Identifying Aging Villages with Primary Care Shortages: a Geographic Information System Approach 615
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Expert-Based Assessment Model for Evaluating Habitat Suitability of Pond-Breeding Amphibians
sustainability Article An Expert-Based Assessment Model for Evaluating Habitat Suitability of Pond-Breeding Amphibians Shin-Ruoh Juang 1, Szu-Hung Chen 2 and Chen-Fa Wu 1,* 1 Department of Horticulture, National Chung Hsing University, Taichung City 402, Taiwan; [email protected] 2 Department of Ecosystem Science & Management, Texas A&M University, College Station, TX 77843, USA; [email protected] * Correspondence: [email protected]; Tel./Fax: +886-4-2285-9125 Academic Editor: Iain Gordon Received: 8 November 2016; Accepted: 10 February 2017; Published: 16 February 2017 Abstract: Farm ponds are important habitats for amphibians, birds, and other wildlife. In Taiwan, artificial ponds were originally created on farmlands for irrigation purposes and the needs of the domestic water supply. Although pond creation is a typical farming practice, it also provides habitats for pond-breeding amphibians. Thus, it is essential to understand the current status of habitats and their vulnerability regarding urgent conservation needs for target species. Günther’s frog (Hylarana guentheri), a pond-breeding amphibian, has a high sensitivity towards surrounding environmental changes, and can be used as an indicator species to assess habitat suitability. The purpose of this study is to establish a systematic framework to assess the habitat suitability of pond-breeding amphibians by using Günther’s frog as a pilot-study species. First, we collected frog survey data from Chiayi, Taiwan, from winter 2013 to spring 2015, and investigated the present status of the environmental conditions around the ponds. Next, expert questionnaires and the fuzzy Delphi method were applied to establish the hierarchical evaluation criteria regarding the habitat suitability assessment. -
Cycling Taiwan – Great Rides in the Bicycle Kingdom
Great Rides in the Bicycle Kingdom Cycling Taiwan Peak-to-coast tours in Taiwan’s top scenic areas Island-wide bicycle excursions Routes for all types of cyclists Family-friendly cycling fun Tourism Bureau, M.O.T.C. Words from the Director-General Taiwan has vigorously promoted bicycle tourism in recent years. Its efforts include the creation of an extensive network of bicycle routes that has raised Taiwan’s profile on the international tourism map and earned the island a spot among the well-known travel magazine, Lonely Planet’s, best places to visit in 2012. With scenic beauty and tasty cuisine along the way, these routes are attracting growing ranks of cyclists from around the world. This guide introduces 26 bikeways in 12 national scenic areas in Taiwan, including 25 family-friendly routes and, in Alishan, one competition-level route. Cyclists can experience the fascinating geology of the Jinshan Hot Spring area on the North Coast along the Fengzhimen and Jinshan-Wanli bikeways, or follow a former rail line through the Old Caoling Tunnel along the Longmen-Yanliao and Old Caoling bikeways. Riders on the Yuetan and Xiangshan bikeways can enjoy the scenic beauty of Sun Moon Lake, while the natural and cultural charms of the Tri-Mountain area await along the Emei Lake Bike Path and Ershui Bikeway. This guide also introduces the Wushantou Hatta and Baihe bikeways in the Siraya National Scenic Area, the Aogu Wetlands and Beimen bikeways on the Southwest Coast, and the Round-the-Bay Bikeway at Dapeng Bay. Indigenous culture is among the attractions along the Anpo Tourist Cycle Path in Maolin and the Shimen-Changbin Bikeway, Sanxiantai Bike Route, and Taiyuan Valley Bikeway on the East Coast. -

Download Article
