National Public Health Emergency Team (NPHET) for COVID-19 Governance Structures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

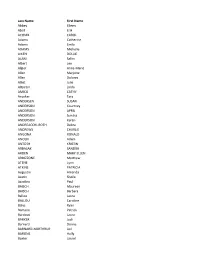
Misdemeanor Warrant List
SO ST. LOUIS COUNTY SHERIFF'S OFFICE Page 1 of 238 ACTIVE WARRANT LIST Misdemeanor Warrants - Current as of: 09/26/2021 9:45:03 PM Name: Abasham, Shueyb Jabal Age: 24 City: Saint Paul State: MN Issued Date Bail Amount Warrant Type Charge Offense Level 10/05/2020 415 Bench Warrant-fail to appear at a hearing TRAFFIC-9000 Misdemeanor Name: Abbett, Ashley Marie Age: 33 City: Duluth State: MN Issued Date Bail Amount Warrant Type Charge Offense Level 03/09/2020 100 Bench Warrant-fail to appear at a hearing False Pretenses/Swindle/Confidence Game Misdemeanor Name: Abbott, Alan Craig Age: 57 City: Edina State: MN Issued Date Bail Amount Warrant Type Charge Offense Level 09/16/2019 500 Bench Warrant-fail to appear at a hearing Disorderly Conduct Misdemeanor Name: Abney, Johnese Age: 65 City: Duluth State: MN Issued Date Bail Amount Warrant Type Charge Offense Level 10/18/2016 100 Bench Warrant-fail to appear at a hearing Shoplifting Misdemeanor Name: Abrahamson, Ty Joseph Age: 48 City: Duluth State: MN Issued Date Bail Amount Warrant Type Charge Offense Level 10/24/2019 100 Bench Warrant-fail to appear at a hearing Trespass of Real Property Misdemeanor Name: Aden, Ahmed Omar Age: 35 City: State: Issued Date Bail Amount Warrant Type Charge Offense Level 06/02/2016 485 Bench Warrant-fail to appear at a hearing TRAFF/ACC (EXC DUI) Misdemeanor Name: Adkins, Kyle Gabriel Age: 53 City: Duluth State: MN Issued Date Bail Amount Warrant Type Charge Offense Level 02/28/2013 100 Bench Warrant-fail to appear at a hearing False Pretenses/Swindle/Confidence Game Misdemeanor Name: Aguilar, Raul, JR Age: 32 City: Couderay State: WI Issued Date Bail Amount Warrant Type Charge Offense Level 02/17/2016 Bench Warrant-fail to appear at a hearing Driving Under the Influence Misdemeanor Name: Ainsworth, Kyle Robert Age: 27 City: Duluth State: MN Issued Date Bail Amount Warrant Type Charge Offense Level 11/22/2019 100 Bench Warrant-fail to appear at a hearing Theft Misdemeanor ST. -

CAREY V. COMMISSIONER of CORRECTION (AC 24655) Schaller, West and Hennessy, Js
****************************************************** The ``officially released'' date that appears near the beginning of each opinion is the date the opinion will be published in the Connecticut Law Journal or the date it was released as a slip opinion. The operative date for the beginning of all time periods for filing postopinion motions and petitions for certification is the ``officially released'' date appearing in the opinion. In no event will any such motions be accepted before the ``officially released'' date. All opinions are subject to modification and technical correction prior to official publication in the Connecti- cut Reports and Connecticut Appellate Reports. In the event of discrepancies between the electronic version of an opinion and the print version appearing in the Connecticut Law Journal and subsequently in the Con- necticut Reports or Connecticut Appellate Reports, the latest print version is to be considered authoritative. The syllabus and procedural history accompanying the opinion as it appears on the Commission on Official Legal Publications Electronic Bulletin Board Service and in the Connecticut Law Journal and bound volumes of