For Peer Review Only Journal: BMJ Open
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Water Safety Policy in Scotland —A Guide
Water Safety Policy in Scotland —A Guide 2 Introduction Scotland is surrounded by coastal water – the North Sea, the Irish Sea and the Atlantic Ocean. In addition, there are also numerous bodies of inland water including rivers, burns and about 25,000 lochs. Being safe around water should therefore be a key priority. However, the management of water safety is a major concern for Scotland. Recent research has found a mixed picture of water safety in Scotland with little uniformity or consistency across the country.1 In response to this research, it was suggested that a framework for a water safety policy be made available to local authorities. The Royal Society for the Prevention of Accidents (RoSPA) has therefore created this document to assist in the management of water safety. In order to support this document, RoSPA consulted with a number of UK local authorities and organisations to discuss policy and water safety management. Each council was asked questions around their own area’s priorities, objectives and policies. Any policy specific to water safety was then examined and analysed in order to help create a framework based on current practice. It is anticipated that this framework can be localised to each local authority in Scotland which will help provide a strategic and consistent national approach which takes account of geographical areas and issues. Water Safety Policy in Scotland— A Guide 3 Section A: The Problem Table 1: Overall Fatalities 70 60 50 40 30 20 10 0 2010 2011 2012 2013 Data from National Water Safety Forum, WAID database, July 14 In recent years the number of drownings in Scotland has remained generally constant. -

Greenland Barnacle 2003 Census Final
GREENLAND BARNACLE GEESE BRANTA LEUCOPSIS IN BRITAIN AND IRELAND: RESULTS OF THE INTERNATIONAL CENSUS, MARCH 2003 WWT Report Authors Jenny Worden, Carl Mitchell, Oscar Merne & Peter Cranswick March 2004 Published by: The Wildfowl & Wetlands Trust Slimbridge Gloucestershire GL2 7BT T 01453 891900 F 01453 891901 E [email protected] Reg. charity no. 1030884 © The Wildfowl & Wetlands Trust All rights reserved. No part of this document may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the prior permission of WWT. This publication should be cited as: Worden, J, CR Mitchell, OJ Merne & PA Cranswick. 2004. Greenland Barnacle Geese Branta leucopsis in Britain and Ireland: results of the international census, March 2003 . The Wildfowl & Wetlands Trust, Slimbridge. gg CONTENTS Summary v 1 Introduction 6 2 Methods 7 3 Results 8 4 Discussion 13 4.1 Census total and accuracy 13 4.2 Long-term trend and distribution 13 4.3 Internationally and nationally important sites 17 4.4 Future recommendations 19 5 Acknowledgements 20 6 References 21 Appendices 22 ggg SUMMARY Between 1959 and 2003, eleven full international surveys of the Greenland population of Barnacle Geese have been conducted at wintering sites in Ireland and Scotland using a combination of aerial survey and ground counts. This report presents the results of the 2003 census, conducted between 27th and 31 March 2003 surveying a total of 323 islands and mainland sites along the west and north coasts of Scotland and Ireland. In Ireland, 30 sites were found to hold 9,034 Greenland Barnacle Geese and in Scotland, 35 sites were found to hold 47,256. -
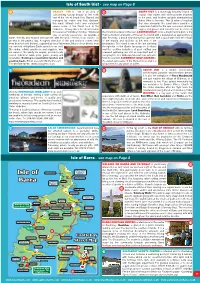
Isle of Barra - See Map on Page 8
Isle of South Uist - see map on Page 8 63 ORASAY INN is set in an area of 66 SOUTH UIST is a stunningly beautiful island of outstanding natural beauty at the north crystal clear waters with white powder beaches end of the Isle of South Uist. Owned and to the west, and heather uplands dominated by managed by Isobel and Alan Graham, Beinn Mhor to the east. The 20 miles of machair this small, intimate hotel and restaurant that runs alongside the sand dunes provides a serves some of the fi nest food in the marvellous habitat for the rare corncrake. Golden Hebrides. Orasay Inn is the ideal location eagles, red grouse and red deer can be seen