Challenges and Facilitators for Intersectoral Health Policy in a Danish Municipality
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Co-Operation Between Municipalities and Pharmacies on Local Disease
- El-Souri Mira* Cooperation between municipalities and community - Andrés L** - Burghle A* - Faber NH** - Friese B* pharmacies on local prevention and health promotion - Husted GR* - Rossing C* – what are the opportunities? * Pharmakon, Danish College of Pharmacy Practice Milnersvej 42, 3400 Hillerød, Denmark ** The Danish Commitee for Health Education, Classensgade 71, 5. sal 2100 København Ø, Denmark Contact information: ”The cooperation has been an eye opener - we can use each other for the benefit of our citizens” Gitte Reventlov Husted [email protected] Background Methods Study settings There is a current lack of knowledge on how A user involvement approach was chosen for the Five municipalities and six pharmacies (figure 1). pharmacies can be involved in cooperation with development of the collaboration model. Jammerbugt Municipality One pair from each Danish region participated in Aabybro Pharmacy municipalities to participate in health promotion a 1 ½ day-start-up seminar followed by a three and disease prevention. It seems that there is Through workshops1 the parties were guided to: Gladsaxe Municipality months study period (November 2017 till January Søborg Pharmacy an unutilized potential for involving pharmacies - define the target group of vulnerable citizens 2018). in disease prevention and health promotion and in their local area Ikast Brande Municipality Ikast Pharmacy linking them more closely to the rest of the health - agree on choice of healthcare service to Each collaborating pair worked together to system for the benefit of the individual citizen – deliver in collaboration provide an agreed service to 20 citizens and to ensure patient safety. - draft a plan on how to effectively cooperate in (100 in total). -

Emergency Management Assessment for Esbjerg Municipality
Emergency management assessment for Esbjerg Municipality 4th SEMESTER MSc. Risk and Safety Management Master Thesis January 10th 2017 Title: Abstract Emergency management assessment for Esbjerg Municipality The purpose of this project is to assess the emergency management setup of the municipality and the fire Theme: department of Esbjerg, Denmark. Furthermore, Master Thesis analyze an emergency situation exercise with the municipal management team, incorporating assistance Project Period: with a simulation software. Fall Semester 2016 First of all, a preliminary understanding of the current Project Group: emergency management setup is carried out, including RISK4-3-E16 legislation standards, the organizational structure, and Participants: the current emergency plans. In addition, a Numa Toro hypothetical emergency scenario is created, combined Ole Bjørn Pedersen with the use of a simulation software, in order to assess the team’s performance. Moreover, a FRAM model is Supervisor: created to describe outcomes based on a variability in Anders Schmidt Kristensen socio-technical systems. Dewan Ashan In conclusion, improvement can be drawn out of the Page Numbers: 81 emergency management performance during the Date of Completion: exercise simulation, such as communication, response January 10th 2017 time during decision making, and solutions quality. As well as the incorporation of simulation software to aid in the training and practice exercises. I II Acronyms AAU Aalborg University DEMA Danish Emergency Management Agency DMI Danmarks Meterologiske -

Iodine, Inorganic and Soluble Salts
