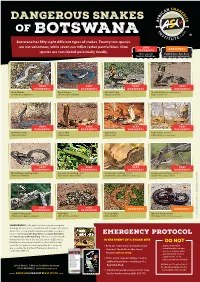
Botswana Has Fifty Eight Different Types of Snakes
DANGEROUS SNAKES OF B OT SWA NA Botswana has fifty eight different types of snakes. Twenty two species are not venomous, while seven can inflict rather painful bites. Nine VERY DANGEROUS species are considered potentially deadly. DANGEROUS Has caused Painful bite, but does human fatalities not require antivenom VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Black Mamba Black Mamba Snouted Cobra Snouted Cobra - banded phase (Dendroaspis polylepis) (Dendroaspis polylepis) (Naja annulifera) (Naja annulifera) VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Anchieta’s Cobra Cape Cobra Cape Cobra Cape Cobra - juvenile (Naja anchietae) (Naja nivea) (Naja nivea) (Naja nivea) Photo Marius Burger VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Mozambique Spitting Cobra Common Boomslang - male Common Boomslang - female Common Boomslang - juvenile (Naja mossambica) (Dispholidus typus viridis) (Dispholidus typus viridis) Photo André Coetzer (Dispholidus typus viridis) VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Southern Twig Snake Puff Adder Horned Adder Bibron’s Stiletto Snake (Thelotornis capensis capensis) (Bitis arietans arietans) (Bitis caudalis) (Atractaspis bibronii) Photo Warren Dick © Johan Marais African Snakebite Institute Snakebite African © Johan Marais JOHAN MARAIS is the author of various books on reptiles including the best-seller A Complete Guide to Snakes of Southern Africa. He is a popular public speaker and offers a variety of courses including Snake Awareness, Scorpion Awareness EMERGENCY PROTOCOL and Venomous Snake Handling. Johan is accredited by the International Society of Zoological Sciences (ISZS) and is a IN THE EVENT OF A SNAKE BITE Field Guides Association of Southern Africa (FGASA) and DO NOT ww Travel Doctor-approved service provider. His courses are 1 Keep the victim calm, immobilized and .. -

Quantitative Characterization of the Hemorrhagic, Necrotic, Coagulation
Hindawi Journal of Toxicology Volume 2018, Article ID 6940798, 8 pages https://doi.org/10.1155/2018/6940798 Research Article Quantitative Characterization of the Hemorrhagic, Necrotic, Coagulation-Altering Properties and Edema-Forming Effects of Zebra Snake (Naja nigricincta nigricincta)Venom Erick Kandiwa,1 Borden Mushonga,1 Alaster Samkange ,1 and Ezequiel Fabiano2 1 School of Veterinary Medicine, Faculty of Agriculture and Natural Resources, Neudamm Campus, University of Namibia, P. Bag 13301, Pioneers Park, Windhoek, Namibia 2Department of Wildlife Management and Ecotourism, Katima Mulilo Campus, Faculty of Agriculture and Natural Resources, University of Namibia, P. Bag 1096, Ngweze, Katima Mulilo, Namibia Correspondence should be addressed to Alaster Samkange; [email protected] Received 30 May 2018; Revised 5 October 2018; Accepted 10 October 2018; Published 24 October 2018 Academic Editor: Anthony DeCaprio Copyright © 2018 Erick Kandiwa et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Tis study was designed to investigate the cytotoxicity and haemotoxicity of the Western barred (zebra) spitting cobra (Naja nigricincta nigricincta) venom to help explain atypical and inconsistent reports on syndromes by Namibian physicians treating victims of human ophidian accidents. Freeze-dried venom milked from adult zebra snakes was dissolved in phosphate bufered saline (PBS) for use in this study. Haemorrhagic and necrotic activity of venom were studied in New Zealand albino rabbits. Oedema-forming activity was investigated in 10-day-old Cobb500 broiler chicks. Procoagulant and thrombolytic activity was investigated in adult Kalahari red goat blood in vitro. -

