WHO Surgical Site Infection Prevention Guidelines Web Appendix 7 Summary of a Systematic Review on the Effectiveness and Optimal Method of Hair Removal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Neurosurgery Without Hair Removal and Shampoo Care
& The ics ra tr pe a u i t i d c e s P Pediatrics & Therapeutics Simona et al., Pediatr Ther 2016, 6:2 ISSN: 2161-0665 DOI: 10.4172/2161-0665.1000282 Research Article Open Access Cranial Neurosurgery without Hair Removal and Shampoo Care: Retrospective Analysis of 450 Cases Vergna Simona1, Pinotti Sara1, Festini Filippo1, Spacca Barbara2, Peri Giacomo2 and Genitori Lorenzo2* 1Department of Health Sciences, University of Florence, Italy 2Department of Pediatric Neurosurgery, Anna Meyer Children's Hospital, Italy *Corresponding author: Lorenzo Genitori, Department of Pediatric Neurosurgery, Anna Meyer Children's Hospital, “Anna Meyer” Children’s Hospital, Viale Pieraccini, 24, 50139, Florence, Italy, Tel: 39 (0) 55 5662 934; Fax: 39 (0) 55 5662 396; E-mail: [email protected] Rec date: Mar 02, 2016, Acc date: Mar 24, 2016, Pub date: Mar 28, 2016 Copyright: © 2016 Simona V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited. Abstract Goal: To assess infection rate in a population of children who underwent cranial neurosurgery without hair removal. Methods: Retrospective analysis of clinical records of children undergoing cranial neurosurgery with “shampoo care” during one year. Results: 450 children were included. 5.55% of them had a wound complication, with only two cases of infection (0.4%). Available literature was revised to assess the effectiveness of our protocol. Wound complication and infections rates found in our experience were lower than those reported in patients treated with a standard trichotomy. -

Shaving and Shavers - Part 2 Ou Israel Center - Summer 2018
5778 - dbhbn ovrct [email protected] 1 sxc HALACHIC AND HASHKAFIC ISSUES IN CONTEMPORARY SOCIETY 101 - SHAVING AND SHAVERS - PART 2 OU ISRAEL CENTER - SUMMER 2018 In Part 1 we saw that the Torah prohibits men from shaving their beard with a razor. In this shiur we need to apply the principles that we learned in Part 1 to the electric shaver and understand the contemporary psak. A] THE HISTORY OF THE ELECTRIC SHAVER • 1879 - invention of the manual beard-clipping machine, mentioned by poskim at the end of the 19C. • 1898 - patents first filed for an electric razor. • 1903 - invention of the safety razor by Gillette in the US. This was marketed in Europe from 1905. • 1925 - invention of the electric safety razor and the vibro-shave. • 1931 - Jacob Schick created the first electric shaver. This was already referenced in the US poskim by 1932.1 • 1939 - Phillips began to produce the shaver with a round head. 2 • 1980s - Invention of the ‘Lift & Cut’ electric shaver. B] THE HALACHIC BACKGROUND We must briefly review the halachic framework for the mitzvah that we saw in Part 1. :Wbe z ,¬ t P ,t ,h ºj J , t´«k u o·f Jt«r , t P Up ºE , t´«k 1. zf:yh trehu In Parashat Kedoshim the Torah explicitly prohibits ‘destroying’ the corners of the beard. It does NOT specifically refer to a razor blade. , yrG U y r Gh t¬«k o ºrG c¸cU Uj·Kdh t«k obez ,tpU o ºJt«r C Æv j re U ³j r eh&t«k (v) 2. -