on for a special Hebridean holiday. Whatever the mountain slopes to the east. LOCHBOISDALE, once a major herring port, is the type of activity you prefer, we provide a main settlement and ferry terminal on the island with a population of approximately warm, friendly and relaxed atmosphere, with the best of fresh, local cuisine, as 300. Recently, a brand new marina has opened, with a good walk from the village an end to the perfect day. A superb selection of fi sh and seafood comes fresh to the marina and facilities at the end of the from boat to hotel kitchen, supplied by local fi shermen. Much of our beef is from breakwater. The island is one of the last surviving our own fold of Highland Cattle, raised on our croft. strongholds of the Gaelic language in Scotland Discerning, reliable producers and suppliers, who and the crofting industries of peat cutting and are aware of the quality we require, provide locally seaweed gathering are still an important part of reared Hebridean lamb, pork, game, poultry and everyday life. -

Visiting the Islands in the Sound of Barra Paul A. Smith, Richard
Visiting the islands in the Sound of Barra Paul A. Smith, Richard Pankhurst This article originally appeared in the Curracag Newsletter, but was originally intended for Hebridean Naturalist. Richard Pankhurst passed away in 2013. In late July 2003, the authors and Jane & Eric Twelves spent several days visiting various islands in the Sound of Barra, to undertake botanical surveys. There are no previous data for most of these islands, although there is a fairly comprehensive list for Fuday, and a rather short one for Fiaray. J. W. Heslop Harrison visited many of these islands while undertaking botanical surveys, and he published several articles (for example Harrison et al. 1939), but these are mostly not specific about which plants are found on which islands. We hoped to update these and to add to the botanical knowledge of these areas. The islands we visited are shown in Table 1. Table 1: Islands visited 25-27 July 2003 Island Observed grazing Number of species Total number of intensity found in July 2003 species previously known Fuday ungrazed 97 206 Fiaray grazed 112 22 Gighay grazed 126 0 Hellisay grazed 117 0 Orosay grazed 82 0 Lingay-fhada grazed 67 0 Fuiay grazed 122 0 Flodday grazed 106 0 Garbh Lingay ungrazed 79 0 Fuday Fuday is the best known botanically of the uninhabited islands in the Sound of Barra, particularly for its variety of orchids (eight species and four hybrids amongst the 206 known species), and had been visited by RJP twice before (once as part of a Botanical Society of the British Isles (BSBI) field meeting, see Pankhurst 1999). -

The Western Isles of Lewis, Harris, Uists, Benbecula and Barra
The Western Isles of Lewis, Harris, Uists, Benbecula and Barra 1 SEATREK is based in Uig on 5 UIG SANDS RESTAURANT is a newly Let the adventure begin! Lewis, one of the most beautiful opened licensed restaurant with spectacular locations in Britain. We offer views across the beach. Open for lunches unforgettable boat trips around and evening meals. Booking essential. the Hebrides. All welcome, relaxed atmosphere and family Try any of our trips for a great friendly. Timsgarry, Isle of Lewis HS2 9ET. family experience with the Tel: 01851 672334. opportunity of seeing seals, Email: [email protected] basking sharks, dolphins and www.uigsands.co.uk many species of birds. DOUNE BRAES HOTEL: A warm welcome awaits you. We especially 6 Leaving from Miavaig Seatrek RIB Short Trips cater for ‘The Hebridean Way’ for cyclists, walkers and motorcyclists. Harbour, Uig, Isle of Lewis. We have safe overnight storage for bicycles. We offer comfortable Tel: 01851 672469. Sea Eagles & Lagoon Trip .............................. 2 hours accommodation, light meals served through the day and our full www.seatrek.co.uk Island Excursion ................................................. 3 hours evening menu in the evening. Locally sourced produce including Email: [email protected] Customised Trips ............................................... 4 hours our own beef raised on our croft, shellfi sh and local lamb. There’s a Fishing Trip ........................................................... 2 hours Gallan Head Trip ................................................. 2 hours good selection of Malt Whiskies in the Lounge Bar or coffees to go Sea Stacks Trip ................................................... 2 hours whilst you explore the West Side of the Island. Tel: 01851 643252. Email: [email protected] www.doune-braes.co.uk 2 SEA LEWIS BOAT TRIPS: Explore the 7 BLUE PIG CREATIVE SPACE: coastline North and South of Stornoway Carloway’s unique working studio and in our 8.5m Rib. -

