Examination of the Newborn
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Non-Syndromic Occurrence of True Generalized Microdontia with Mandibular Mesiodens - a Rare Case Seema D Bargale* and Shital DP Kiran
Bargale and Kiran Head & Face Medicine 2011, 7:19 http://www.head-face-med.com/content/7/1/19 HEAD & FACE MEDICINE CASEREPORT Open Access Non-syndromic occurrence of true generalized microdontia with mandibular mesiodens - a rare case Seema D Bargale* and Shital DP Kiran Abstract Abnormalities in size of teeth and number of teeth are occasionally recorded in clinical cases. True generalized microdontia is rare case in which all the teeth are smaller than normal. Mesiodens is commonly located in maxilary central incisor region and uncommon in the mandible. In the present case a 12 year-old boy was healthy; normal in appearance and the medical history was noncontributory. The patient was examined and found to have permanent teeth that were smaller than those of the average adult teeth. The true generalized microdontia was accompanied by mandibular mesiodens. This is a unique case report of non-syndromic association of mandibular hyperdontia with true generalized microdontia. Keywords: Generalised microdontia, Hyperdontia, Permanent dentition, Mandibular supernumerary tooth Introduction [Ullrich-Turner syndrome], Chromosome 13[trisomy 13], Microdontia is a rare phenomenon. The term microdontia Rothmund-Thomson syndrome, Hallermann-Streiff, Oro- (microdentism, microdontism) is defined as the condition faciodigital syndrome (type 3), Oculo-mandibulo-facial of having abnormally small teeth [1]. According to Boyle, syndrome, Tricho-Rhino-Phalangeal, type1 Branchio- “in general microdontia, the teeth are small, the crowns oculo-facial syndrome. short, and normal contact areas between the teeth are fre- Supernumerary teeth are defined as any supplementary quently missing” [2] Shafer, Hine, and Levy [3] divided tooth or tooth substance in addition to usual configuration microdontia into three types: (1) Microdontia involving of twenty deciduous and thirty two permanent teeth [7]. -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Dental Anomalies: Foundational Articles and Consensus Recommendations, 2021
Dental Anomalies: Foundational Articles and Consensus Recommendations, 2021 Adekoya-Sofowora CA. Natal and neonatal teeth: a review. Niger Postgrad Med J 2008;15:38-41 Al-Ani AH, Antoun JS, Thomson WM, Merriman TR, Farella M. Hypodontia: An Update on Its Etiology, Classification, and Clinical Management. Biomed Res Int. 2017:9378325. doi.org/10.1155/2017/9378325. Anthonappa RP, King NM, Rabie AB. Aetiology of supernumerary teeth: A literature review. Eur Arch Paediatr Dent. 2013;14:279-88. Dashash, M. Yeung CA, Jamous I, Blinkhorn A. Interventions for the restorative care of amelogenesis imperfecta in children and adolescents. Cochrane Database Syst Rev 2013;6:CD007157. Gallacher A, Ali R, Bhakta S. Dens invaginatus: diagnosis and management strategies. Br Dent J 2016;221:383-7. Gill DS, Barker CS. The multidisciplinary management of hypodontia: a team approach. Br Dent J 2015;218:143-9. Khalaf K, Miskelly J, Voge E, Macfarlane TV. Prevalence of hypodontia and associated factors: a systematic review and meta-analysis. J Orthod. 2014; 41:299-316. Lammi L. Arte S, Somer M, Javinen H, et al. Mutations in AXIN2 cause familial tooth agenesis and predispose to colorectal cancer. Am. J. Hum. Genet. 2004, 74:1043–1050. Marvin ML, Mazzoni S, Herron CM, Edwards S, et al. AXIN2-associated autosomal dominant ectodermal dysplasia and neoplastic syndrome. Am J Med Genet A. 2011,155 898–902. Seow WK. Developmental defects of enamel and dentine: Challenges for basic science research and clinical management. Aust Dent J 2014;59:143-54. Shields ED, Bixler D, El-Kafrawy AM. A proposed classification for heritable human dentine defects with a description of a new entity. -

Teliangectaticum Granuloma Associated to a Natal Tooth Granuloma Telangiectásico Asociado a Diente Natal
