2014 Orlando, FL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
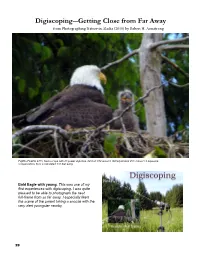
Digiscoping―Getting Close from Far Away from Photographing Nature in Alaska (2010) by Robert H
Digiscoping―Getting Close from Far Away from Photographing Nature in Alaska (2010) by Robert H. Armstrong Fujifilm FinePix 4700, Kowa scope with 20 power objective, f/2.8 at 1/74 second, ISO equivalent 200, minus 0.9 exposure compensation, from a calculated 231 feet away. Bald Eagle with young. This was one of my first experiences with digiscoping. I was quite pleased to be able to photograph the nest full-frame from so far away. I especially liked the scene of the parent taking a snooze with the very alert youngster nearby. 29 Digiscoping is taking pho- tos using a small digital camera mounted on a spotting scope. This setup can easily give you a lens equivalent of about 2,300 mm. That’s a very high magnification when you consider the biggest telephoto lenses for regular cameras are usually smaller than 1,000 mm and generally around 400 – 600 mm. Also, digiscoping equipment costs much less than high-quality large telephoto lenses and often weighs much less. Digiscoping allows you to photograph most wildlife from a considerable distance without disturbing them. From 40 feet away you can get close-up photos of songbirds. You can be more especially enjoy the way digiscoping Nikon Coolpix 995 digital camera. than 200 feet away for larger birds allows me to photograph birds (Some people seem to have trouble such as Great Blue Herons and at their nests without disturbing digiscoping with the newer model Bald Eagles. And you can be much them. 4500. I’m not sure why, but perhaps farther away for large mammals it is related to having a higher such as mountain goats and bears. -

Healthcare List of Medical Institutions Participating in Medishield Life Scheme Last Updated on 1 April 2020 by Central Provident Fund Board
1 Healthcare List of Medical Institutions Participating in MediShield Life Scheme Last updated on 1 April 2020 by Central Provident Fund Board PUBLIC HOSPITALS/MEDICAL CLINICS Alexandra Hospital Admiralty Medical Centre Changi General Hospital Institute of Mental Health Jurong Medical Centre Khoo Teck Puat Hospital KK Women's And Children's Hospital National Cancer Centre National Dental Centre National Heart Centre Singapore National Skin Centre National University Hospital Ng Teng Fong General Hospital Singapore General Hospital Singapore National Eye Centre Sengkang General Health (Hospital) Tan Tock Seng Hospital PRIVATE HOSPITALS/MEDICAL CLINICS Concord International Hospital Farrer Park Hospital Gleneagles Hospital Mt Alvernia Hospital Mt Elizabeth Hospital Mount Elizabeth Novena Hospital Parkway East Hospital Raffles Hospital Pte Ltd Thomson Medical Centre DAY SURGERY CENTRES A Clinic For Women A Company For Women A L Lim Clinic For Women Pte Ltd Abraham’s Ear, Nose & Throat Surgery Pte Ltd Access Medical (Bedok South) Access Medical (Bukit Batok) Access Medical (Circuit Road) Access Medical (East Coast) Access Medical (Jurong West) Access Medical (Kim Keat) Access Medical (Marine Terrace) Access Medical (Redhill Close) Access Medical (Tampines 730) Access Medical (Toa Payoh) Access Medical (Whampoa) 2 Access Medical (Teck Ghee) Adult & Child Eye (ACE) Clinic Advance Surgical Group Advanced Centre For Reproductive Medicine Pte. Ltd. Advanced Medicine Imaging Advanced Urology (Parkway East Medical Center) Agape Women’s Specialists -