A Preliminary Herpetological Survey of the Vilanculos Coastal Wildlife Sanctuary on the San Sebastian Peninsula, Vilankulo, Mozambique
Herpetology Notes, volume 3: 181-193 (2010) (published online on 31 May 2010) A preliminary herpetological survey of the Vilanculos Coastal Wildlife Sanctuary on the San Sebastian Peninsula, Vilankulo, Mozambique Niels H.G. Jacobsen1*, Errol W. Pietersen2 & Darren W. Pietersen3 Abstract. This paper reports on and discusses the findings of a herpetofaunal survey of the San Sebastian Peninsula, Vilankulo, Mozambique. A total of 39 reptile and 20 amphibian species were recorded including new records for Mozambique, range extensions and taxa previously considered endemic to the Bazaruto Archipelago. Keywords. Herpetofauna, San Sebastian Peninsula, Vilankulo, Mozambique. Introduction These islands form a northward extension of the San Sebastian Peninsula. The herpetofauna of Mozambique is still relatively A survey of the herpetofauna of the San Sebastian poorly known, especially when compared to the rest of Peninsula was undertaken as part of a larger study of southern Africa. The most recent accounts are those of the vegetation and fauna to assess the conservation Broadley (1966a, 1983), Poynton & Broadley (1985a, importance of the area. b, 1987, 1988) and Channing 2001. In addition, it appears that some early records have been overlooked The Study Site in museum collections. Apart from these, most The San Sebastian Peninsula lies south-east of the recent records often emanate from scant, sporadic town of Vilankulo, forming the mainland extension of or opportunistic collecting (Downs & Wirminghaus the Bazaruto Archipelago which includes Margaruque, 1990). As a result there is a void in our knowledge, Benguera, Bazaruto and Santa Carolina islands (Fig. 1). which also complicates the interpretation of species’ The Vilanculos Coastal Wildlife Sanctuary (VCWS) distributions and even the taxonomic status of some lies along the peninsula between 22.0833 and 22.3500° species. -

Snakes of Durban
SNakes of durban Brown House Snake Herald Snake Non - venomous Boaedon capensis Crotaphopeltis hotamboeia Often found near human habitation where they Also referred to as the Red-lipped herald. hunt rodents, lizards and small birds. This nocturnal (active at night) snake feeds They are active at night and often collected mainlyly on frogs and is one of the more common for the pet trade. snakes found around human dwellings. SPOTTED BUSH Snake Eastern Natal Green Snake Southern Brown Egg eater Philothamnus semivariegatus Philothamnus natalensis natalensis Dasypeltis inornata Probably the most commonly found snake in This green snake is often confused with the This snake has heavily keeled body scales and urban areas. They are very good climbers, Green mamba. This diurnal species, (active during is nocturnal (active at night) . Although harmless, often seen hunting geckos and lizards the day) actively hunts frogs and geckos. they put up an impressive aggression display, in the rafters of homes. Max length 1.1 metres. with striking and open mouth gaping. Can reach This diurnal species (active during the day) over 1 metre in length and when they are that big is often confused with the Green mamba. they can eat chicken eggs. Habitat includes Max length 1.1 metres. grasslands, coastal forests and it frequents suburban gardens where they are known to enter aviaries in search of eggs. night adder Causus rhombeatus A common snake often found near ponds and dams because they feed exclusively on amphibians. They have a cytotoxic venom and bite symptoms will include pain and swelling. Max length 1 metre. -

RJHS 6(2).Cdr
Management of snakebite victims Ayinbuomwan et al. Management of snakebite victims using low dose antisnake venom in a tertiary hospital in Southern Nigeria: A 5-year Retrospective study *Ayinbuomwan A.S.1,2, Opadeyi A.O.1,2, and Isah A.O.1,2 Abstract Objective: Antisnake venom (ASV) is a specific antidote for the management of snake bite envenomations. This study profiled the treatment and outcome of adult snake bite victims managed using low dose antisnake venom. Methods: This was a 5-year retrospective study that involved all adult patients who presented in University of Benin Teaching Hospital, Benin City, Nigeria, with a history of snake bite. Information obtained were demographic characteristics, clinical features, and administered treatment per established. All patients with a diagnosis of snake bite envenomation were administered ASV. Results: Sixty patients were seen during the study period, 35(58.3%) males, 25(41.7%) females with a mean age was 34.7±13.3. The mean time from bite to presentation was 14.67±14.05 hours with range of 1- 48 hours. Twenty patients (33.3%) had snake bite envenomations, of these eleven (57.9%) were managed and discharged after administration of 30 to 40 mls of polyvalent ASV. The mean dose of PASV used was 3.9 ± 2.0 vials. The most encountered clinical indication for ASV administration was progressive painful swelling. No death was recorded throughout this period studied. Conclusion: Adoption of the low dose regimen in the management of snake bite envenomations may be as effective as the traditional high dose regimen. -