official reports are copyrighted by the Secretary of the State, State of Connecticut, and may not be repro- duced and distributed without the express written per- mission of the Commission on Official Legal Publications, Judicial Branch, State of Connecticut. ****************************************************** CHARLES CAREY v. COMMISSIONER OF CORRECTION (AC 24655) Schaller, West and Hennessy, Js. Argued September 17Ðofficially released November 23, 2004 (Appeal from Superior Court, judicial district of New Haven, Hon. Howard F. Zoarski, judge trial referee.) Kirstin B. Coffin, special public defender, for the appellant (petitioner). Margaret Gaffney Radionovas, senior assistant state's attorney, with whom, on the brief, were Christo- pher L. -

Mathew Carey's Douay-Rheims Bible
Mathew Carey’s Douay-Rheims Bible by Nicholas Mario Bruno1 Penniless and exiled, a young printer, disguised as a woman to avoid arrest by the English, sailed to Philadelphia with the Marquis de Lafayette. When the ship arrived in Philadelphia, Lafayette introduced Carey to George Washington and other influential Americans who lent him $400 to set up a printing shop. This young printer, Mathew Carey, would be very influential in early American printing. This paper will examine his life and some of his most influential work both as an American printer, dedicated to creating a nationalistic literary identity, and his work as a Catholic, printing the Mathew Carey Bible during an important era for the Catholic Church in America. Background of Mathew Carey Although known mainly for his work in America, Carey was not born in America; he was born in Dublin, Ireland in 1760. He started his career as a journalist in Ireland. At the age of 19, Carey advocated the repeal of the British Penal Code against Irish Catholics in an anonymous pamphlet. When the British government offered a reward for the author of the pamphlet, Carey fled for France where he met Benjamin Franklin. After a year in France, Carey returned to Ireland but again got into trouble with political authorities – this time for his views on economic policy. Carey, who supported tariffs, published a cartoon of a British official who opposed a tariff bill being hanged for treason. Fortunately for Carey, Franklin had introduced him to the Marquis de Lafayette and arranged for Lafayette to 1 Nicholas Bruno won 1st place in the 2011 “A Piece of the Past” museum essay contest. -

Petitioners, V
No. _________ ================================================================================================================ In The Supreme Court of the United States --------------------------------- --------------------------------- BARRY L. RUPERT, CAROL RUPERT, MICHAEL RISHMAGUE, LIONEL ALESSIO, DAN AULI PANOS, EDNA ABLE, et al., Petitioners, v. RALPH S. JANVEY, in his Capacity as Court-Appointed Receiver for Stanford Receivership Estate, et al., Respondents. --------------------------------- --------------------------------- On Petition For Writ Of Certiorari To The United States Court Of Appeals For The Fifth Circuit --------------------------------- --------------------------------- PETITION FOR WRIT OF CERTIORARI --------------------------------- --------------------------------- RANDALL A. PULMAN MICHAEL J. STANLEY Counsel of Record W. SHAWN STAPLES LESLIE SARA HYMAN STANLEY LAW, P.C. MATTHEW J. MCGOWAN 230 Westcott St, PULMAN, CAPPUCCIO & Ste 120 PULLEN, LLP