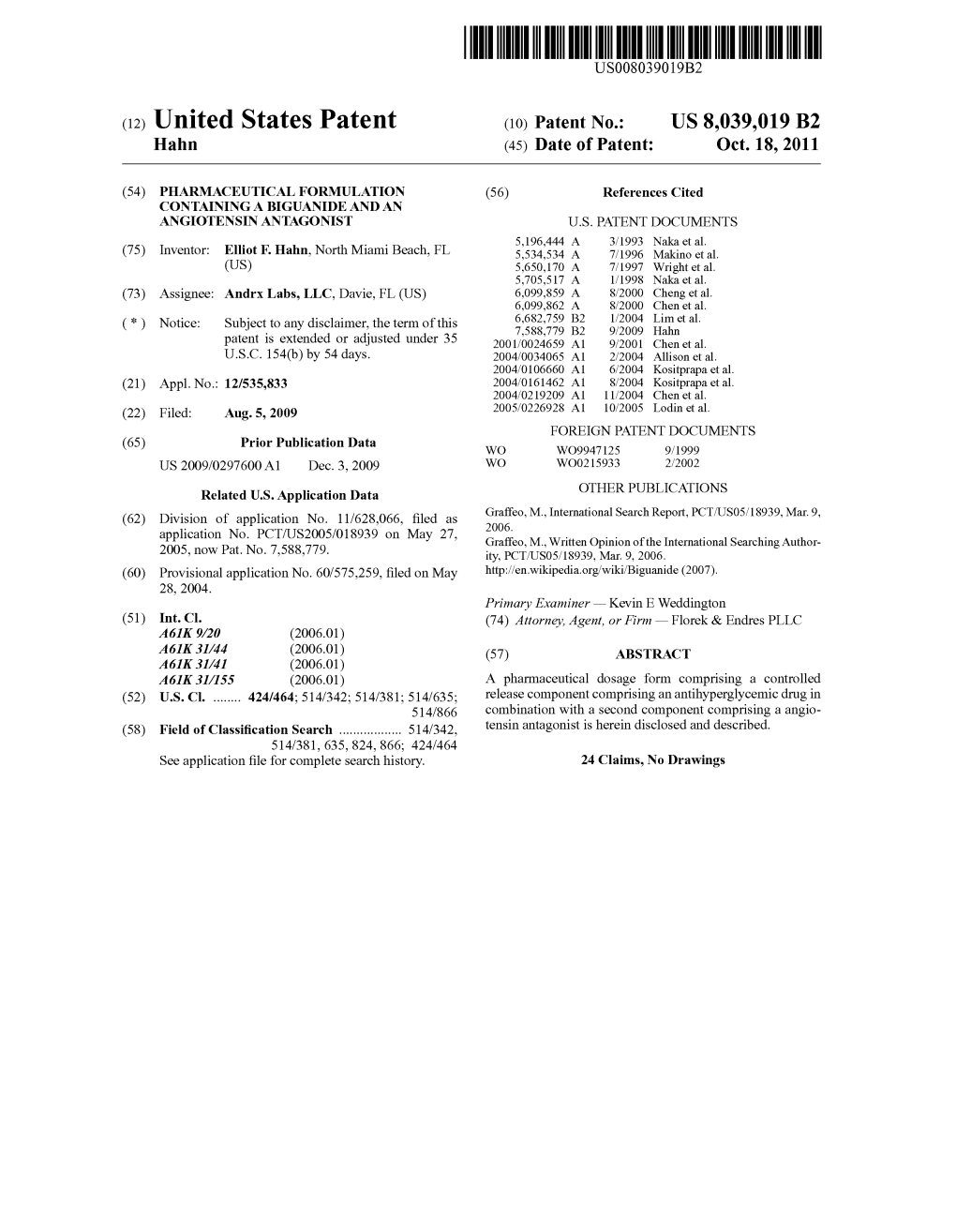
(12) United States Patent (10) Patent No.: US 8,039,019 B2 Hahn (45) Date of Patent: Oct
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Specifications of Approved Drug Compound Library
Annexure-I : Specifications of Approved drug compound library The compounds should be structurally diverse, medicinally active, and cell permeable Compounds should have rich documentation with structure, Target, Activity and IC50 should be known Compounds which are supplied should have been validated by NMR and HPLC to ensure high purity Each compound should be supplied as 10mM solution in DMSO and at least 100µl of each compound should be supplied. Compounds should be supplied in screw capped vial arranged as 96 well plate format. -

Identification of Compounds That Rescue Otic and Myelination
RESEARCH ARTICLE Identification of compounds that rescue otic and myelination defects in the zebrafish adgrg6 (gpr126) mutant Elvira Diamantopoulou1†, Sarah Baxendale1†, Antonio de la Vega de Leo´ n2, Anzar Asad1, Celia J Holdsworth1, Leila Abbas1, Valerie J Gillet2, Giselle R Wiggin3, Tanya T Whitfield1* 1Bateson Centre and Department of Biomedical Science, University of Sheffield, Sheffield, United Kingdom; 2Information School, University of Sheffield, Sheffield, United Kingdom; 3Sosei Heptares, Cambridge, United Kingdom Abstract Adgrg6 (Gpr126) is an adhesion class G protein-coupled receptor with a conserved role in myelination of the peripheral nervous system. In the zebrafish, mutation of adgrg6 also results in defects in the inner ear: otic tissue fails to down-regulate versican gene expression and morphogenesis is disrupted. We have designed a whole-animal screen that tests for rescue of both up- and down-regulated gene expression in mutant embryos, together with analysis of weak and strong alleles. From a screen of 3120 structurally diverse compounds, we have identified 68 that reduce versican b expression in the adgrg6 mutant ear, 41 of which also restore myelin basic protein gene expression in Schwann cells of mutant embryos. Nineteen compounds unable to rescue a strong adgrg6 allele provide candidates for molecules that may interact directly with the Adgrg6 receptor. Our pipeline provides a powerful approach for identifying compounds that modulate GPCR activity, with potential impact for future drug design. DOI: https://doi.org/10.7554/eLife.44889.001 *For correspondence: [email protected] †These authors contributed Introduction equally to this work Adgrg6 (Gpr126) is an adhesion (B2) class G protein-coupled receptor (aGPCR) with conserved roles in myelination of the vertebrate peripheral nervous system (PNS) (reviewed in Langenhan et al., Competing interest: See 2016; Patra et al., 2014). -

A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache
University of South Florida Masthead Logo Scholar Commons School of Information Faculty Publications School of Information 7-2015 A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache Authors: Jeffrey L. Jackson, Elizabeth Cogbill, Rafael Santana-Davila, Christina Eldredge, William Collier, Andrew Gradall, Neha Sehgal, and Jessica Kuester OBJECTIVE: To compare the effectiveness and side effects of migraine prophylactic medications. DESIGN: We performed a network meta-analysis. Data were extracted independently in duplicate and quality was assessed using both the JADAD and Cochrane Risk of Bias instruments. Data were pooled and network meta-analysis performed using random effects models. DATA SOURCES: PUBMED, EMBASE, Cochrane Trial Registry, bibliography of retrieved articles through 18 May 2014. ELIGIBILITY CRITERIA FOR SELECTING STUDIES: We included randomized controlled trials of adults with migraine headaches of at least 4 weeks in duration. RESULTS: Placebo controlled trials included alpha blockers (n = 9), angiotensin converting enzyme inhibitors (n = 3), angiotensin receptor blockers (n = 3), anticonvulsants (n = 32), beta-blockers (n = 39), calcium channel blockers (n = 12), flunarizine (n = 7), serotonin reuptake inhibitors (n = 6), serotonin norepinephrine reuptake inhibitors (n = 1) serotonin agonists (n = 9) and tricyclic antidepressants (n = 11). In addition there were 53 trials comparing different drugs. Drugs with at least 3 trials that were more effective than placebo for episodic migraines -

WO 2013/061161 A2 2 May 2013 (02.05.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/061161 A2 2 May 2013 (02.05.2013) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/337 (2006.01) A61K 31/48 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/395 (2006.01) A61K 31/51 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/4174 (2006.01) A61K 31/549 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, A61K 31/428 (2006.01) A61K 31/663 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (21) International Application Number: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, PCT/IB20 12/002768 ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (22) International Filing Date: NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, 25 October 2012 (25.10.2012) RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (25) Filing Language: English ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/552,922 28 October 201 1 (28. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau Et Al
US 20150202317A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau et al. (43) Pub. Date: Jul. 23, 2015 (54) DIPEPTDE-BASED PRODRUG LINKERS Publication Classification FOR ALPHATIC AMNE-CONTAINING DRUGS (51) Int. Cl. A647/48 (2006.01) (71) Applicant: Ascendis Pharma A/S, Hellerup (DK) A638/26 (2006.01) A6M5/9 (2006.01) (72) Inventors: Harald Rau, Heidelberg (DE); Torben A 6LX3/553 (2006.01) Le?mann, Neustadt an der Weinstrasse (52) U.S. Cl. (DE) CPC ......... A61K 47/48338 (2013.01); A61 K3I/553 (2013.01); A61 K38/26 (2013.01); A61 K (21) Appl. No.: 14/674,928 47/48215 (2013.01); A61M 5/19 (2013.01) (22) Filed: Mar. 31, 2015 (57) ABSTRACT The present invention relates to a prodrug or a pharmaceuti Related U.S. Application Data cally acceptable salt thereof, comprising a drug linker conju (63) Continuation of application No. 13/574,092, filed on gate D-L, wherein D being a biologically active moiety con Oct. 15, 2012, filed as application No. PCT/EP2011/ taining an aliphatic amine group is conjugated to one or more 050821 on Jan. 21, 2011. polymeric carriers via dipeptide-containing linkers L. Such carrier-linked prodrugs achieve drug releases with therapeu (30) Foreign Application Priority Data tically useful half-lives. The invention also relates to pharma ceutical compositions comprising said prodrugs and their use Jan. 22, 2010 (EP) ................................ 