www.medigraphic.org.mx Revista Odontológica Mexicana Facultad de Odontología Vol. 20, No. 1 January-March 2016 pp 29-32 CASE REPORT Teliangectaticum granuloma associated to a natal tooth Granuloma telangiectásico asociado a diente natal Katherine Vásquez Sanjuán,* Ary López Álvarez,§ Jonathan Harris RicardoII ABSTRACT RESUMEN Oral teliangectaticum granuloma, also known as pyogenic granuloma Granuloma telangiectásico bucal, también conocido como granulo- is a proliferation of exuberant granulation tissue caused by chronic ma piógeno, es una proliferación de tejido de granulación exuberan- inflammation or local irritation. It is a rare lesion in newborn; it te, a una infl amación crónica o una irritación local, poco frecuente appears as an isolated tumor lesion, mostly located in the anterior del recién nacido, que se presenta como una lesión tumoral única, zone of the alveolar crest. This lesion bleeds spontaneously and localizada con mayor frecuencia en la zona anterior de la cresta shows predilection for the female gender. Its etiology is related to alveolar, de sangrado espontáneo, tiene predilección por el género trauma factors, local irritation and hormonal changes. Due to its size femenino, la etiología se relaciona con factores traumáticos, irrita- it can affect the newborn’s feeding. Surgical removal is the choice ción local y cambios hormonales, por el tamaño puede afectar la treatment for this type of lesions. The present study presents the alimentación del neonato, la remoción quirúrgica es el tratamiento case of a newborn with diagnosis of telangiectaticum granuloma de elección. Se presenta caso clínico de recién nacido con diagnós- in the mandibular ridge associated to a natal tooth. -

Subset of Alphabetical Index to Diseases and Nature of Injury for Use with Perinatal Conditions (P00-P96)
Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) SUBSET OF ALPHABETICAL INDEX TO DISEASES AND NATURE OF INJURY FOR USE WITH PERINATAL CONDITIONS (P00-P96) Conditions arising in the perinatal period Conditions arising—continued - abnormal, abnormality—continued Note - Conditions arising in the perinatal - - fetus, fetal period, even though death or morbidity - - - causing disproportion occurs later, should, as far as possible, be - - - - affecting fetus or newborn P03.1 coded to chapter XVI, which takes - - forces of labor precedence over chapters containing codes - - - affecting fetus or newborn P03.6 for diseases by their anatomical site. - - labor NEC - - - affecting fetus or newborn P03.6 These exclude: - - membranes (fetal) Congenital malformations, deformations - - - affecting fetus or newborn P02.9 and chromosomal abnormalities - - - specified type NEC, affecting fetus or (Q00-Q99) newborn P02.8 Endocrine, nutritional and metabolic - - organs or tissues of maternal pelvis diseases (E00-E99) - - - in pregnancy or childbirth Injury, poisoning and certain other - - - - affecting fetus or newborn P03.8 consequences of external causes (S00-T99) - - - - causing obstructed labor Neoplasms (C00-D48) - - - - - affecting fetus or newborn P03.1 Tetanus neonatorum (A33) - - parturition - - - affecting fetus or newborn P03.9 - ablatio, ablation - - presentation (fetus) (see also Presentation, - - placentae (see also Abruptio placentae) fetal, abnormal) - - - affecting fetus or newborn -

Mortality Perinatal Subset, 2013
ICD-10 Mortality Perinatal Subset (2013) Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) Conditions arising in the perinatal period Note - Conditions arising in the perinatal period, even though death or morbidity occurs later, should, as far as possible, be coded to chapter XVI, which takes precedence over chapters containing codes for diseases by their anatomical site. These exclude: Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) Endocrine, nutritional and metabolic diseases (E00-E99) Injury, poisoning and certain other consequences of external causes (S00-T99) Neoplasms (C00-D48) Tetanus neonatorum (A33 2a) A -ablatio, ablation - - placentae (see alsoAbruptio placentae) - - - affecting