Iodine, inorganic and soluble salts Evaluation of health hazards and proposal of a health-based quality criterion for drinking water Environmental Project No. 1533, 2014 Title: Editing: Iodine, inorganic and soluble salts Elsa Nielsen, Krestine Greve, John Christian Larsen, Otto Meyer, Kirstine Krogholm, Max Hansen Division of Toxicology and Risk Assessment National Food Institute, Technical University of Denmark Published by: The Danish Environmental Protection Agency Strandgade 29 1401 Copenhagen K Denmark www.mst.dk/english Year: ISBN no. Authored 2013. 978-87-93026-87-2 Published 2014. Disclaimer: When the occasion arises, the Danish Environmental Protection Agency will publish reports and papers concerning research and development projects within the environmental sector, financed by study grants provided by the Danish Environmental Protection Agency. It should be noted that such publications do not necessarily reflect the position or opinion of the Danish Environmental Protection Agency. However, publication does indicate that, in the opinion of the Danish Environmental Protection Agency, the content represents an important contribution to the debate surrounding Danish environmental policy. Sources must be acknowledged. 2 Iodine, inorganic and soluble salts Content CONTENT 3 PREFACE 5 1 GENERAL DESCRIPTION 6 1.1 IDENTITY 6 1.2 PRODUCTION AND USE 6 1.3 ENVIRONMENTAL OCCURRENCE AND FATE 7 1.3.1 Air 7 1.3.2 Water 7 1.3.3 Soil 8 1.3.4 Foodstuffs 10 1.3.5 Bioaccumulation 11 1.4 HUMAN EXPOSURE 11 2 TOXICOKINETICS 15 2.1 ABSORPTION 15 -

Report Miavibehansen
Developing Rural Mobility A CASE STUDY OF ALSELV By Mia Lodberg Vibe-Hansen, 20191883 MSc4 Mobilities & Urban studies Group: Ma4-urb19 Submitted 26.05.2021 Developing Rural Mobility A CASE STUDY OF ALSLEV BY MIA LODBERG VIBE-HANSEN SUBMITTED 26.05.2021 _________________________________________________ Student: Mia Lodberg Vibe-Hansen, 20191883 _________________________________________________ Supervisor: Claus Lassen 1 I Abstract Today there is an imbalance between the cities and the rural areas in Denmark. Many of the municipalities placed in rural Denmark are struggling with an increasing opt-out of their cities, which affects many areas within the municipality. The challenges of shrinking cities in rural areas are often seen in a generalizing and overall perspective, making it difficult to see the potentials within the individual city. Approached by a cross disciplinary mobilities perspective that is included in the new mobilities paradigm (Urry 2000), this project aims to explore the city of Alslev in Varde Municipality, in relation to the challenges of shrinking cities in rural Denmark. To see, if by adding a mobilities perspective, could unfold the city in a new perspective, which could give rise to new potentials and extend the knowledge upon which urban planners explore a city, and hopefully bring something new to the discussion of developing the rural areas within the municipality. By analysing the rural mobilities of Alslev, it will be studied how Alslev performs as a ‘place’ to identify what are the strengths of Alslev, and what could have potential for improvement. With a focus on everyday life, the citizens of Alslev’s everyday activities are used as a focal point for the mobilities perspective. -

Kemisk Grundvandskortlægning
DANMARKS OG GRØNLANDS GEOLOGISKE UNDERSØGELSE RAPPORT 2020/11 Danish review on advances in assessing: N retention in the subsurface in relation to future targeted N-regulation of agriculture November 2019 Birgitte Hansen, Anders Vest Christiansen, Tommy Dalgaard, Flemming Jørgensen, Bo V. Iversen, Jakob Juul Larsen, Charlotte Kjærgaard, Brian H. Jacobsen, Esben Auken, Anker Lajer Højberg & Stefan Schaper Geological survey of Øster Voldgade 10 GEUS is a research and advisory Denmark and Greenland (GEUS) DK-1350 Copenhagen K institution in the Danish Ministry GEOLOGICAL SURVEY OF DENMARK AND GREENLAND Denmark of Climate, Energy and Utilities DANISH MINISTRY OF CLIMATE, ENERGY AND UTILITIES DANMARKS OG GRØNLANDS GEOLOGISKE UNDERSØGELSE RAPPORT 2020/11 Danish review on advances in assessing: N retention in the subsurface in relation to future targeted N-regulation of agriculture November 2019 Birgitte Hansen, Anders Vest Christiansen, Tommy Dalgaard, Flemming Jørgensen, Bo V. Iversen, Jakob Juul Larsen, Charlotte Kjærgaard, Brian H. Jacobsen, Esben Auken, Anker Lajer Højberg & Stefan Schaper GEOLOGICAL SURVEY OF DENMARK AND GREENLAND DANISH MINISTRY OF CLIMATE, ENERGY AND UTILITIES 2 G E U S DE NATIONALE GEOLOGISKE UNDERSØGELSER FOR DANMARK OG GRØNLAND KLIMA- OG ENERGIMINISTERIET 3 Affiliation of authors Birgitte Hansen: GEUS Anders Vest Christiansen: Department of Geosciences, AU Tommy Dalgaard: Department of Agroecology, AU Flemming Jørgensen: Central Denmark Region Bo V. Iversen: Department of Agroecology, AU Jakob Juul Larsen: Department of Engineering, AU Charlotte Kjærgaard: SEGES, Landbrug og Fødevare Brian H. Jacobsen: Department of Food and Resource Economics, KU Esben Auken: Department of Geosciences, AU Anker Lajer Højberg: GEUS Stefan Schaper: Department of Management, BSS, AU 4 G E U S Content 1. -