10 151564.1 as medicaments. US 2015/0202317 A1 Jul. 23, 2015 DIPEPTDE-BASED PRODRUG LINKERS 0007 Alternatively, the drugs may be conjugated to a car FOR ALPHATIC AMNE-CONTAINING rier through permanent covalent bonds. -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX -

Drug Delivery System for Use in the Treatment Or Diagnosis of Neurological Disorders
(19) TZZ __T (11) EP 2 774 991 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 10.09.2014 Bulletin 2014/37 C12N 15/86 (2006.01) A61K 48/00 (2006.01) (21) Application number: 13001491.3 (22) Date of filing: 22.03.2013 (84) Designated Contracting States: • Manninga, Heiko AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 37073 Göttingen (DE) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO •Götzke,Armin PL PT RO RS SE SI SK SM TR 97070 Würzburg (DE) Designated Extension States: • Glassmann, Alexander BA ME 50999 Köln (DE) (30) Priority: 06.03.2013 PCT/EP2013/000656 (74) Representative: von Renesse, Dorothea et al König-Szynka-Tilmann-von Renesse (71) Applicant: Life Science Inkubator Betriebs GmbH Patentanwälte Partnerschaft mbB & Co. KG Postfach 11 09 46 53175 Bonn (DE) 40509 Düsseldorf (DE) (72) Inventors: • Demina, Victoria 53175 Bonn (DE) (54) Drug delivery system for use in the treatment or diagnosis of neurological disorders (57) The invention relates to VLP derived from poly- ment or diagnosis of a neurological disease, in particular oma virus loaded with a drug (cargo) as a drug delivery multiple sclerosis, Parkinsons’s disease or Alzheimer’s system for transporting said drug into the CNS for treat- disease. EP 2 774 991 A1 Printed by Jouve, 75001 PARIS (FR) EP 2 774 991 A1 Description FIELD OF THE INVENTION 5 [0001] The invention relates to the use of virus like particles (VLP) of the type of human polyoma virus for use as drug delivery system for the treatment or diagnosis of neurological disorders. -

Microwave-Induced in Situ Amorphization
Microwave-Induced In Situ Amorphization A New Strategy for Tackling the Stability Issue of Amorphous Solid Dispersions Qiang, Wei; Lobmann, Korbinian; McCoy, Colin P.; Andrews, Gavin P.; Zhao, Min Published in: Pharmaceutics DOI: 10.3390/pharmaceutics12070655 Publication date: 2020 Document version Publisher's PDF, also known as Version of record Document license: CC BY Citation for published version (APA): Qiang, W., Lobmann, K., McCoy, C. P., Andrews, G. P., & Zhao, M. (2020). Microwave-Induced In Situ Amorphization: A New Strategy for Tackling the Stability Issue of Amorphous Solid Dispersions. Pharmaceutics, 12(7), [655]. https://doi.org/10.3390/pharmaceutics12070655 Download date: 25. sep.. 2021 pharmaceutics Review Microwave-Induced In Situ Amorphization: A New Strategy for Tackling the Stability Issue of Amorphous Solid Dispersions Wei Qiang 1, Korbinian Löbmann 2 , Colin P. McCoy 1 , Gavin P. Andrews 1,3 and Min Zhao 1,3,* 1 School of Pharmacy, Queen’s University Belfast, Belfast BT9 7BL, UK; [email protected] (W.Q.); [email protected] (C.P.M.); [email protected] (G.P.A.) 2 