Houston, Texas 77007 2161 NW Military Hwy, Ste 400 (713) 980-4381 San Antonio, Texas 78213 Counsel for the (210) 222-9494 Able Parties [email protected] Counsel for the Rupert Parties ================================================================================================================ COCKLE LEGAL BRIEFS (800) 225-6964 WWW.COCKLELEGALBRIEFS.COM i QUESTION PRESENTED FOR REVIEW Petitioners were investors who lost their invest- ment in the Stanford International Bank Ponzi scheme. Petitioners brought suit in state court against two brokers that made independent -

Carey CV 2017
JOHN MICHAEL CAREY Curriculum vitae, February 2017 Department of Government Phone: 603 646 1130 Dartmouth College Fax: 603 646 2152 Silsby Hall 6108 Email: [email protected] Hanover, New Hampshire 03755 Website: www.dartmouth.edu/~jcarey EDUCATION University of California, San Diego: Ph.D. in Political Science, 1993. • Dissertation title: Term Limits and Legislative Representation Harvard University: B.A. Magna Cum Laude in Social Studies, June 1986. • Certificate in Latin American studies. EMPLOYMENT Dartmouth College: John Wentworth Professor in the Social Sciences, 2007-present. • Committee Advisory to the President, 2015-present. • Institutional Review Board for Arts & Sciences, 2015-present. • Faculty Athletic Representative to NCAA, 2011-present. • Chair, Department of Government, 2009-2015. • Chair, President’s Advisory Committee on Investor Responsibility (ACIR), 2007-2011. Committee member, 2006-2007. • Arts & Sciences Committee on Priorities, 2009-2012. • Professor of Government, 2005-2007. • Associate Professor of Government, 2003-2005. • Co-director of Undergraduate Honors Program, 2004-2010. • Courses: Introduction to Comparative Politics; Latin American Politics; Elections & Reform; Democracy & Accountability in Latin America. Juan March Institute, Madrid, Spain: Visiting Professor of Political Science, March-May 2006. Harvard University: David Rockefeller Visiting Associate Professor of Government, January- June 2003. Washington University in St. Louis: Associate Professor of Political Science, 2000-2002; Assistant Professor, 1997-2000. • Director of Graduate Studies in political science, 2001-2002. University of Rochester: Assistant Professor of Political Science, 1994-1997. • Director, Undergraduate Honors Program in Political Science, 1996-97. International Summer School in Political Science, Poland: Professor. July-August 1994, 1998. Universidad Católica de Chile, Santiago, Chile: Visiting Professor at the Instituto de Ciencias Políticas. -
Last Name First Name Abbey Eileen Abell Erik ACOMB CAROL Adams
Last Name First Name Abbey Eileen Abell Erik ACOMB CAROL Adams Catherine Adams Emily ADAMS Michelle AIKEN DOLLIE ALANI Salim Albert Lee Algier Anne-Marie Allen Marjorie Allen Dolores Alliet Julie Altpeter Linda AMICO CATHY Anacker Tara ANDERSEN SUSAN ANDERSON Courtney ANDERSON APRIL ANDERSON Sondra ANDERSON Karen ANDREACCHI-ROTH Debra ANDREWS CHARLIE ANGONA RONALD ANOLIK Adam ANTOSH KRISTIN ARBASAK SANDRA ARDEN MARY ELLEN ARDIZZONE Matthew ATENE Lynn ATKINS PATRICIA Augustin Amanda Austin Sheila Azzolino Paul BAISCH Maureen BAISCH Barbara Ballou Laura BALLOU Caroline Balys Ryan Bamann Patrick Bardossi Laura BARKER Jodi Barnard Donna BARNARD-NORTHRUP Lori BARONE Holly Baxter Laurel BEADLE PATRICE BEATO PAT BEAUMONT Patricia BEAUMONT Nicole Beegen Debora BENDSCHNEIDER DEB Bennett Susan BENNETT