fetus or newborn P02.1 2a -abnormal, abnormality, abnormalities - see also Anomaly - - alphafetoprotein - - - maternal, affecting fetus or newborn P00.8 - - amnion, amniotic fluid - - - affecting fetus or newborn P02.9 - - anticoagulation - - - newborn (transient) P61.6 - - cervix NEC, maternal (acquired) (congenital), in pregnancy or childbirth - - - causing obstructed labor - - - - affecting fetus or newborn P03.1 - - chorion - - - affecting fetus or newborn P02.9 - - coagulation - - - newborn, transient P61.6 - - fetus, fetal 1 ICD-10 Mortality Perinatal Subset (2013) - - - causing disproportion - - - - affecting fetus or newborn P03.1 - - forces of labor - - - affecting fetus or newborn P03.6 - - labor NEC - - - affecting fetus or newborn P03.6 - - membranes -

Common Pediatric Dental Problems
PEDIATRIC SURGERY FOR THE PRZMARY CARE PEDIATRICIAN, PART II 0031-3955/98 $8,00 + .OO COMMON PEDIATRIC DENTAL PROBLEMS Paul R. Creighton, DDS Pediatric dentistry is one of the eight specialties recognized by the American Dental Association. In the early 1900s, children were treated as ”little adults” and the focus of routine dentistry was to treat the effects of dental decay, such as pulpitis, and resultant pain from this condition. Initially, dental decay resulted in extraction and restorative treatment with emphasis on space maintenance and arch integrity. Since the early 1900s, tremendous improvements have taken place in restorative and preventative techniques. Today, pediatric dentistry is prevention oriented. The cornerstone of prevention-based pediatric dentistry is early referral to the dentist and routine follow-up visits. For many years, the American Academy of Pediatrics has recommended that children make their first dental visit after their third birthday. The Academy of Pediatric Dentistry, on the other hand, has recommended that children be seen by the age of 1 year. The goal of a pediatric dental practice is to emphasize the importance of oral health to the child and the child’s parents. Behavior management is still very much the backbone of the specialty. A primary goal of the treatment-oriented pediatric dental profession is behavior management. A prevention-oriented pediatric dental profession concentrates on educating the parents of very young children on the dental milestones seen in the pediatric population, proper diet, and other issues that prevent dental disease. Given the etiology, pathogenesis, and the treatment of dental diseases, prevention is the only true cure, although realistically, restorative treatment will always be a significant component to the specialty. -

Case Report Delayed Tooth Eruption in Congenital Hypertrkhosis Lanuginosa
Case Report Delayed tooth eruption in congenital hypertrkhosis lanuginosa Deborah L. Franklin, PhD, MDent Sci, BDS, FDSRCS (Eng), MRCD (C) Graham J. Roberts, MDS, PhD, FDSRCS (Eng), BDS, MPhil ypertrichosis in childhood is found in a vari- Dental anomalies such as neonatal teeth, hypodontia, ety of conditions and may be localized or the presence of supernumerary teeth, and "defects" in generalized.' Localized hypertrichosis may be the enamel have been reported in association with hy- H 3 5 7 related to trauma, nevi, or spina bifida occulta. Gen- pertrichosis lanuginosa. ' ' The present case illustrates eralized hypertrichosis can occur with a variety of delayed eruption of primary and permanent teeth re- metabolic, chromosomal, and congenital disorders; sulting in unusual root morphology of primary molar these include Gorlin syndrome, Cornelia de Lange syn- teeth, and also enamel hypoplasia. drome, Leprechaunism, the porphyrias and muco- polysaccharidoses, trisomy 18, gingival hyperplasia Case report with hypertrichosis, and the congenital hypertrichoses. A male child was born of unrelated parents follow- Pre- or postnatal drug exposure with drugs such as glu- ing a normal pregnancy and delivery. He was the first cocorticoids, cyclosporin, and maternal alcohol abuse born and has an unaffected younger brother. The in pregnancy may also result in hypertrichosis. In the mother had taken no medication or vitamin/mineral congenital hypertrichoses, excessive hair growth is the supplements during the pregnancy. The child was cov- primary disorder. The terminology of these disorders ered in dense blonde lanugo hair at birth which was has been confused in the past but they have been de- particularly dense around the base of the spine and scribed as congenital hypertrichosis universalis, external auditory canals. -