Department of Pharmacy, University of Copenhagen, 2100 Copenhagen, Denmark; [email protected] 3 China Medical University- Queen’s University Belfast Joint College (CQC), China Medical University, Shenyang 110000, China * Correspondence: [email protected]; Tel.: +44-028-9097-2798; +86-024-31939488 Received: 30 May 2020; Accepted: 3 July 2020; Published: 11 July 2020 Abstract: The thermodynamically unstable nature of amorphous drugs has led to a persistent stability issue of amorphous solid dispersions (ASDs). Lately, microwave-induced in situ amorphization has been proposed as a promising solution to this problem, where the originally loaded crystalline drug is in situ amorphized within the final dosage form using a household microwave oven prior to oral administration. -

Quantitative Structure-Interaction Relationship Analysis of 1,4-Dihydropyridine Drugs in Concomitant Administration with Grapefruit Juice
ORIGINAL ARTICLES Clinical Pharmaceutics Laboratory, Department of Pharmaceutics, Meiji Pharmaceutical University, Tokyo, Japan Quantitative structure-interaction relationship analysis of 1,4-dihydropyridine drugs in concomitant administration with grapefruit juice Y. Uesawa, K. Mohri Received July 11, 2011, accepted August 16, 2011 Dr. Yoshihiro Uesawa, Clinical Pharmaceutics Laboratory, Department of Pharmaceutics, Meiji Pharmaceutical University, 2-522-1, Noshio, Kiyose, Tokyo 204-8588, Japan [email protected] Pharmazie 67: 195–201 (2012) doi: 10.1691/ph.2012.1101 Quantitative structure-interaction relationship (QSIR) analyses of 1,4-dihydropyridine drugs were per- formed on grapefruit juice interaction potentials to characterize the interaction and evaluate drugs not yet tested in clinical research. AUC ratios of drugs with and without grapefruit juice ingestion were esti- mated as grapefruit juice interaction potentials from clinical studies on dihydropyridine drugs such as amlodipine, azelnidipine, benidipine, cilnidipine, felodipine, manidipine, nicardipine, nifedipine, nimodip- ine, nisoldipine, and pranidipine. The minimal energy conformation in each dihydropyridine drug was searched for using Merck Molecular Force Field (MMFFaq), and then geometry optimization was performed by density-functional-theory (DFT) calculation (B3LYP/6-31G**). The geometric, electronic, and physico- chemical features including molecular size, dipole moment, total energy, HOMO/LUMO energies, and logP values were then obtained. Dragon descriptors were also calculated by optimized 3D-structures. The rela- tion between the potentials and over 1000 of the molecular properties was investigated using statistical techniques including partial least squares analysis with genetic algorithm (GA-PLS) to a variable subset selection. Some PLS regression equations including logP values and dragon descriptors as explanatory variables were constructed in which the maximal contribution coefficient was 94%. -

Efonidipine Simultaneously Improves Blood Pressure, Endothelial Function, and Metabolic Parameters in Nondiabetic Patients with Hypertension