Greenland Barnacle Geese Brant Leucopsis in Britain and Ireland: Results of the International Census, Spring 2018
Scottish Natural Heritage Research Report No. 1154 Greenland barnacle geese Brant leucopsis in Britain and Ireland: results of the International census, spring 2018 RESEARCH REPORT Research Report No. 1154 Greenland barnacle geese Brant leucopsis in Britain and Ireland: results of the International census, spring 2018 For further information on this report please contact: Simon Cohen Scottish Natural Heritage Fodderty Way Dingwall Business Park DINGWALL IV15 9XB Telephone: 01463 701611 E-mail: [email protected] This report should be quoted as: Mitchell, C. & Hall, C. 2020. Greenland barnacle geese Branta leucopsis in Britain and Ireland: results of the International census, spring 2018. Scottish Natural Heritage Research Report No. 1154. This report, or any part of it, should not be reproduced without the permission of Scottish Natural Heritage. This permission will not be withheld unreasonably. The views expressed by the author(s) of this report should not be taken as the views and policies of Scottish Natural Heritage. © Scottish Natural Heritage 2020. RESEARCH REPORT Summary Greenland barnacle geese Brant leucopsis in Britain and Ireland: results of the International census, spring 2018 Research Report No. 1154 Project No: 114469 Contractor: The Wildfowl & Wetlands Trust Year of publication: 2020 Keywords Greenland barnacle goose; Islay; Scotland; census Background Between 1959 and 2018, fourteen full international surveys of the Greenland population of barnacle goose Branta leucopsis have been conducted at wintering sites in Scotland and Ireland using a combination of aerial survey and ground counts. This report presents the results of the 2018 census in Scotland, conducted primarily between 19-20 March, and also includes the total count in Ireland in order to estimate the total population size. -
Barra – the Physical Background
Barra Barra - the Physical Background Noel Fojut AS WITH all islands, the physical facts of Barra's location, geology and climate have a profound influence upon the nature of life for inhabitants and visitors. Even today the constraints of time, tide and weather are no respecters of timetables, while weather variations within a single day can give the lie to the changing seasons. How much more so in, centuries past, must the physical geography of Barra have determined human options, closing off opportunities with one hand while opening up connections with the other. Determinism may be an unpopular concept in modern science, yet anyone spending a winter on Barra might think again. Barra's story begins in an unimaginably distant geological past. An area oflighter crustal rocks, a 'craton' as geologists of 3000 million years later would term it, formed the basis for an early continent (Fettes et al 1992: passim)1. This area, of unknown extent but including much of what is today the Western Isles, rode high above the heavier rocks of the ocean floor. Despite endless crustal movements, continents spreading and being destroyed, oceans opening and closing, these rocks remained unabsorbed. Most of the upper crust of the Earth from that early date has long been re-cycled, drawn down into the lower reaches, melted and re-cycled. But not the rocks of Barra. Despite intense pressure and folding, sometimes as much as 25 km below the surface at the root of an ancient mountain chain comparable to the Alps or the Andes, they survived, to form what today we call the Lewisian gneiss. -