Cheryl Benson Sharon BERDS Patina Berk Karen Bermudez Berlin BIRD Daisy Bisbo Karen bissinger kathryn BLACK Karen Blackmon Kathleen BLANKENBERG CHRISTOPHER BLOOM PEARL BLOSS Jeffrey BLOSS WILLIAM BLOSSOM Mariellen Bock Elizabeth BODENSTEINER Cheryl Bogdon Melody BOHN Kathleen BONGIOVANNI MARYANNE Bonnell Diane BOONE NICOLE Borrelli Annette Borrelli James Bowdish Tina Bowley Matthew BRIGHTMAN Susan BROGAN Tyler BROOKS Suzanne BROWN Joseph BROWN SHIRLEY BRUTON Eileen BUCUKOVSKI Sandra Buechel Kathy Bullis Keith BUNTING Christine BURDICK Lynn BURGSTROM Sheryl BURKE DEBORAH BURKHART JULIE BURNS CHRISTINE BURNS Shelley Burns CAITLIN BUSACCO ANGELA BUSCEMI Beverly BUSCETTO Kirsten BUTLER Christopher Cain L CALABRO KAREN Caldicott Lisa Caldiero Al Callens -
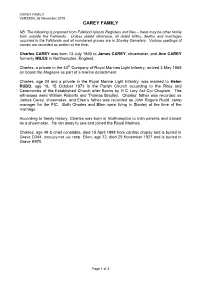
CAREY Charles and Ellen.Pdf
CAREY FAMILY VERSION: 26 November 2010 CAREY FAMILY NB: The following is prepared from Falkland Islands Registers and files – there may be other family born outside the Falklands. Unless stated otherwise, all dated births, deaths and marriages occurred in the Falklands and all numbered graves are in Stanley Cemetery. Various spellings of names are recorded as written at the time. Charles CAREY was born 13 July 1850 to James CAREY, shoemaker, and Ann CAREY formerly MILES in Northampton, England. Charles, a private in the 40th Company of Royal Marines Light Infantry, arrived 3 May 1869 on board the Mageera as part of a marine detachment. Charles, age 24 and a private in the Royal Marine Light Infantry, was married to Helen RUDD, age 18, 15 October 1873 in the Parish Church according to the Rites and Ceremonies of the Established Church after Banns by H C Lory Act Col Chaplain. The witnesses were William Roberts and Thomas Bradley. Charles’ father was recorded as James Carey, shoemaker, and Ellen’s father was recorded as John Rogers Rudd, camp manager for the FIC. Both Charles and Ellen were living in Stanley at the time of the marriage. According to family history, Charles was born in Northampton to Irish parents and trained as a shoemaker. He ran away to sea and joined the Royal Marines. Charles, age 49 & chief constable, died 15 April 1898 from cardiac dropsy and is buried in Grave D344. [Obituary FIM Jun 1898] Ellen, age 72, died 29 November 1927 and is buried in Grave K970. Page 1 of 3 CAREY FAMILY VERSION: 26 November 2010 FIRST GENERATION Children of Charles & Ellen CAREY: 1. -

Cemetery-Burials by Last Name
Cemetery - Burials By Last Name Last Name First Name Middle Maiden Name Section Block Lot Grave Died Age Burial Date AARONS PATRICIA LYNN B 214 D 8/20/2010 AASEN CARL MASONIC 119 2 2 3/2/1983 83 AASEN FLORENCE LUCILLE MASONIC 119 4 2/21/1990 66 2/24/1990 AASEN JUDITH MASONIC 119 3 3 3/7/1977 78 ABBE IVAN ROBERT J 2 8 A 7/2/1953 24 ABBOTT CHARLES A 78A 5 6/4/1912 28 ABBOTT GARY DELBERT NATURES PATHWAY E 19 1/7/2015 70 1/23/2015 ABBOTT KETURAH OLD CEMETERY 368 4/23/1907 0 ABEL MAGDALINE OLD CEMETERY 97 2/13/1905 0 ABERNATHY CLYDE C. A 74A 5 1/16/1957 77 ABERNATHY EDGAR W. I 6 8 D 8/14/1976 68 ABERNATHY IMA I 6 8 E 7/25/1980 72 ACHILLES ALBERT O. D 14 8 A 12/21/1963 0 ACHILLES FRED A 93 4 9/2/1920 71 ACHILLES MARY D 14 8 B 5/22/1965 74 ACHILLES OLGA A 93 5 7/5/1937 84 ACHORN OLIVER OLD CEMETERY 397 2/28/1894 0 ACKER JOHN A 7 4 8/12/1917 34 ACKER JOHN OLD CEMETERY 72 1/26/1901 0 ACKERMAN BERNICE LOIS J 2 8 B 11/12/1988 86 11/16/1988 ADAMS BRANDON J. J 12 1 N 9/14/1974 0 Friday, March 23, 2018 Page 1 of 690 Last Name First Name Middle Maiden Name Section Block Lot Grave Died Age Burial Date ADAMS ELIAS E 1 4 A 11/27/1923 73 ADAMS HARRIET B 227 C 10/22/1958 81 ADAMS INA CHASE B 100 D 8/22/1950 72 ADAMS LLEWELLYN B 100 C 9/14/1936 63 ADAMS MIRIAM REEL L 3 15 A 11/4/2014 95 11/13/2014 ADAMS NELLIE OR MILLIE 1ST ADDITION 182 5 9/13/1913 0 ADAMS PAMELA J. -