Advances in Social Science, Education and Humanities Research, volume 205 The 2nd International Conference on Culture, Education and Economic Development of Modern Society (ICCESE 2018) The Research on Docking Model of Rural Tourism across the Taiwan Straits Xicong Zheng Tourism Management Minnan Normal University Zhangzhou, China 363000 Abstract—In recent years, rural travel has become a new tourism promotion, and the most basic form of rural tourism form of tourism in the industry of China. It is a tourism product should have: developed by the combination of rural and agricultural production and the resource advantages of the countryside, so 1. Located in a rural area. that the rural industrial economy will show new vitality and 2. Village function: It consists of small businesses, open realize the sustainable development of rural tourism. This paper spaces, natural environments, monuments, traditional societies analyzes and compares the mode of rural tourism by exploring and customs. docking pattern on both sides of the Taiwan Straits, and puts forward some suggestions. 3. Village size: Buildings and the environment are small scales. Keywords—both sides of the Taiwan Straits; rural tourism; docking pattern 4. With traditional qualities, slow growth rate, and close relationship with local families. I. INTRODUCTION 5. The combination of rural environment, economy, history Rural tourism originated in France in 1855, and has a and location. history of more than 100 years. In the 1960s, rural tourism in The European Union and the World Organization for the modern sense began in Spain, and then it developed rapidly Economic Cooperation and Development (1994) defined rural in developed countries. -
![[カテゴリー]Location Type [スポット名]English Location Name [住所](https://docslib.b-cdn.net/cover/8080/location-type-english-location-name-1138080.webp)
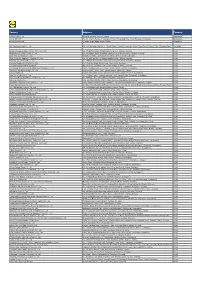
[カテゴリー]Location Type [スポット名]English Location Name [住所
※IS12TではSSID"ilove4G"はご利用いただけません [カテゴリー]Location_Type [スポット名]English_Location_Name [住所]Location_Address1 [市区町村]English_Location_City [州/省/県名]Location_State_Province_Name [SSID]SSID_Open_Auth Misc Hi-Life-Jingrong Kaohsiung Store No.107 Zhenxing Rd. Qianzhen Dist. Kaohsiung City 806 Taiwan (R.O.C.) Kaohsiung CHT Wi-Fi(HiNet) Misc Family Mart-Yongle Ligang Store No.4 & No.6 Yongle Rd. Ligang Township Pingtung County 905 Taiwan (R.O.C.) Pingtung CHT Wi-Fi(HiNet) Misc CHT Fonglin Service Center No.62 Sec. 2 Zhongzheng Rd. Fenglin Township Hualien County Hualien CHT Wi-Fi(HiNet) Misc FamilyMart -Haishan Tucheng Store No. 294 Sec. 1 Xuefu Rd. Tucheng City Taipei County 236 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Misc 7-Eleven No.204 Sec. 2 Zhongshan Rd. Jiaoxi Township Yilan County 262 Taiwan (R.O.C.) Yilan CHT Wi-Fi(HiNet) Misc 7-Eleven No.231 Changle Rd. Luzhou Dist. New Taipei City 247 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Restaurant McDonald's 1F. No.68 Mincyuan W. Rd. Jhongshan District Taipei CHT Wi-Fi(HiNet) Restaurant Cobe coffee & beauty 1FNo.68 Sec. 1 Sanmin Rd.Banqiao City Taipei County Taipei CHT Wi-Fi(HiNet) Misc Hi-Life - Taoliang store 1F. No.649 Jhongsing Rd. Longtan Township Taoyuan County Taoyuan CHT Wi-Fi(HiNet) Misc CHT Public Phone Booth (Intersection of Sinyi R. and Hsinsheng South R.) No.173 Sec. 1 Xinsheng N. Rd. Dajan Dist. Taipei CHT Wi-Fi(HiNet) Misc Hi-Life-Chenhe New Taipei Store 1F. No.64 Yanhe Rd. Anhe Vil. Tucheng Dist. New Taipei City 236 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Misc 7-Eleven No.7 Datong Rd. -
Factory Address Country
Factory Address Country Durable Plastic Ltd. Mulgaon, Kaligonj, Gazipur, Dhaka Bangladesh Lhotse (BD) Ltd. Plot No. 60&61, Sector -3, Karnaphuli Export Processing Zone, North Potenga, Chittagong Bangladesh Bengal Plastics Ltd. Yearpur, Zirabo Bazar, Savar, Dhaka Bangladesh ASF Sporting Goods Co., Ltd. Km 38.5, National Road No. 3, Thlork Village, Chonrok Commune, Korng Pisey District, Konrrg Pisey, Kampong Speu Cambodia Ningbo Zhongyuan Alljoy Fishing Tackle Co., Ltd. No. 416 Binhai Road, Hangzhou Bay New Zone, Ningbo, Zhejiang China Ningbo Energy Power Tools Co., Ltd. No. 50 Dongbei Road, Dongqiao Industrial Zone, Haishu District, Ningbo, Zhejiang China Junhe Pumps Holding Co., Ltd. Wanzhong Villiage, Jishigang Town, Haishu District, Ningbo, Zhejiang China Skybest Electric Appliance (Suzhou) Co., Ltd. No. 18 Hua Hong Street, Suzhou Industrial Park, Suzhou, Jiangsu China Zhejiang Safun Industrial Co., Ltd. No. 7 Mingyuannan Road, Economic Development Zone, Yongkang, Zhejiang China Zhejiang Dingxin Arts&Crafts Co., Ltd. No. 21 Linxian Road, Baishuiyang Town, Linhai, Zhejiang China Zhejiang Natural Outdoor Goods Inc. Xiacao Village, Pingqiao Town, Tiantai County, Taizhou, Zhejiang China Guangdong Xinbao Electrical Appliances Holdings Co., Ltd. South Zhenghe Road, Leliu Town, Shunde District, Foshan, Guangdong China Yangzhou Juli Sports Articles Co., Ltd. Fudong Village, Xiaoji Town, Jiangdu District, Yangzhou, Jiangsu China Eyarn Lighting Ltd. Yaying Gang, Shixi Village, Shishan Town, Nanhai District, Foshan, Guangdong China Lipan Gift & Lighting Co., Ltd. No. 2 Guliao Road 3, Science Industrial Zone, Tangxia Town, Dongguan, Guangdong China Zhan Jiang Kang Nian Rubber Product Co., Ltd. No. 85 Middle Shen Chuan Road, Zhanjiang, Guangdong China Ansen Electronics Co. Ning Tau Administrative District, Qiao Tau Zhen, Dongguan, Guangdong China Changshu Tongrun Auto Accessory Co., Ltd. -