NIC Electrology Written Examination
NATIONAL ELECTROLOGY THEORY EXAMINATION CANDIDATE INFORMATION BULLETIN (CIB) EXAMINATION CONTENT AND IMPORTANT INSTRUCTIONS Please visit your examination provider’s website for the most current bulletin prior to testing. The National Electrology Theory Examination is the national licensure examination for Electrologists, which is developed and administered by the National-Interstate Council of State Boards of Cosmetology (NIC). This bulletin contains IMPORTANT INFORMATION regarding the examination, including content outline covered by the theory examination, sample questions and answers, and references. The time allowed for the Electrology Theory Examination is 90 minutes. PLEASE REVIEW ALL INFORMATION CAREFULLY. For each NIC National Theory Examination, there are TWO (2) parts to every Candidate Information Bulletin (CIB) stored as separate documents: • Examination Content and Important Instructions – This provides information about the scope of content covered in the Theory examination and information and guidelines related to administration of the Theory examination. • References – This provides a list of references used to develop and support the content covered in the examination. The references are always the same for the Theory and Practical examinations. BE CERTAIN TO DOWNLOAD AND/OR PRINT AND REVIEW BOTH DOCUMENTS THAT MAKE UP THE NIC EXAMINATION CIB. PLEASE REVIEW ALL INFORMATION CAREFULLY! IMPORTANT INSTRUCTIONS Do not leave the examination area without permission. Permission must be obtained to leave the examination area for any reason, including restroom usage or at the completion of the examination. Picture ID is required for re-entry into the examination. With the exception of verbal instructions, the proctors and examination administration personnel are not allowed to communicate with candidates. If you have an emergency situation please notify the proctor. -

Comparative Study of Shaving and Depilatory Cream for Hair Removal in Inguinal Hernia Surgical Site Preparation
RESEARCH PAPER Medical Science Volume : 6 | Issue : 2 | FEBRUARY 2016 | ISSN - 2249-555X Comparative Study of Shaving and Depilatory Cream for Hair Removal in Inguinal Hernia Surgical Site Preparation KEYWORDS depilatory cream; shaving; surgical site infection Dr Manish Bansal Gp capt G S Sethi Department of Surgery, Command Hospital (WC), Department of Surgery, Command Hospital (WC), Chandimandir, Panchkula, Haryana, India Chandimandir, Panchkula, Haryana, India ABSTRACT Introduction: Hair interferes with exposure of incision, suturing and wound dressings. Hair removal is thought to reduce the risk of surgical site infections. Three methods of hair removal are used: shaving, clipping and chemical depilation. Aims and objectives: This study aimed to evaluate shaving and depilatory cream for hair removal in inguinal hernia sur- gical site preparation and to compare incidence of surgical site infection, safety, time needed and cost of hair removal. Material and methods: The study was a prospective & comparative study carried out on 100 patients undergoing in- guinal hernia surgical repair at Command Hospital (WC), Chandimandir. Patients were randomized into two groups, i.e., razor shaving group and depilatory cream group. Results: 9 patients (9%) had surgical site infection including 1(2%) in depilatory cream group and 8(16%) in razor group. Infection was significantly associated with razor than depilatory cream. INTRODUCTION There has been no consistent agreement between recom- Postoperative wound infection may lead to significant mendations -

(BBL™) / LASER HAIR REMOVAL Pre- and Post-Care Instructions
Broad Band Light (BBL™) / LASER HAIR REMOVAL Pre- and Post-Care Instructions Please read the following carefully, as this information will prepare you for BBL / Laser Hair Removal, what to expect, and how to care for the treated area. PRE - LASER INSTRUCTIONS 1. Shave the site/s to be treated the evening before each treatment session. (Avoid waxing for 2 weeks before and throughout treatment course – as waxing diminishes laser target.) 2. Also, minimize sun exposure, as best as possible, for at least 1 month before and after treatment. Wear protective clothing (hat, etc.) and a high SPF (at least SPF 30) sunblock to protect the treated area/s from direct sun exposure. 3. Also, do not use aspirin, aspirin containing medications or alcohol for at least 1 week before and for the first 2 days after treatment. Take Tylenol or another pain reliever which contains no aspirin or ibuprofen, if needed. 4. Apply EMLA / ELA-Max / Topicaine (or other topical anesthetic) at least 1 hour before treatment under saran wrap, if needed. WHAT TO EXPECT ♦ BBL/Laser-treated hairs will still be visible / present after your treatment. However, they are now injured or destroyed at the level of the hair follicle (“root”) and will soon fall out (usually, within the next 2-5 days up to 2 weeks). ♦ The treated area may redden and/or swell somewhat. A mild sunburn sensation may be noticed for up to several hours after treatment. This is caused by the BBL/laser energy, and represents inflammation, and not infection. It is normal and expected part of healing process. -