(DQIP) Trial: Case Study Evaluation of Adoption and Maintenance of a Complex Intervention to Reduce High-Risk Primary Care Prescribing
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2016-015281 on 10 March 2017. Downloaded from Process evaluation of the Data-driven Quality Improvement in Primary Care (DQIP) trial: case study evaluation of adoption and maintenance of a complex intervention to reduce high-risk primary care prescribing Aileen Grant,1 Tobias Dreischulte,2,3 Bruce Guthrie3 To cite: Grant A, ABSTRACT Strengths and limitations of this study Dreischulte T, Guthrie B. Objective: To explore how different practices Process evaluation of the responded to the Data-driven Quality Improvement in ▪ Data-driven Quality This is a comprehensive, preplanned process Primary Care (DQIP) intervention in terms of their Improvement in Primary Care evaluation which includes a third of all practices (DQIP) trial: case study adoption of the work, reorganisation to deliver the which participated in the Data-driven Quality Bibliothek. Protected by copyright. evaluation of adoption and intended change in care to patients, and whether Improvement in Primary Care (DQIP) stepped- maintenance of a complex implementation was sustained over time. wedge cluster-randomised trial. intervention to reduce high- Design: Mixed-methods parallel process evaluation of ▪ The evaluation sampled four practices which risk primary care prescribing. a cluster trial, reporting the comparative case study of rapidly implemented the intervention and all six BMJ Open 2017;7:e015281. purposively selected practices. practices which failed to implement the interven- doi:10.1136/bmjopen-2016- Setting: Ten (30%) primary care practices tion to some degree. 015281 participating in the trial from Scotland, UK. ▪ A strength of the study is the use of qualitative Results: Four practices were sampled because they data from interviews and observational field ▸ Prepublication history and had large rapid reductions in targeted prescribing. -
Western Isles Native Woodland Restoration Survey Report Restoration & Enhancement of Native Woodland Resources Sapling
Western Isles Native Woodland Restoration Survey Report restoration & enhancement of native woodland resources Sapling Native woodland, Bowglass, Isle of Harris Dog Rose Acknowledgements The author would like to thank Scottish Natural Heritage the many people who provided 32 Francis Street information, guidance and helped survey sites throughout the duration Stornoway of this project. They include Stewart Isle of Lewis Angus, Simon Fraser, Brendan Harty, Kevin Kennedy, Carol Knott, Mark T: 01851 705258 MacDonald, Iain MacIver, Kenny MacKay, Donald MacLeod, Duncan MacPherson and Paul Smith. Comhairle nan Eilean Siar This report has been part-funded by Sandwick Road Scottish Natural Heritage Stornoway Isle of Lewis HS1 2BW T: 01851 703773 F: 01851 709287 Western Isles Native Woodland Restoration Survey Report 2 Contents Summary .....................................................................................................................................5 Context .....................................................................................................................................5 the Western Background ...................................................................................................................................6 Methodology ...............................................................................................................................7 Isles once Key Sites .....................................................................................................................................8 -

Archaeological Remains on Uist's Machair: Threats and Potential