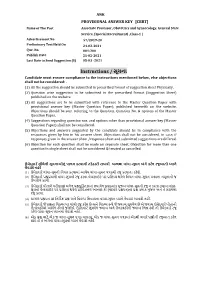
Instructions / સૂચના Candidate Must Ensure Compliance to the Instructions Mentioned Below, Else Objections Shall Not Be Considered:
ANK PROVISIONAL ANSWER KEY [CBRT] Name of The Post Associate Professor, Obstetrics and Gynaecology, General State Service, (Special Recruitment) ,Class-1 | Advertisement No 57/2019-20 Preliminary Test Held On 24-02-2021 Que. No. 001-200 Publish Date 25-02-2021 Last Date to Send Suggestion (S) 05-03 -2021 Instructions / સૂચના Candidate must ensure compliance to the instructions mentioned below, else objections shall not be considered: - (1) All the suggestion should be submitted in prescribed format of suggestion sheet Physically. (2) Question wise suggestion to be submitted in the prescribed formatr (Suggestion rSheet) published on the website.r r (3) All suggestions are to be submitted with reference to the Maste Question Pape withr provisional answe key (Maste Question Paper), published herewith on the website. Objections should be sent referring to the Question, rQuestion No. & options ofr the Maste Question Paper. (4) Suggestions regarding question nos. and options othe than provisional answe key (Master Question Paper) shall not be considered. r (5) Objections and answers suggestedr by the candidate should be in compliance with the responses givenr by him in his answe sheet. Objections shall not be considered, r in case, if responses given in the answe sheet /response sheet and submitted suggestions are differed. (6) Objection fo each question shall be made on separate sheet. Objection fo more than one question in single sheet shall not be considered & treated as cancelled. ઉમેદવાર ે નીચેની સૂચનાઓનું પાલન કરવાની તકેદારી રાખવી, અયથા વાંધા-સૂચન અંગે કર ેલ રજૂઆતો યાને લેવાશે નહીં (1) ઉમેદવારે વાંધા-સૂચનો િનયત કરવામાં આવેલ વાંધા-સૂચન પકથી રજૂ કરવાના રહેશે. -

Parturitional Brain Injury Definition of Parturitional Injury
Parturitional Brain Injury Definition of parturitional injury Thierry A.G.M. Huisman, MD • Any condition that affects the fetus adversely Director Pediatric Radiology and Pediatric Neuroradiology Johns Hopkins Hospital during labor and delivery • May be caused by: – Hypoxia and infection (birth injury) – Mechanical forces (birth trauma) Definition of parturitional injury Introduction • Life starts with a mechanical trauma – Squeezed together by a muscular wrapping • Any condition that affects the fetus adversely – Pushed through a narrow, bony canal with multiple bumps during labor and delivery – Getting your neck extended, rotated and pulled – Life line (umbilical cord) may be compressed – Possibly additional “medieval” instrumentation • May be caused by: – All of this for many minutes or even hours – Hypoxia and infection (birth injury) – Mechanical forces (birth trauma) Introduction Introduction • Life starts with a mechanical trauma • Life starts with a “stress” trauma – Or even worse, within minutes you are squeezed – And than suddenly lots of light, noise and many and “ejected” crying/emotional people around you,…. 1 Subjects who try to relive the „Scientific approach” “I am stuck feeling” Tortuguero expedition. www.philsheldon.wordpress.com Guettler FV, et al. Magnetic resonance imaging of the active second stage of labour: Proof of principle Eur Radiol 2012;22:2020-2026 Epidemiology Epidemiology • Significant variability across the world • Dramatically decreased in last decades • Birth trauma in 3% of all live births • Accounts for less than 2% of neonatal deaths • Even when the injuries are benign, birth trauma may result in significant anxiety for a family Disability adjusted life year (DALY): Measure of overall disease burden expressed as number of years lost due to ill-health, disability or early death Reichard R. -