Relationships Between Floods and Social Fragmentation: a Case Study of Chiayi, Taiwan
Relationships between floods and social fragmentation: A case study of Chiayi, Taiwan • Yung-Jaan Lee • Chung-Hua Institution for Economic Research, Taiwan • Li-Pei Peng* • Ting-Jay Lee • National Taiwan University, Taiwan *Corresponding author Abstract Resumen Lee, Y.-J. Peng, L.-P., & Lee, T.-J. (March-April, 2017). Lee, Y.-J. Peng, L.-P., & Lee, T.-J. (marzo-abril, 2017). Las Relationships between floods and social fragmentation: A relaciones entre las inundaciones y la fragmentación social: un case study of Chiayi, Taiwan. Water Technology and Sciences estudio de caso de Chiayi, Taiwán. Tecnología y Ciencias del (in Spanish), 8(2), 5-18. Agua, 8(2), 5-18. The social vulnerability approach has been recognized El enfoque de la vulnerabilidad social ha sido reconocido como una de las as one of the most important tools for exploring contexts herramientas más importantes para explorar contextos y estrategias and coping strategies in relation to contemporary disasters. de afrontamiento en relación con los desastres contemporáneos. Sin However, social vulnerability is such a multi-faceted and embargo, la vulnerabilidad social es un constructo tan multifacético complex construct that scholars from different fields have not y complejo que estudiosos de diversas disciplinas no han llegado a un consenso sobre la mejor manera de medirlo y continúa el debate reached consensus on how best to measure it, and discussions 5 on this issue continue. Some scholars consider that this sobre dicha cuestión. Algunos estudiosos consideran que este enfoque puede manifestar el papel de la intervención humana. Sin approach can manifest the role of human agency. However, embargo, dada la falta de observaciones históricas, interpretar las given a lack of historical observations, interpreting the causes causas de los desastres a través de perspectivas basadas en eventos of disasters through event-based perspectives cannot easily no puede reflejar el mecanismo institucional detrás de tales eventos. -

Agriculture Landscape Planning Based on Biotop Area Factor in Yunlin, Taiwan
AGRICULTURE LANDSCAPE PLANNING BASED ON BIOTOP AREA FACTOR IN YUNLIN, TAIWAN Su-Hsin Lee1 and Jing-Shoung Hou2 1Professor, Department of Geography, National Taiwan Normal University NO.162, Heping East Rd., Section1, Taipei, Taiwan; Tel: +886-2-77341665 Email: [email protected] 2Professor, Department of Landscape Architecture at Tung-Hai University NO.20-5, Lane 128, Sec. 3 Chung-Gone Rd., Taichung 407, Taiwan; Tel: +886-4-24635298 Email: [email protected] KEY WORDS: landscape planning, agriculture, BAF ABSTRACT: Agriculture has been the primary industry in Yunlin area for hundreds years. It contributes to industrial and living landscape which continuously represents vivid cultural landscape of the area. The strategies of landscape planning in Yunlin area not only emphasis on improving landscape and environment, but also focus on sustaining agricultural culture through landscape planning. In addition, ecological consideration and adapt-for-environment land use guidelines should be applied for local environmental development in order to meet the goal of sustainable environment planning. In this case, Yunlin area’s local industries and economy can continuously develop in the process of landscape improvement considering social, economic, and ecological dimensions. The strategies demonstrate the concept of green infrastructure (G.I.). Therefore, this study uses biotope area factor (BAF) to analyse environmental resource of Yunlin area in order to contribute to agricultural landscape planning. The results show: 1)Yunlin area can be categorised into different sub-area of land use according to BAF. The categories include agriculture land, forest land, transportation land, water conservancy land, building land, public infrastructure land, recreation and leisure land, mining land, and the land for other use. -