Zambia & Malawi
Zambia & Malawi - The Best of Africa Naturetrek Tour Report 2 - 9 October 2016 Red-billed Oxpeckers on Kudu in middle of breeding herd of Elephants Red-necked Spurfowl Looking at African Skimmers near Mwalasi Enjoying Sable Antelopes Report and images by Samuel Lenard Chihana Naturetrek Mingledown Barn Wolf's Lane Chawton Alton Hampshire GU34 3HJ UK T: +44 (0)1962 733051 E: [email protected] W: www.naturetrek.co.uk Tour Report Zambia & Malawi - The Best of Africa Tour participants: Samuel Lenard Chihana (Local Guide) with four Naturetrek Clients Please note that this tour report only covers the first part of the tour, in Malawi, that was led by Samuel Lenard Chihana. We do not have reports from the other Local Guides. Day 1 Sunday 2nd October In flight to Kamuzu International Airport. Day 2 Monday 3rd October Weather: overcast and cloudy. We met at Kamuzu International Airport and, having sorted immigration formalities, changed their money and loaded the vehicle, we started our drive to Mvuu around 2.35pm. Along a Forest Reserve at Linthipe I offered them a packed lunch and they had an opportunity to walk around and stretch their legs. During our lunch break we saw Southern Citril and Bronze Manikin, flying and perched. On our way from the airport and just before stopping we saw Pied Crows, Lilac-breasted Rollers and House Sparrows. We also saw White-necked Ravens as we passed Dedza. We arrived at around 7.45pm. I gave them a briefing during check in, mentioning all activities offered in the Camp, including Village Tours, Rhino tracking, Sanctuary Drives and Hides, Help Malawi and School Visiting, and also the opportunity to visit or participate in Bat or Carnivore Research, if interested. -

Snake and Lizards of Minnesota
SNAKES AND LIZARDS OF MINNESOTA TABLE OF CONTENTS Acknowledgments . 4 Introduction . 6 Key to Minnesota’s Snakes . 24 Common Gartersnake . 26 Common Watersnake . 28 DeKay’s Brownsnake . 30 Eastern Hog‑nosed Snake . 32 Gophersnake . 34 Lined Snake . 36 Massasauga . 38 Milksnake . 40 North American Racer . 42 Plains Gartersnake . 44 Plains Hog‑nosed Snake . 46 Red‑bellied Snake . 48 Ring‑necked Snake . 50 Smooth Greensnake . 52 Timber Rattlesnake . 54 Western Foxsnake . 56 Western Ratsnake . 58 Key to Minnesota’s Lizards . 61 Common Five‑lined Skink . .. 62 Prairie Skink . 64 Six‑lined Racerunner . 66 Glossary . 68 Appendix . 70 Help Minnesota’s Wildlife! . 71 Cover photos: Timber rattlesnakes photograph by Barb Perry . Common five‑lined skink photograph by Carol Hall . Left: Park naturalist holding gophersnake . Photograph by Deborah Rose . ACKNOWLEDGMENTS Text Rebecca Christoffel, PhD, Contractor Jaime Edwards, Department of Natural Resources (DNR) Nongame Wildlife Specialist Barb Perry, DNR Nongame Wildlife Technician Snakes and Lizards Design of Minnesota Creative Services Unit, DNR Operation Services Division Editing Carol Hall, DNR Minnesota Biological Survey (MBS), Herpetologist Liz Harper, DNR Ecological and Water Resources (EWR), Assistant Central Regional Manager Erica Hoagland, DNR EWR, Nongame Wildlife Specialist Tim Koppelman, DNR Fish and Wildlife, Assistant Area Wildlife Manager Jeff LeClere, DNR, MBS, Animal Survey Specialist John Moriarity, Senior Manager of Wildlife, Three Rivers Park District Pam Perry, DNR, EWR, Nongame Wildlife Lake Specialist (Retired) This booklet was funded through a State Wildlife Grant and the Nongame Wildlife Program, DNR Ecological and Water Resources Division . Thank you for your contributions! See inside back cover . ECOLOGICAL AND WATER RESOURCES INTRODUCTION is understandable in Minnesota, spend most of the active season .