Industrial Sponsorships
Introduction to Industrial Sponsorships Candidates who have the passion to become healthcare professionals and would like to seek financial sponsorship in the healthcare sector may approach the following organisations to discuss their interest in joining the sector. Please note that any sponsorship awarded may typically come with obligations to serve a working bond with the sponsoring organisation. Parkway Pantai Student Scholarship [Radiology] Parkway Pantai is one of Asia’s largest integrated private healthcare groups operating in Singapore, Malaysia, India, China, Brunei and United Arab Emirates. For over 40 years, its Mount Elizabeth, Gleneagles, Pantai and Parkway brands have established themselves as the region’s best known brands in private healthcare, synonymous with best-in-class patient experience and outcomes. It is part of IHH Healthcare, the world’s second largest healthcare group by market capitalisation. IHH operates more than 10,000 licensed beds across 50 hospitals in 10 countries worldwide. In Singapore, Parkway Pantai is the largest private healthcare operator with four JCI- accredited, multi-specialty tertiary hospitals - Mount Elizabeth Hospital, Mount Elizabeth Novena Hospital, Gleneagles Hospital and Parkway East Hospital. It also owns Parkway Shenton, a large network of primary healthcare clinics and services, ParkwayHealth Radiology, ParkwayHealth Laboratory and Parkway College. Types of Sponsorships: Partial / Full Sponsorships Bond Duration: 3 years upon graduation / 6 years upon graduation Contact Person: Linus Leow Email Address: [email protected] Website: https://www.parkwayhospitals.com/ Industrial Sponsorships by other Healthcare Institutions The following organisations have also sponsored candidates in the past and may offer sponsorships for accepted candidates of this programme. You may wish to visit the organisations’ websites for more details or contact the relevant person in the respective organisation by phone or in writing to find out the selection procedures. -

Singapore Medical Council 2018 List of Accredited Cme
SINGAPORE MEDICAL COUNCIL 2018 LIST OF ACCREDITED CME ACTIVITIES FOR CATEGORIES 1C / 2 / 3A / 3B CORE ANAESTHESIOLOGY ACTIVITIES / PROGRAMMES Category 1A: Participation at local pre-approved activities 1 Anaesthetic Topics (RHs) Anaesthetic Topics held at Mt. Alvernia Hospital by College of Anaesthesiology (CAS) & 2 Singapore Society of Anaesthesiologists 3 Cardiac Subspecialty Teaching (SGH) 4 ICU Teaching/ Round (RHs) 5 Journal Reading (RHs) 6 Morbidity and Mortality Meetings in Private hospitals 7 Mortality & Morbidity (RHs) 8 Peer Reviewed Learning (Private Hospitals) 9 Pain Subspecialty Teaching (RHs & Private Hospitals) Category 1B: Participation at local ad-hoc activities 1 Advanced Regional Anaesthesia & Ultrasound-Guided Peripheral Nerve Block Technique Annual Scientific Meeting of Academy of Medicine Singapore & Singapore Society of 2 Anaesthesiologists 3 Biennial General Scientific Meeting (GSM) of the Society of Intensive Care Medicine 4 Monthly Combined Anaesthetic Meeting 5 Refresher course in Anaesthesia organized by College of Anaesthesiologists, Singapore 6 Talks co-organised by society of anesthesiologists and /or College of anesthesiologists Category 1C: Participation at overseas ad-hoc activities 1 American Society of Anesthesiologists Annual Meeting (ASA) 2 American Society of Critical Care Anesthesiologists Annual Meeting 3 Annual Scientific Meeting, Association of Anaesthetist, UK 4 ASEAN Congress of Anaesthesiology 5 Asia-Pacific Association of Critical Care Medicine (APACCM) 6 Asian-Australasian Congress of Anaesthesiology -

College of Anaesthesiologists, Singapore
36 ANNUAL REPORT 2012 COLLEGE OF ANAESTHESIOLOGISTS, SINGAPORE Council 2012-2013 8th Annual General Meeting The office bearers for 2012-2013 Council are: The 8th Annual General Meeting (AGM) of the College was held on 19 May 2012, 1:15 pm at the York Hotel, Rose Room. President: Dr Chong Jin Long A total of 25 Fellows were present at the AGM. President-Elect: Dr Philip Tseng Vice President: Dr Boey Wah Keong Honorary Secretary: Dr Ti Lian Kah Honorary Treasurer: Dr Kwek Tong Kiat Council Members: Dr Agnes Ng Suah Bwee Dr Sophia Chew Activities Combined Anaesthesia Meetings The following Combined Anaesthesia Meetings were co-organized with the Singapore Society of Anaesthesiologists: 25 February, National University Health System (Tower Block) Symposium – Current Cardiac Topics Chairperson: Dr Sophia Chew Preoperative Management of Patients with Implantable Cardiac Dr WS Teo Device Cardiologist, Mt Elizabeth Hospital Patients with Acute Coronary Syndrome on Antiplatelet Therapy Dr Tan Huay Cheem Going for Surgery: Balancing the Risk of Ischemia and Bleeding Cardiologist, National University Hospital Cardiac Anaesthesia - The Journey Dr Boey Wah Keong Anaesthesiologists, Gleneagles Hospital 28 April, National University Health System (Tower Block) Pain Adjuvants for Today Dr Edwin Seet Consultant, Department of Anaesthesia, Khoo Teck Phuat Hospital Thoracic Anaesthesia the Occassional Thoracic Anaesthesia Dr Suresh Paranjothy Provide Consultant, Department of Anaesthesia, National University Health System 30 June, Singapore General Hospital -