Mainland China's Policy Towards Reunification with Taiwan 1979
ONE COUNTRY TWO SYSTEMS MAINLAND CHINA'S POLICY TOWARDS REUNIFICATION WITH TAIWAN 1979 - CHING-YUN YANG THESIS SUBMITTED FOR THE PH.D. LONDON SCHOOL OF ECONOMICS AND POLITICAL SCIENCE UNIVERSITY OF LONDON 1992 UMI Number: U062759 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. Dissertation Publishing UMI U062759 Published by ProQuest LLC 2014. Copyright in the Dissertation held by the Author. Microform Edition © ProQuest LLC. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 ( M G S g S R 7 0 1 ^ ABSTRACT This research examines mainland China's reunification policy towards Taiwan with a particular focus on the years of 1979-1987. Following the establishment of Sino-U.S. diplomatic relations in January 1979,Communist leaders in Beijing carried out a series of intensive campaigns to woo the Nationalists in Taiwan to accept peace talks and to re-unify Taiwan and mainland China under the formula of "One Country Two Systems". The formula implies that, after unification, two different systems will remain - Socialism on the mainland and Capitalism in Taiwan for at least 50 years. Although Beijing's reunification policy has been further developed and persistently propagated, its efforts, so far, have met with little success. -

Evaluation of the Preservation Value and Location of Farm Ponds in Yunlin County, Taiwan
Int. J. Environ. Res. Public Health 2014, 11, 548-572; doi:10.3390/ijerph110100548 OPEN ACCESS International Journal of Environmental Research and Public Health ISSN 1660-4601 www.mdpi.com/journal/ijerph Article Evaluation of the Preservation Value and Location of Farm Ponds in Yunlin County, Taiwan Wen-Wen Chou 1, Soen-Han Lee 1 and Chen-Fa Wu 2,* 1 Department of Architecture, National Cheng Kung University, Tainan City 701, Taiwan; E-Mails: [email protected] (W.-W.C.); [email protected] (S.-H.L.) 2 Department of Horticulture, National Chung Hsing University, Taichung City 402, Taiwan * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel./Fax: +886-422-859-125. Received: 7 October 2013; in revised form: 3 December 2013 / Accepted: 13 December 2013 / Published: 31 December 2013 Abstract: Farm ponds in Yunlin County first appeared in 1,622 and have played roles in habitation, production, the ecology, culture, and disaster reduction. Farm ponds largely disappeared with the development of urban areas and the industrial sector; thus, effective preservation of the remaining ponds is critical. The criteria to evaluate the preservation value of farm ponds is established by expert questionnaires which follow the Fuzzy Delphi Method (FDM) and Fuzzy Analytic Hierarchy Process (FAHP), and GIS, which are integrated into a spatial analysis of the remaining 481 farm ponds in Yunlin County. The results show that 28 ponds should be preserved to continue the cultural interaction between farm ponds and settlements; 36 ponds should preserved to connect coasts and streams, which are important habitats for birds; 30 ponds should be preserved to increase storage capacity, recharge groundwater, and reduce land subsidence; four ponds should be preserved as Feng-Shui ponds in front of temples in settlements or as recreation areas for local citizens; and four farms should be preserved (high priority) in agricultural production areas to support irrigation. -

Eradication and Control Strategies for Red Imported Fire Ants (Solenopsis Invicta) in Taiwan
sustainability Article Eradication and Control Strategies for Red Imported Fire Ants (Solenopsis invicta) in Taiwan Helen K. Liu 1,*, Chung-Chi Lin 2,3, Li-Hsin Huang 4, Sin-An Huang 3 and Rong-Nan Huang 3,5,* 1 Department of Political Science, National Taiwan University, Taipei 10617, Taiwan 2 Department of Biology, National Changhua University of Education, Changhua County 50007, Taiwan; [email protected] 3 National Red Imported Fire Ant Control Center, Council of Agriculture, Executive Yuan, R.O.C. (Taiwan), Taipei 10617, Taiwan; [email protected] 4 Department of Pesticide Application, Taiwan Agricultural Chemicals and Toxic Substances Research Institute, Council of Agriculture, Executive Yuan, Taichung 41358, Taiwan; [email protected] 5 Department of Entomology, National Taiwan University, Taipei 10617, Taiwan * Correspondence: [email protected] (H.K.L.); [email protected] (R.