Download Langt CV Som
Curriculum Vitae Professor Jan Damsgaard Copenhagen Business School January 2020 Personal data Full name: Jan Damsgaard Place of birth: Born in Viborg, Denmark, 1966 Citizenship: Danish Marital status: Married to Cecilie Paus Damsgaard (M.A. in Communications) Children: Simon (born 2000), Christian (born 2003), and Marcus (born 2008) Hobbies: Running, biking and gadgets! Address At work At home Department of Digitalization Skovvej 22 Howitzvej 60, office 3.01e 2820 Gentofte DK 2000 Frederiksberg Denmark Mobile : +45 2479 4309 Phone : +45 22420082 URL : www.cbs.dk/en/staff/jddigi E-mail : [email protected] Email: [email protected] Academic degrees Ph.D. in Information Systems, Aalborg University, Denmark (1996) Master of Science in Computer Science (Danish: Cand. Scient. med hovedfag i datalogi og sidefag i psykologi), Aalborg University, Denmark (1993) Current memberships SME:Digital panel appointed by the Cabinet Minister of Business (2018 - ) Member of Ledernes Digitale Tænketank (2019 – ) www.lederne.dk The Danish Prime Minister´s Disruption Council (Statsministerens Disruptionråd) (2017 – ) National Digital Advisor appointed by the Danish Academy of Technical Sciences (Danish: ATV Digital Vismand) (2014 - ) Member of Danish Academy of Technical Sciences (2014 – ) www.atv.dk Member of VL Group 26 of The Danish Management Society for Top Executives (2012 – ) www.vl.dk Board of directors Member of the board - Auction Group A/S (2016 – ) www.autoproff.dk Member of the board – RelyOn Nutec (2019 – ) www.relyonnutec.com Member of the board - IoT DK A/S (2016 – ) www.iotdk.dk Positions Current position Full professor, Department of Digitalization, Copenhagen Business School. Since July 2006 – Previous positions Head of department, Department of Digitalization, Copenhagen Business School. -

Intersectoral Health Policy in Varde, Denmark Case Study Report
Process evaluation of the development and implementation of an intersectoral health policy in Varde municipality, Denmark Authors: Maja Larsen, PhD Okje Anna Koudenburg, B.Sc Gabriel Gulis, PhD University of Southern Denmark, Institute of Public Health, Unit for Health Promotion Research 1 © World Health Organization 2014 All rights reserved. Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO web site (www.who.int/about/licensing/copyright_form/en/index.html), or to the WHO Centre for Health Development, I.H.D. Centre Building, 9th Floor, 5-1, 1-chome, Wakinohama-Kaigandori, Chuo-ku, Kobe City, Hyogo Prefecture, 651-0073, Japan (fax: +81 78 230 3178; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. -

Annual Report 2016
ANNUAL REPORT 2016 THE DOCTORAL SCHOOL OF SOCIAL SCIENCES CONTENTS PREFACE 3 REPORT FROM THE DOCTORAL SCHOOL 4 STRATEGIC ACTION PLAN FOR THE DOCTORAL SCHOOL OF SOCIAL SCIENCES 2016-2021 6 COMPETENCES AND CAREER PROFILES OF PHD GRADUATES FROM THE HUMANITIES AND SOCIAL SCIENCES 9 STATUS AND TRENDS 11 LIST OF AWARDED DEGREES IN 2016 15 THE DOCTORAL PROGRAMME IN LIST OF PHD COURSES IN 2016 SOCIOLOGY AND SOCIAL WORK 20 24 PARTNERS THE DOCTORAL PROGRAMME IN 22 POLITICAL SCIENCE 26 DOCTORAL PROGRAMMES IN INNOVATION AND BUSINESS ECONOMICS 28 THE DOCTORAL PROGRAMME IN CULTURE AND GLOBAL STUDIES 30 THE DOCTORAL PROGRAMME IN LAW AND BUSINESS LAW 34 THE DOCTORAL PROGRAMME IN EDUCATION, LEARNING AND PHILOSOPHY 36 PREFACE It is our great pleasure to present the Annual report 2016 versity. It continues many of the strategic initiatives set for the Doctoral School of Social Sciences at Aalborg Uni- forth in the previous strategic action plan, but also details versity. The report describes the status, together with most several new initiatives. The detailed plan is presented in important activities at the Doctoral School in the period. the report. Furthermore, Professor Poul Houman Ander- In addition, the report lists the seven affiliated Doctoral sen has been appointed as new Director of the Doctoral Programs. School. He replaces Professor Ann-Dorte Christensen, who has been heading the school 2011-2016. 