Emerging Treatments and Technologies BRIEF REPORT Efonidipine Simultaneously Improves Blood Pressure, Endothelial Function, and Metabolic Parameters in Nondiabetic Patients With Hypertension 1 2 KWANG KON KOH, MD JEONG-A KIM, PHD underwent a 3-week washout period. At 2 1 MICHAEL J. QUON, MD, PHD WOOK-JIN CHUNG, MD the end of the washout period, partici- 1 4 SANG JIN LEE, MD YONGHEE LEE, PHD pants were randomly assigned to either 1 1 SEUNG HWAN HAN, MD EAK KYUN SHIN, MD 3 40–80 mg efonidipine or placebo daily JEONG YEAL AHN, MD during 8 weeks. Patients were then crossed over to the second treatment arm on completion of the first treatment arm ypertension is characterized by en- sure (9). Therefore, we hypothesized (without washout phase). The Green dothelial dysfunction and fre- that efonidipine therapy may simulta- Cross Pharmaceutical company (Yongin, H quently clusters with metabolic neously improve endothelial dysfunc- Korea) provided the identical placebo disorders that are characterized by insulin tion, adipocytokine profiles, and other (purchased by investigators). One patient resistance (1,2). These comorbidities may metabolic parameters in nondiabetic suffered from facial flushing and was be explained, in part, by reciprocal rela- patients with hypertension. withdrawn. Thus, data from 38 patients tionships between endothelial dysfunc- were analyzed. This study was approved tion and insulin resistance (1). By contrast RESEARCH DESIGN AND by the Gil Hospital Institute Review with calcium channel blockers (CCBs), METHODS — We evaluated effects of Board. treatment of hypertension with -block- efonidipine in a randomized, double- Blood samples were obtained at ers and diuretics is associated with a blind, placebo-controlled, crossover 8:00 A.M. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

The Pharmaceuticals and Medical Devices Agency Annual Report Fy 2010 Table of Contents
THE PHARMACEUTICALS AND MEDICAL DEVICES AGENCY ANNUAL REPORT FY 2010 TABLE OF CONTENTS Page I. THE PHARMACEUTICALS AND MEDICAL DEVICES AGENCY .................. 1 PART 1 History and Objective of PMDA ........................................................................................................ 2 PART 2 Outline of Operations ........................................................................................................................ 4 2.1 Relief Services for Adverse Health Effects ............................................................................... 4 2.2 Reviews ..................................................................................................................................... 4 2.3 Safety Measures ....................................................................................................................... 5 II. OPERATING PERFORMANCE FOR FY 2010............................................... 7 PART 1 Development of Fiscal Year 2010 Plan ............................................................................................ 8 1.1.Development and Implementation of Fiscal Year 2010 Plan ................................................... 8 1.2.Results of the Evaluation on Operating Performance for FY 2009 .......................................... 8 1.3.Budget Screening by the Government Revitalization Unit ..................................................... 11 PART 2 Improvement in Overall Management of Operations and Service Quality of PMDA ..................... 14 2. 1.Efficient