-N.H.) Received: 11 April 2020; Accepted: 8 May 2020; Published: 12 May 2020 Abstract: Invasive alien species are one of the major threats to biological diversity, public safety, agriculture, and economics. In recent years, a new wave of the red imported fire ant (RIFA) has been detected in new regions, including Kobe (Japan), Daegu (South Korea), Kaohsiung (Taiwan), and other locations in southeast Asia. Due to the increasing number of invasions, practitioners and scientists are seeking effective strategies to respond to RIFA invasions in Pacific regions, especially in countries that have had no presence of RIFA. This study aims to identify the strategies adopted to eradicate RIFA in Taiwan and to elucidate some of the assumptions about RIFA prevention and treatment in infested areas with diverse land patterns. -

Non-Anopheline Mosquitoes of Taiwan: Annotated Catalog and Bibliography1
Pacific Insects 4 (3) : 615-649 October 10, 1962 NON-ANOPHELINE MOSQUITOES OF TAIWAN: ANNOTATED CATALOG AND BIBLIOGRAPHY1 By J. C. Lien TAIWAN PROVINCIAL MALARIA RESEARCH INSTITUTE2 INTRODUCTION The studies of the mosquitoes of Taiwan were initiated as early as 1901 or even earlier by several pioneer workers, i. e. K. Kinoshita, J. Hatori, F. V. Theobald, J. Tsuzuki and so on, and have subsequently been carried out by them and many other workers. Most of the workers laid much more emphasis on anopheline than on non-anopheline mosquitoes, because the former had direct bearing on the transmission of the most dreaded disease, malaria, in Taiwan. Owing to their efforts, the taxonomic problems of the Anopheles mos quitoes of Taiwan are now well settled, and their local distribution and some aspects of their habits well understood. However, there still remains much work to be done on the non-anopheline mosquitoes of Taiwan. Nowadays, malaria is being so successfully brought down to near-eradication in Taiwan that public health workers as well as the general pub lic are starting to give their attention to the control of other mosquito-borne diseases such as filariasis and Japanese B encephalitis, and the elimination of mosquito nuisance. Ac cordingly extensive studies of the non-anopheline mosquitoes of Taiwan now become very necessary and important. Morishita and Okada (1955) published a reference catalogue of the local non-anophe line mosquitoes. However the catalog compiled by them in 1955 was based on informa tion obtained before 1945. They listed 34 species, but now it becomes clear that 4 of them are respectively synonyms of 4 species among the remaining 30. -

The Image of Wu Feng in Taiwan School Readers
University of Massachusetts Amherst ScholarWorks@UMass Amherst Masters Theses 1911 - February 2014 2008 The orM al and Racial Socialization of Children: The mI age of Wu Feng in Taiwan School Readers Claire R. Maccabee University of Massachusetts Amherst Follow this and additional works at: https://scholarworks.umass.edu/theses Part of the Chinese Studies Commons Maccabee, Claire R., "The orM al and Racial Socialization of Children: The mI age of Wu Feng in Taiwan School Readers" (2008). Masters Theses 1911 - February 2014. 171. Retrieved from https://scholarworks.umass.edu/theses/171 This thesis is brought to you for free and open access by ScholarWorks@UMass Amherst. It has been accepted for inclusion in Masters Theses 1911 - February 2014 by an authorized administrator of ScholarWorks@UMass Amherst. For more information, please contact [email protected]. THE MORAL AND RACIAL SOCIALIZATION OF CHILDREN: THE IMAGE OF WU FENG IN TAIWAN SCHOOL READERS A Thesis Presented by CLAIRE R. MACCABEE Submitted to the Graduate School of University of Massachusetts Amherst in partial fulfillment for the requirements of the degree of MASTER OF ARTS September 2008 Chinese THE MORAL AND RACIAL SOCIALIZATION OF CHILDREN: THE IMAGE OF WU FENG IN TAIWAN SCHOOL READERS A Thesis Presented by CLAIRE R. MACCABEE Approved as to style and content by: ____________________________________ Alvin P. Cohen, Chair ____________________________________ Donald E. Gjertson, Member ____________________________________ Shaodan Luo, Member ________________________________________ Donald E. Gjertson, Director Asian Languages and Literatures _________________________________________ Julie Candler Hayes, Chair Department of Languages, Literatures, and Cultures DEDICATION First and foremost, to Professor Cohen, a phenomenal teacher, mentor, and friend.