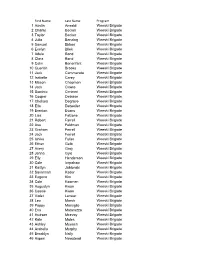
First Name Last Name Program 1 Austin Ansaldi Weeski Brigade 2
First Name Last Name Program 1 Austin Ansaldi Weeski Brigade 2 Charlie Becker Weeski Brigade 3 Taylor Becker Weeski Brigade 4 Julia Benzing Weeski Brigade 5 Samuel Birken Weeski Brigade 6 Evelyn Bliek Weeski Brigade 7 Adele Bond Weeski Brigade 8 Clara Bond Weeski Brigade 9 Colin Bonenfant Weeski Brigade 10 Quentin Brooks Weeski Brigade 11 Jack Cammarata Weeski Brigade 12 Isabelle Carey Weeski Brigade 13 Mason Chapman Weeski Brigade 14 Jack Cicero Weeski Brigade 15 Dominic Cimineri Weeski Brigade 16 Cooper Deblase Weeski Brigade 17 Chelsea Degrave Weeski Brigade 18 Ella Detweiler Weeski Brigade 19 Brenton Evans Weeski Brigade 20 Lisa Falzone Weeski Brigade 21 Robert Farrell Weeski Brigade 22 Asa Feldman Weeski Brigade 23 Graham Ferrell Weeski Brigade 24 Jack Ferrell Weeski Brigade 25 Ishika Fuller Weeski Brigade 26 Ethan Gelb Weeski Brigade 27 Avery Gray Weeski Brigade 28 Jenna Gyle Weeski Brigade 29 Elly Henderson Weeski Brigade 30 Cole Ingraham Weeski Brigade 31 Kaitlyn Jablonski Weeski Brigade 32 Savannah Kader Weeski Brigade 33 Eugene Kim Weeski Brigade 34 Cole Koomen Weeski Brigade 35 Augustyn Kwon Weeski Brigade 36 Cassie Kwon Weeski Brigade 37 Violet Lenear Weeski Brigade 38 Leo Marsh Weeski Brigade 39 Poppy Marsiglio Weeski Brigade 40 Eva Matarazzo Weeski Brigade 41 Hudson Mcevoy Weeski Brigade 42 Kate Moles Weeski Brigade 43 Ashley Muench Weeski Brigade 44 Arabella Murphy Weeski Brigade 45 Brooklyn Nally Weeski Brigade 46 Aspen Newstead Weeski Brigade 47 Campbell Nicholson Weeski Brigade 48 Emily Orlando Weeski Brigade 49 Emily -

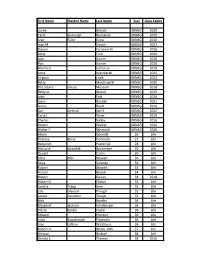
2017 Purge List LAST NAME FIRST NAME MIDDLE NAME SUFFIX
2017 Purge List LAST NAME FIRST NAME MIDDLE NAME SUFFIX AARON LINDA R AARON-BRASS LORENE K AARSETH CHEYENNE M ABALOS KEN JOHN ABBOTT JOELLE N ABBOTT JUNE P ABEITA RONALD L ABERCROMBIA LORETTA G ABERLE AMANDA KAY ABERNETHY MICHAEL ROBERT ABEYTA APRIL L ABEYTA ISAAC J ABEYTA JONATHAN D ABEYTA LITA M ABLEMAN MYRA K ABOULNASR ABDELRAHMAN MH ABRAHAM YOSEF WESLEY ABRIL MARIA S ABUSAED AMBER L ACEVEDO MARIA D ACEVEDO NICOLE YNES ACEVEDO-RODRIGUEZ RAMON ACEVES GUILLERMO M ACEVES LUIS CARLOS ACEVES MONICA ACHEN JAY B ACHILLES CYNTHIA ANN ACKER CAMILLE ACKER PATRICIA A ACOSTA ALFREDO ACOSTA AMANDA D ACOSTA CLAUDIA I ACOSTA CONCEPCION 2/23/2017 1 of 271 2017 Purge List ACOSTA CYNTHIA E ACOSTA GREG AARON ACOSTA JOSE J ACOSTA LINDA C ACOSTA MARIA D ACOSTA PRISCILLA ROSAS ACOSTA RAMON ACOSTA REBECCA ACOSTA STEPHANIE GUADALUPE ACOSTA VALERIE VALDEZ ACOSTA WHITNEY RENAE ACQUAH-FRANKLIN SHAWKEY E ACUNA ANTONIO ADAME ENRIQUE ADAME MARTHA I ADAMS ANTHONY J ADAMS BENJAMIN H ADAMS BENJAMIN S ADAMS BRADLEY W ADAMS BRIAN T ADAMS DEMETRICE NICOLE ADAMS DONNA R ADAMS JOHN O ADAMS LEE H ADAMS PONTUS JOEL ADAMS STEPHANIE JO ADAMS VALORI ELIZABETH ADAMSKI DONALD J ADDARI SANDRA ADEE LAUREN SUN ADKINS NICHOLA ANTIONETTE ADKINS OSCAR ALBERTO ADOLPHO BERENICE ADOLPHO QUINLINN K 2/23/2017 2 of 271 2017 Purge List AGBULOS ERIC PINILI AGBULOS TITUS PINILI AGNEW HENRY E AGUAYO RITA AGUILAR CRYSTAL ASHLEY AGUILAR DAVID AGUILAR AGUILAR MARIA LAURA AGUILAR MICHAEL R AGUILAR RAELENE D AGUILAR ROSANNE DENE AGUILAR RUBEN F AGUILERA ALEJANDRA D AGUILERA FAUSTINO H AGUILERA GABRIEL -