Archaeological remains on Uist’s machair: threats and potential by Mike Parker Pearson, Department of Archaeology, University of Sheffield, Sheffield Jacqui Mulville and Niall Sharples School of History and Archaeology, University of Cardiff, Cardiff Helen Smith Department of Conservation Science, University of Bournemouth, Bournemouth Scottish Archaeological Internet Report 48, 2011 www.sair.org.uk CONTENTS List of Illustrations. 58 1 Abstract . .59 2 Introduction. 60 3 The Principal Threat to Machair Sites: Rabbit Damage . .62 4 The Quality of Archaeological Evidence on the Machair. 64 4.1 Stratigraphy and preserved floor accumulations. 64 4.2 Clarity of sequences . 6 4.3 Bone preservation . 6 4.4 Juxtaposed calcareous, acidic and waterlogged conditions. 6 5 The Machair Sequence of Settlement and Land Use . .67 6 Development of Archaeological Methods and Techniques. 69 6.1 Environmental archaeology. 69 6.2 From tapestries and test pits to open-area excavation. 69 6.3 Analysing house floors. 69 6.4 Absolute dating . 70 7 Diet: Residues and Isotopes. 71 7.1 Inferring mummification from skeletons. 71 8 Priorities for the Future . .72 9 Acknowledgements. .74 10 References . .75 11 A Bibliography of the ‘SEARCH’ Project . .77 11.1 Monographs. 77 11.2 Books (popular accounts). 77 11.3 Academic published papers. 77 11.3.1 Archaeology . 77 11.3.2 Palaeoecology . 79 11.3.3 Ecology. 81 11.4 Popular accounts (not including newspaper reports) . 82 11. Unpublished reports (not including MSc and PhD theses). 82 11.6 PhD theses and MA/MSc dissertations . 84 7 LIST OF ILLUSTRATIONS 1 The southern islands of the Western Isles . -

Scottish Islands
This is the definitive list for Scottish Islandbaggers. (Islandbagging = The obsessive compulsion to visit island summits.) Rick Livingstone’s Tables of THE ISLANDS OF SCOTLAND ¾ A register of all islands 15 hectares, or more, in area. That’s 37 acres, and roughly equates to a circular island ¼ of a mile across. ¾ Includes tidal islands, islands which are bridged or have cause-ways and freshwater islands. Comments & suggestions welcome: e-mail: [email protected] or landmail to: Rick Livingstone, Overend House, Greysouthen, Cockermouth, Cumbria, CA130UA, U.K. © Rick Livingstone 2011 [v300111] THE ISLANDS OF SCOTLAND IN REGIONAL ORDER Name Region Location O.S. Grid ref Summit name Height Area & No. Map (summit) (metres) Region 1. Solway & the Clyde 1. Ardwall Island 1.1 Gatehouse of Fleet 83 572-493 - none - 34 19h 2. Ailsa Craig 1.2 SE of Arran 76 018-999 The Cairn 338 99h 3. Sanda 1.3 S of Kintyre 68 730-044 - none - 123 1.2km2 4. Davaar 1.4 Campbeltown 68 758-200 - none - 115 1km2 5. Holy Island 1.5 E of Arran 69 063-298 Mullach Mor 314 2.5km2 6. Arran 1.6 East of Kintyre 69 416-992 Goat Fell 874 430km2 7. Little Cumbrae 1.7 SE of Bute 63 143-514 Lighthouse Hill 123 3.5km2 8. Great Cumbrae 1.8 SE of Bute 63 169-570 Barbay Hill 127 11km2 9. Inchmarnock 1.9 W of Bute 63 019-602 - none - 60 2.5km2 10. Bute 1.10 N of Arran 63 043-699 Windy Hill 278 120km2 Region 2. -

Author(S): Title: Year
This publication is made freely available under ______ __ open access. AUTHOR(S): TITLE: YEAR: Publisher citation: OpenAIR citation: Publisher copyright statement: This is the ______________________ version of an article originally published by ____________________________ in __________________________________________________________________________________________ (ISSN _________; eISSN __________). OpenAIR takedown statement: Section 6 of the “Repository policy for OpenAIR @ RGU” (available from http://www.rgu.ac.uk/staff-and-current- students/library/library-policies/repository-policies) provides guidance on the criteria under which RGU will consider withdrawing material from OpenAIR. If you believe that this item is subject to any of these criteria, or for any other reason should not be held on OpenAIR, then please contact [email protected] with the details of the item and the nature of your complaint. This publication is distributed under a CC ____________ license. ____________________________________________________ Downloaded from http://bmjopen.bmj.com/ on January 9, 2018 - Published by group.bmj.com Open Access Research Process evaluation of the Data-driven Quality Improvement in Primary Care (DQIP) trial: case study evaluation of adoption and maintenance of a complex intervention to reduce high-risk primary care prescribing Aileen Grant,1 Tobias Dreischulte,2,3 Bruce Guthrie3 To cite: Grant A, ABSTRACT Strengths and limitations of this study Dreischulte T, Guthrie B. Objective: To explore how different practices Process