2016 marks a year of progress and change, both in terms of implementing new strategic directions and in terms of The annual report consists of two parts. The first part con- uniting the administrative services of the Faculty of Huma- cerns the Doctoral School’s general development and ac- nities and the Social Sciences. -
Topsoil Resilient Soil and Water Resources, Understanding the Water Beneath Your Feet Colophon
Midterm Catalogue Topsoil Resilient soil and water resources, understanding the water beneath your feet Colophon The Topsoil mid-term catalog is published by Region Midtjylland and compiled by the partners of the Topsoil project. Questions and suggestions Region Midtjylland (lead beneficiary) Contact person: Project manager Flemming Jørgensen Email: [email protected] You can download the publication at https://northsearegion.eu/topsoil Publisher Flemming Jørgensen (Project manager) Layout and design Formatting: Stefan David, https://www.stefandavid.be Pictures: Yves Adams, partners in the Topsoil project 2 Foreword Climate change affects the hydrological cycle and we now experience more heavy rains and increas- ing sea levels. The changes in climate also affect the groundwater aquifers – the water beneath our feet. The Topsoil project explores the possibilities of using the topsoil layers to solve current and fu- ture water challenges concerning water quantity and quality. It looks beneath the surface of the ground, predicts and finds solutions for climate related threats like flooding during wet periods and droughts during summer seasons. The overall objective of the project is the joint development of methods to describe and manage the uppermost 30 m of the subsurface, in order to improve the climate resilience and protect the environment of the North Sea Region. Across the North Sea in Northern Europe we share different challenges within ground water and climate change. In a 3½ year European project we have adressed five shared challenges via geological, geophysical and hydrological investigations, stakeholder involvement and changes in management. In 16 pilot areas we have developed and tested solutions for managing the uppermost 20-30 m of the subsurface. -
A Future As a General Medical Practitioner in Denmark Three General Medical Practitioners in Southern Denmark
A future as a general medical practitioner in Denmark Three general medical practitioners in Southern Denmark regionsyddanmark.dk Maj 2016 General medical practice recruitment Basic principles and facts Our recruitment team is available for dis- Contact details for the Basic principles of the health care Facts cussions and any questions you may have, recruitment team system in Denmark • Norm: 1,600 patients per GP and Gitte Kristensen will be your contact Project Manager Gitte Kristensen • All residents in Denmark have equal • Region of Southern Denmark person throughout the process. After 14 +45 7663 1439 access to publicly financed health care • 788 GPs months’ employment, Gitte will continue as [email protected] services, regardless of employment and • 383 GP practices/clinics your sparring partner and help you contact financial and social status • 90% of the population have at least general medical practices in view of finding Secretary Marianne Blom Petersen • Health is a public responsibility – most 1 contact with a GP within a year employment. +45 7663 1391 services are financed, planned and opera- • 7 contacts per citizen, 6.5 – daytime, [email protected] ted by the Regions 0.5 outside daytime • The financing of health care services Recruitment Consultant derives mainly from taxation Charlotte Godsk Hansen • The system is characterised by decen- [email protected] tralisation of responsibility to politically elected councils GP – main facts in short • Own private medical practice/clinic (solo practice, partnership practice, collabora- tive practice or sharing practices) • Monitored by the Region and the GPs in cooperation • Family doctor • Gatekeeper • No co-payment • Number and distribution of GPs according to a plan • Financing the GPs: 75% fee for service, 25% capitation payment • Average income for a Danish GP: Practice/clinic turnover approx. -