Policy 312 PROFESSIONAL APPEARANCE STANDARDS Page 2 of 4
Policy 312 Subject PROFESSIONAL APPEARANCE STANDARDS Date Published Page 26 August 2017 1 of 4 By Order of the Police Commissioner POLICY 1. Personal Discipline, Public Confidence and Respect. These Professional Appearance Standards are established to encourage public confidence and respect, to instill a degree of personal discipline among members, to facilitate easy recognition of officers in the field, and to promote officer safety and performance. 2. Applicable to All Sworn Members. The following guidelines establish the Baltimore Police Department’s (BPD) Professional Appearance Standards and shall apply to both male and female members, unless otherwise specified. These regulations apply to all sworn personnel working in a uniformed capacity (to include uniformed overtime and uniformed secondary employment) and to all sworn personnel in court attire. GENERAL 1. Unless otherwise authorized, all on-duty sworn personnel shall appear neat, clean and well−groomed and shall project an image of authority, safety and professionalism to the public at all times. 2. All members are required to familiarize themselves with these standards and to remain in strict compliance at all times. Supervisor/Shift Commander 1. Inspect subordinates daily to ensure compliance with the Professional Appearance Standards established in this policy. 2. Take corrective action, when needed. Universal Hairstyle Requirements 1. Hair must be neatly groomed and conform to the shape of the head. 2. Only natural hair colors are permitted. Hair colors that are considered extreme, faddish or artificial, such as purple, pink or green are prohibited. 3. The bulk of the hair will not be excessive or present a ragged or unkempt appearance, and shall not: 3.1. -

Pharmaceutical Sciences Cosmetics HAIR REMOVAL PRODUCTS
Development Team Principal Investigator Prof. Farhan J Ahmad Jamia Hamdard, New Delhi Dr. Vijaya Khader Former Dean, Acharya N G Ranga Agricultural University Dr. Javed Ali Paper Coordinator Jamia Hamdard, New Delhi Content Writer Mohammad Kashif Iqubal Jamia Hamdard, New Delhi Content Reviewer Dr. Mohd. Aqil Jamia Hamdard, New Delhi Pharmaceutical Cosmetics Sciences HAIR REMOVAL PRODUCTS 0 HAIR REMOVAL PRODUCTS 2017 CONTENTS Introduction Methods for removing hair Required qualities and characteristics of hair styling products Types of hair removal products with typical ingredients Formulations Effects of hair removal products on the skin and hair After depilation/ epilation preparations Packaging of hair removal products Evaluation of hair removal products Marketed hair removal products Pharmaceutical Cosmetics Sciences HAIR REMOVAL PRODUCTS 0 HAIR REMOVAL PRODUCTS 2017 HAIR REMOVAL PRODUCTS 1. INTRODUCTION Hair removal is an increasingly important sector of the cosmetic and personal care industry. Both men and women are becoming more concerned about the aesthetic aspect of their appearance. Human beings choose to remove unwanted body hair for acosmetic, social, cultural, or medical reason.A number of hair removal techniques have been developed over the years, including methods for temporary and permanent hair removal. The availability of the current methods and products may be different; most of them can be used at home; however, there are some that can be used only in professional salons and dermatological offices. 2. METHODS FOR REMOVING HAIR Now a day, there are a number of hair removal techniques and products available. Temporary methods provide hairless skin for a shorter (1–3 days) or a longer time (1–3 weeks), depending on the technique and the individual’s physiological characteristics. -

Wigmaker and Barber by Sharon Fabian
Name Date Wigmaker and Barber By Sharon Fabian Cosmetology is a popular vocational subject in high school. In cosmetology class, students learn to wash and cut hair. They learn to give perms and to color hair too. They learn how to do a fancy hairstyle for a special occasion like a prom. They might learn to cut and style wigs as well as real hair. Cosmetology students often go on to work as hairdressers, styling hair for customers. In colonial times, there were also people who worked as hairdressers. Some people are surprised to learn that, because we often think of the colonists as hard working people who didn't have time for frivolous things like a fancy hairdo. However, there were many people in colonial America who were very fashion conscious and who kept up with the latest styles in both clothing and hairstyles. This was especially true in the larger cities like Williamsburg, Virginia. A city like Williamsburg had shops that catered to the fashion conscious. Wigmakers and barbers there both provided hairdressing services. A barber might provide shaves and haircuts in addition to his other duties, such as performing surgery and pulling teeth! A wigmaker, of course, made wigs, and in the 1700s, wigs were the latest fashion! The fashion of wearing wigs began with the royalty in France; it spread to England and then to America. In colonial times, the gentlemen, not the ladies, wore wigs. Colonial gentlemen also wore queues. A queue was like a ponytail wig that was tied on at the back of the head. -