AIA Singapore Frequently Asked Questions Letter of Guarantee
AIA Singapore 1 Robinson Road, AIA Tower Singapore 048542 T : 1800 248 8000 AIA.COM.SG Frequently Asked Questions Letter of Guarantee Service for AIA HealthShield Gold Series Policyholder 1. What is a Letter of Guarantee (“LOG”)? The LOG is a letter issued by AIA Singapore Private Limited to selected Singapore Government Restructured Hospitals, Private Hospitals and Medical Institutions for full or partial waiver of hospital upfront cash deposit in the event of hospitalisation and/or surgery. However, the policyholders may be required to settle the hospital bills following the hospital discharge. 2. What type of medical policy is entitled to the LOG service? The LOG service is only offered to Medisave‐approved Integrated AIA HealthShield Gold series* policyholders. Non‐integrated medical policy (such as AIA Pink Of Health, Hospital & Surgical Benefit Rider, AIA HealthShield Gold Max Foreigner, Comprehensive Medical Plan, AIA Platinum Heath, etc.) are not entitled to the LOG service. *AIA HealthShield Gold series plans include AIA HealthShield Gold Plan A, AIA HealthShield Gold Plan A Public Service, AIA HealthShield Gold Prestige, AIA HealthShield Gold Prestige Public Service, AIA HealthShield Gold Elite, AIA HealthShield Gold Elite Special, AIA HealthShield Gold Max and AIA HealthShield Gold Max Special. We are pleased to inform that from 6 August 2013, the LOG service will be extended to take into consideration our policyholder’s coverage under AIA HealthShield Gold Essential. 3. Which hospitals accept the LOG service? The LOG service -

College of Obstetricians and Gynaecologists, Singapore 2007
COLLEGE OF OBSTETRICIANS AND GYNAECOLOGISTS, SINGAPORE 2007 COLLEGE OF OBSTETRICIANS AND GYNAECOLOGISTS, SINGAPORE (INCORPORATED IN THE REPUBLIC OF SINGAPORE) COMPANY REGISTRATION NUMBER: 200410332N 2007-2008 Council Photo was taken at the 4th COGS Annual Lecture & Dinner on 21st July 2007 1st Row (from Left) : Dr SH Yeo, Dr Lai Fon-Min, Dr Chang Tou Choong, Prof Rajmohan Nambiar (Guest-of-Honour), Prof Tony Chung (Guest Lecturer), Dr Ho Tew Hong, Dr Sheila Loh Back Row (from Left) : Dr Jothi Kumar, Dr Fong Chuan Wee, Dr Roy Ng, Dr Kelvin Tan, Dr Arijit Biswas, Dr Tay Eng Hseon, Dr Suresh Nair 4th COGS Annual Lecture & Dinner: Dr TC Chang presenting a token of appreciation to Guest Lecturer, Prof Tony Chung 54 COLLEGE OF OBSTETRICIANS AND GYNAECOLOGISTS, SINGAPORE 2007 Annual Report of the 2007-2008 Council Co-opted Members: Dr Chang Tou Choong Dr Lai Fon-Min 1. THE COUNCIL Section of Reproductive Medicine The 3rd Annual General Meeting of the College of Chairman: Dr Loh Kia Ee Sheila Obstetricians and Gynaecologists, Singapore, was held on Vice-Chairman: Dr Yu Su Ling 11 May 2007, Friday, at 6.30pm at Lecture Theatre, Honorary Secretary: Dr Fong Yoke Fai Training Centre, KK Women’s & Children’s Hospital, Committee Members: Dr Loh Seong Feei 100 Bukit Timah Road, Singapore 229899. Dr Koh Chung Fai Co-opted Members: Dr Cheng Li Chang The following office-bearers for the year 2007 – 2008 were elected: Dr Suresh Nair Dr P C Wong President: Dr Chang Tou Choong Immediate Past President: Dr Ho Tew Hong Section of Urogynaecology Vice-President: Dr Lai Fon-Min Chairman: Dr Ng Kwok Weng, Roy Honorary Secretary & Vice-Chairman: Dr Han How Chuan, William Co-opted Member: Dr Suresh Nair Committee Members: Dr Lee Lih Charn Honorary Treasurer & Chairperson, Dr Lee Weng Soon, James Section of Reproductive Medicine: Dr Loh Kia Ee, Sheila Co-opted Members: Dr Chua Hong Liang Council Members : Dr Arijit Biswas Dr See Tho Kai Yin Dr Fong Chuan Wee, Francis 3. -
Astrophotography: Tips, Tricks, and Techniques
Astrophotography: Tips, Tricks, and Techniques Clay S. Turner Sept. 24, 2011 Astrophotography without a Telescope • Use camera on a tripod • Use remote shutter release • Do long exposures with large apertures (“Fast Lenses”) • Include landscape with sky to make image interesting. • Modern low noise DSLRs allow high ISOs to facilitate short exposures. Yellowstone National Park Lowell Observatory Iridium Flares Lowell Observatory Piggyback Astrophotography • Here you attach your camera onto a telescope to use the scope’s tracking. • Camera uses its own lens and not the scope’s optics. • Useful for medium to large areas of the sky. Shot with DSLR and 180 mm lens Three basic ways to image through your telescope. • Prime Focus • Eyepiece Projection • Afocal Photography Prime Focus Imaging • The telescope’s objective is used in place of a “long lens” in photography. Thus the camera, sans lens, is connected where the eyepiece normally goes. • DSLRs are usually used in this mode of Astro-Imaging. • Preferred method of imaging by professional astronomers. Eyepiece Projection • Just like with Prime Focus photography, a camera is used without its lens. But in this case the eyepiece is used to magnify and project the image onto the camera’s sensor (film). • There are special adaptors that will contain the eyepiece and also hold the camera with variable spacing (magnification) permitted. Afocal Photography • In this case the telescope with its eyepiece is focused so an observer while looking into the eyepiece sees the object clearly. Then a camera with a lens is then used to image the object while looking into the eyepiece. Birders often call this technique “digiscoping.” Simple low cost “point and shoot” cameras may be used this way. -