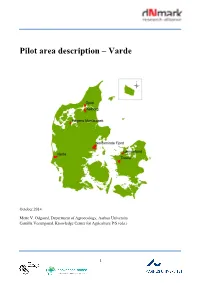
Pilot Area Description – Varde
Pilot area description – Varde October 2014 Mette V. Odgaard, Department of Agroecology, Aarhus University Camilla Vestergaard, Knowledge Center for Agriculture P/S (eds.) 1 Content 1. General pilot area description……….…………………………………………...……….…… 3 2. Varde – geographical location….…………………..……………………………..……………. 4 2.1. Land use…………………………………………………………………………. 5 2.2. Soil type………..………………………………………………………………… 8 2.3. Terrain……………………………………………………….…………………. 10 2.4. Hydrology…..…………….………………….………………………………… 12 3. References………………………………………………………………………...……………. 13 2 1. General pilot area description The alliance finds it important to develop and test solutions in cooperation with multiple operators from different areas of the country. One important focus area is the area surrounding the Limfjord. Here the alliance will work in e.g. Skive and Jammerbugt municipalities. Moreover, operators from Varde, Horsens, and Odsherred municipalities will be involved. So far, the alliance has established 7 pilot areas. These areas will function as test-case areas where scientists and operators can meet and discuss the implementation of different initiatives. Scientific results and experience from these areas can later be used in other localities with similar characteristics. It is therefore important that the pilot areas represent the variability of Denmark not only in relation to geographical location but also to land use, geology, etc. The delineation of the pilot areas is based on water catchment and therefore often relates to a given fjord or a watercourse system. Operators from other parts of the country will be involved ongoing. Thereby, the different research areas will develop the most optimal way. Map: Overview of the pilot areas. 3 2. Varde – geographical location The pilot area Varde covers an area of 6282 ha and belongs to Varde municipality in western Jutland. -

Thomas Larsen
Thomas Larsen Fra: Mikkel Sønderstrup Randløv <[email protected]> Sendt: 8. april 2019 19:06 Til: $Kystdirektoratet (kdi) Cc: Thomas Larsen; Nikolaj Michelsen; Jørn Bo Larsen Emne: Ansøgning om tilladelse til anlæg af et fiber optisk kabel under navnet Havhingsten på dansk søterritorium samt i den danske eksklusive økonomiske zone Vedhæftede filer: S2_HAVHINGSTEN_FINAL_ROUTE CORRIDOR_130319.zip Kategorier: Grøn Til Kystdirektoratet På vegne af North Sea Connect Denmark ApS indsendes hermed ansøgning om anlæg af et fiber optisk kabel under navnet Havhingsten på dansk søterritorium samt i den danske eksklusive økonomiske zone. Vedhæftet er dokumentet ”Ansøgning_Havhingsten_08.04.2019” der indeholder følgende: 1. Ansøgning om tilladelse til anlæg på søterritoriet (application form from the Danish Coastal Authority) 2. Project information and environmental screening, Denmark 3. Sea chart with the cable route 4. Power of attorney from the landowner 5. Risk assessment according to guidelines from the Danish Maritime Authority Vedhæftet er desuden shape-filer for den ansøgte rutekorridor. Vi står til rådighed hvis der er behov for supplerende oplysninger eller afklaringer. Med venlig hilsen Mikkel Randløv Biolog Projektchef Environmental Assessment and Industrial Environment D +45 51616379 M +45 51616379 [email protected] _________________________________ Rambøll Hannemanns Allé 53 DK-2300 København S https://dk.ramboll.com CVR NR. 35128417 1 Ansøgning om tilladelse til anlæg på søterritoriet Dette ansøgningsskema benyttes ved ansøgning om tilladelser til etablering, renovering og udvidelse af anlæg på søterritoriet. Husk at læse vejledningen på side 6, før skemaet udfyldes. Eventuelle spørgsmål til ansøgningsskema og vejledning rettes til Kystdirektoratet på tlf. 99 63 63 63 eller via e-mail [email protected].