Perinatal Journal
ISSN 1305–3124 PERINATAL PERINATAL JOURNAL JOURNAL PERINATAL Volume 24 | Issue 2 | August 2016 JOURNAL A L J O www.perinataljournal.com A T U N R I N R A E L P Contents Volume 24 | Issue 2 | August 2016 P L E R A I N N R A U T A L J O Original Article The cesarean rates and indications between 2010 and 2014 in the Obstetrics 61 Department of Dr. Zekai Tahir Burak Maternal Health Training and Research Hospital Gökçe Naz Küçükbafl, Özlem Moralo¤lu, fiule Özel, Salim Erkaya, Yasemin Taflc›, Rahime Bedir F›nd›k Comparison of first trimester uterine artery Doppler parameters in hyperemesis 66 gravidarum with normal pregnancy ‹smail B›y›k, Gökhan Ocako¤lu, Emin Üstünyurt, Fatih Y›lmaz, Fatih Keskin An obstetric emergency case: vulvovaginal hematoma – our four-year results 72 Özlem Yörük, Ayflegül Öksüzo¤lu, Elif Gül Yapar Eyi, Burcu K›sa Karakaya, Necati Hançerlio¤lu Evaluation of the measurement of ACTH, fibronectin, pentraxin 3 levels and 77 cervical length in pregnant women under threatened preterm delivery Filiz Aktenk, Burcu Artunç Ülkümen, Yeflim Güvenç, Halil Gürsoy Pala, Arzu Oran Hepatitis B seropositivity of pregnant women and the review of Turkish literature 83 Rabia Zehra Bakar, Banu Dane Posterior fossa anomalies: related anomalies and the methods of 89 pregnancy termination Emine Ayd›n, Mert Turgal, Sema Can, Özgür Özyüncü 96 Modified transabdominal cervico-isthmic cerclage: analysis of 16 cases Ebru Çelik Kavak, Salih Burçin Kavak, Yakup Baykufl, Hüsnü Çelik Results of fetal anomaly screening performed at 11–14 weeks 100 of gestation at a tertiary center Tu¤ba K›nay, Metin Kaplan, Mehmet Metin Altay, fiafak Özdemirci, Sinan Karadeniz, Ahmet Okyar Erol Case Report Intrafetal laser therapy in acardiac twin pregnancy: a case report 106 Resul Ar›soy, Oya Pekin, Kaan Pakay, Emre Erdo¤du, Oya Demirci, Murat Muhçu Volume Clinical Guidelines Diabates in pregnancy: diagnosis and treatment. -

Prof. Kypros Nicolaides, Kings College Hospital, London, UK
Prof. Kypros Nicolaides, Kings College Hospital, London, UK. 54 // VISIONS 36 INTERVIEW // ULTRASOUND // Aplio i-series, SMI, STE, MPI, Fetal Medicine VISIONS spoke with Prof. Kypros Nicolaides about using Canon's Aplio i-series systems in fetal medicine. Revolutionizing Fetal Medicine for Decades The Fetal Medicine Foundation, based in London, United Kingdom has made a significant contribution to advancing fetal medicine globally for more than 20 years. Established by Prof. Kyprianos ‘Kypros’ Nicolaides, it aims to improve the health of pregnant women and their babies through research and training in fetal medicine. Ultrasound scanning is, of course, absolutely fundamental in its work, and for many years, the Foundation has leveraged Canon Medical’s latest technology to advance science in this field. rof. Nicolaides is one of the How does the fetus think? How does world’s most well-known pio- it interact with the mother? How does Pneers in fetal medicine. He has it grow? How does it respond? And a real passion for fetal ultrasound. importantly, what happens if there are any problems with the pregnancy?” How it all started he explained. “So, I found my mission! “As a medical student in 1978 at Kings After I qualified in medicine, my whole College Hospital in London, I got to life was completely preoccupied with watch the moving image of a fetus fetal medicine. I studied Obstetrics within the uterus for the first time, and and Gynecology, because there was no it just fascinated me. I fell in love with other route into this area of medicine this. A thousand questions were raised at the time, but my obsession, my love, in my mind; What does the fetus feel? was for fetal medicine.” © 2021 CANON MEDICAL SYSTEMS // ULEU210078 VISIONS 36 // 55 “When I started in clinical practice, very great detail.