Singapore Hospitals Room Charges
ROOM CHARGES DAILY RATE (S$) NO HOSPITAL WARD TYPE & DESCRIPTION ASUMSI RATE Rp.9.500/S$ INCLUDES 7% GST 1 SINGAPORE GENERAL HOSPITAL Standard Ward Class C (9-bedded room) From S$ 35 per day Rp 332,500 Standard Ward Class B2 (6-bedded room) From S$ 70 per day Rp 665,000 Standard Ward Class B2+ (air conditioned 5-bedded From S$ 140 per day Rp 1,330,000 room) Standard Ward Class B1 (air conditioned 4-bedded From S$ 226.84 per day Rp 2,154,980 room) Standard Ward Class A1+/A1 (single room) From S$ 422.65 / 396.97 per day Rp. 4,015,175 / Rp. 3,771,215 2 ALEXANDRA HOSPITAL Class A (Single bedroom) S$ 336 per day Rp 3,192,000 Class B1 (4-bed room) S$ 235 per day Rp 2,232,500 Class B2 (6-bed room) S$ 219 per day Rp 2,080,500 Class C (Open ward) S$ 187 per day Rp 1,776,500 3 CHANGI GENERAL HOSPITAL Class A (Single bedroom) From S$ 390 per day Rp 3,705,000 Class B1 (4-bed room) From S$ 289 per day Rp 2,745,500 Class B2 (6-bed room) From S$ 249 per day Rp 2,365,500 Class C (Open ward) From S$ 205 per day Rp 1,947,500 4 GLENEAGLES HOSPITAL Gleneagles Suite S$ 6,677 Rp 63,431,500 Tanglin Suite S$ 5,361 Rp 50,929,500 Napier / Nassim Suite S$ 2,729 Rp 25,925,500 Dalvey Suite S$ 1,314 Rp 12,483,000 Executive Deluxe Suite S$ 1,314 Rp 12,483,000 Executive Suite S$ 1,095 Rp 10,402,500 Superior Room S$ 766 Rp 7,277,000 Single Room S$ 585 Rp 5,557,500 Two-Bedded S$ 321 Rp 3,049,500 Four Bedded S$ 239 Rp 2,270,500 KK WOMAN'S & CHILDREN'S 5 Rooms - A1 (Single) From S$ 395.90 per day Rp 3,761,050 HOSPITAL Rooms - B1 (4-Beds) From S$ 224.70 per day Rp 2,134,650 -