First Name Maiden Name Last Name Year Dues Expire Lynne Bobula
First Name Maiden Name Last Name Year Dues Expire Lynne Bobula 00NBG 2020 Carol Szunyogh Buchanan 00NBG 2020 Jean Fuller Crow 00NBG 2016 Joan M. Deuch 00NBG 2022 Steven Farnsworth 00NBG 2016 Betty Ford 00NBG 2020 Joan Ganim 00NBG 2018 Ron Ganim 00NBG 2018 Martin G. Johnston 00NBG 2019 Anne Kaczmarek 00NBG 2025 Virginia Little 00NBG 2022 Betty Mantkowski 00NBG 2020 The Squire House Museum 00NBG 2018 Betty Jo Niccoli 00NBG 2019 John Pajk 00NBG 2016 Jayne Randall 00NBG 2021 James Roytz 00NBG 2016 Sue Zielinski Schill 00NBG 2022 Carol J. Tener 00NBG 2019 Charles Valley 00NBG 2016 Robert Walker 00NBG 2016 Walter F. Wisnieski 00NBG 2026 Edwin Schmidt 26 Life Theresa Borys Dominick 27 Life Benjamin Pasternak 28 Life Marjorie Kowallek Bruemmer 30 Life Donald Curtis 30 Life Edna Pfeil Stewart 30 Life Anna Valvoda 30 Life Robert Stewart 33 Life Harold Bejcek 34 Life Robert Gaines 34 2018 Robert G. Ehrbar 35 Life Loretta Trapp Kern 35 Life Lois Gleeson Prough 35 Life Louise Davidson Thayer 35 Life Nick Bondra 36 Life Margaret Jackson Echelberger 36 Life Vlasta Kouba Foster 36 Life Edward Hienton 36 Life Luba Kwatkowich Pisanecki 36 Life Jean Laftery Washburn 36 Life Robert V. Webb, DDS 37 Life Weston Birdsall 38 Life Donald L. Thomas 38 2016 First Name Maiden Name Last Name Year Dues Expire Walter G. Broz 39 Life Virginia Klein Gerseny* 39 Life Jack Harper 39 Life George R. Slater 39 Life Ed Spatz 40NBG Life Jean Thomas Vaughan 40 Life Clayton Baum 41 2018 Ruth Kemp DeHaven 41 2017 Doris M. -

VSB Dean's List for Spring 2015.Pdf
Villanova School of Business Announces Dean's List Recipients First Name Last Name City State Maggie Carey Birmingham AL Bailey Nash Huntsville AL Kenyn Cheatham Scottsdale AZ Gregory Cox Alamo CA Robert McAlister Arcadia CA Kevin Bitar Coronado CA Theodore Wilm Danville CA Timothy Scatterday Danville CA Marc Leprince Fremont CA Kishan Chhatwal Granada Hills CA Alberto Solana Hayward CA Megan McKown Irvine CA Joshua Wharry La Mesa CA Stephen Wemple Lafayette CA Ian Simpson Laguna Hills CA Alexis Mastrocola Laguna Niguel CA Quinn Goonan Laguna Niguel CA Malvika Mecker Los Altos Hills CA Caitlin Drake Los Angeles CA Brendan Austin Mill Valley CA Matthew Reshke Moraga CA Domenic Re Newport Beach CA Michael Lamb Pacific Palisades CA Rory Caulfield Palos Verdes Estates CA Kyle Wilkinson Palos Verdes Estates CA Edward Repko Rancho Santa Fe CA Kyle Beddow San Diego CA Kendall Reardon San Diego CA Michael Rees San Jose CA Kyle Sandvick San Jose CA Jennifer Mauser San Marino CA Nicholas Carney Santa Barbara CA Lena Christianian Boulder CO Jaeyeon Seo Broomfield CO Emily Mayo Centennial CO Sydney Harris Colorado Spgs CO Shayla Frederick Highlands Ranch CO David Smith Avon CT Brittany Nemphos Berlin CT Jeffrey Stevens Cheshire CT Samuel McIntire Darien CT Christopher Brophy Darien CT Jack Ford Fairfield CT Abigail O'Hara Fairfield CT Anthony Miller Farmington CT Caroline Marzo Granby CT Peter Xuan Greenwich CT Claire D'Arcangelo Greenwich CT Mary Dunn Greenwich CT Ryan Melino Madison CT Katherine Mazzeo Madison CT Carolyn Rowan Manchester CT Megan