Instruction Manual
Instruction Manual Cassini 76 DOB English version 8.2014 Rev A 1 The Zoomion® Cassini 76 DOB Congratulations on the purchase of the new Zoomion® Cassini 76 DOB. This small telescope will give you hours of fun, with its all optical glass mirror and super compactness, and it is the ideal companion to start in the world of amateur astronomy. With this telescope you will be able to see the craters on the Moon, star clusters, some nebulae and a glimpse of the Jupiter disc features and its Galilean moons and the rings of Saturn. We have included many accessories so it will be easy to use this telescope. 1. Included parts we have included several accessories that will make the use of the telescope easier and fun, please take a look at the list of the parts so you can identify them in the future. 1. 1.5x Erecting Lens; 2. 2x magnification Barlow Lens; 3, 4, 5 and 6. Four eyepieces 1.25” (31.75mm); a H20mm, H12.5mm, H6mm and a SR4mm eyepiece; 2. Getting Started. It is very simple to get started. Here is how the telescope works. The telescope aperture should point to the object being observed. The mirror on back of the tube will gather the light coming from the object and reflects it to the secondary mirror that brings it to the eyepiece. Close to the aperture there is the focuser. The focuser moves up and down to get a precise focused image. At the focuser one can use the supplied accessories. Different accessories combinations give different results, such as different image magnifications or correct image for example. -

List of Medical Providers for Direct Billing Facilities in Singapore
LIST OF MEDICAL PROVIDERS FOR DIRECT BILLING FACILITIES IN SINGAPORE INPATIENT SERVICES (Note: Prior approval is required) Name of Hospital Address I. Gleneagles Hospital 6A Napier Road, Singapore 258500 II. Mount Elizabeth Hospital 3 Mount Elizabeth, Singapore 228510 III. Mount Elizabeth Novena Hospital 38 Irrawaddy Road, Singapore 329563 II. Mount Elizabeth Hospital 3 Mount Elizabeth, Singapore 228510 IV. Parkway East Hospital 321 Joo Chiat Place, Singapore 427990 V. Raffles Hospital 585 North Bridge Road, Raffles Hospital #11-00, Singapore 188770 OUTPATIENT SERVICES Name of Clinic Address I. Group of Raffles Medical Clinics Please visit the following website to download the latest clinic location listing of Raffles Medical Clinics: http://www.rafflesmedicalgroup.com/family-medicine/clinic-location- listing II. Parkway Shenton Group Clinics (for clinic schedule, please visit: http://www.parkwayshenton.com) 1) Alexandra Retail Centre - Shenton Wellness Centre 460 Alexandra Road, #02-15 PSA Building (Alexandra Retail Centre), Singapore 119963 2) Buangkok MRT - Shenton Medical Group 10 Sengkang Central, #01-04 Buangkok NEL MRT Station, Singapore 545061 3) Bukit Panjang Plaza - Shenton Medical Group No.1 Jelebu Road, #03-02 Bukit Panjang Plaza, Singapore 677743 4) Clementi Central - Shenton Family Medical Clinic Blk 451 Clementi Avenue 3, #01-309, Singapore 120451 5) Dhoby Xchange - Shenton Medical Group 11 Orchard Road, #B2-01 Dhoby Ghaut MRT Station, Singapore 238826 6) Esplanade Xchange - Shenton Medical Group 90 Bras Basah Road, #B1-02 -

01-27 Wex Christmas 2019.Indd
XXX 1 Gold Service Award 2014-2018 Good Service Award Winner 2008-2019 XXX XXX CONTENTS Wishing you a Store Locations page 4 Competition Merry Christmas page 5 DSLRs, CSCs & Lenses page 7-23 from the team at Wex Photo Video Lenses page 24-27 Gift Ideas With many options available in an ever-changing technological landscape, page 28-29 modern photographers and videographers need knowledge and expertise Digital Compacts to ensure they get the right kit for the job. As the UK’s biggest and most page 30-31 trusted photo retailer*, Wex Photo Video is the place to fi nd that expertise. Action Cameras Thanks to our unrivalled range of over 20,000 products and a customer- & Drones service team made up of photographers and fi lmmakers, Wex can meet page 32-33 the demands of even the most complicated project. To help you get what you need when you need it, we ship seven days a week and have a variety Pro Video & © Clive Booth, Canon Ambassador of buying options, from quality-assured used gear to personal fi nance, Accessories including interest-free credit on many of the latest products. In 2019, page 34-35 we have launched more features to make life easier for our customers, including the addition of PayPal Express to our website and a free camera Memory Cards set-up service, available at stores across the country. page 35 Tripods CAPTURE THE To access any of our services, including gear, events and advice, you can call us seven days a week on 01603 486413, explore our website at page 38-41 wex.co.uk or visit one of our eight shops around the UK.