Barbershop Quartet Sc They Wear Even Politicians and Bureaucrats Are Serious About Their Hair: Nearly a Dozen It Well Federal Entities Have On-Site Barbers
Great HAIR OM SC EW N THEY WEAR EvenBarbershop politicians and bureaucrats are serious aboutQuartet their hair: Nearly a dozen IT WELL RIPPLAAR/SIPA/ federal entities have on-site barbers. Here’s a look at four. T Sure, Abraham Lincoln and Teddy Roosevelt By Kate Parham TOFFER sported distinguished facial hair, but modern S RI K Washington men seem more comfortable with a Y B close shave—though there are exceptions. OLDER We asked Mike Gilman, cofounder of the House of Central H OM; Grooming Lounge, and Aaron Perlut, chairman of ➻ Representatives ➻ Intelligence SC EW the American Mustache Institute, to tell us who Agency N around town has winning facial hair. Barber: Joe Quattrone, formerly LLAN/ U a farmer in Italy, heads the House’s M Barber: Daivon Davis is not only c By Christine Ianzito M privatized barbershop. His is one of K the first African-American to own C the best jobs, he says, “because you the CIA’s barbershop but the first to ATRI P come in contact every day with the cut hair in the shop, which opened people who control the world.” LDING/ Ted Leonsis Jayson Werth in 1955. Now 24, he got the gig at age U 18, then bought the shop in 2010. ENTREPRENEUR NATIONALS OUTFIELDER Inside look: He has trimmed ev- Y CLINT SPA eryone from Prime Minister Giulio Inside look: Davis’s chair has seen B ER Andreotti of Italy—who insisted on the likes of General Michael Hayden Z having his picture taken with Quat- and former CIA director Leon I; BLIT ZZ trone—to Dick Cheney, Al Gore, and I Panetta. -
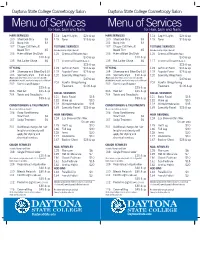
Menu of Services
Daytona State College Cosmetology Salon Daytona State College Cosmetology Salon Menu of Services Menu of Services for Hair, Skin and Nails for Hair, Skin and Nails HAIR SERVICES 114 Cap Hi-Lights $25 & up HAIR SERVICES 114 Cap Hi-Lights $25 & up 100 Shampoo Only $3 115 Toner $15 & up 100 Shampoo Only $3 115 Toner $15 & up 101 Bang Trim $3 _______________________________ 101 Bang Trim $3 _______________________________ 102 Clipper Cut/Haircut/ TEXTURE SERVICES 102 Clipper Cut/Haircut/ TEXTURE SERVICES Beard Trim $5 (Includes Shampoo/Style & Haircut) Beard Trim $5 (Includes Shampoo/Style & Haircut) 103 Haircut/Blow-Dry/Style 116 Chemical Relaxer (Virgin) 103 Haircut/Blow-Dry/Style 116 Chemical Relaxer (Virgin) $10 & up $30 & up $10 & up $30 & up 135 Hot Lather Shave $6 117 Chemical Relaxer (Retouch) 135 Hot Lather Shave $6 117 Chemical Relaxer (Retouch) _______________________________ $25 & up _______________________________ $25 & up STYLING 118 Soft Curl Perm $35 & up STYLING 118 Soft Curl Perm $35 & up 104 Shampoo and Blow-Dry $10 119 Regular Perm $25 & up 104 Shampoo and Blow-Dry $10 119 Regular Perm $25 & up 105 Specialty Style $10 & up 120 Specialty Wrap Perm 105 Specialty Style $10 & up 120 Specialty Wrap Perm (May include; wrap, twists, press & curl, wet sets with (May include; wrap, twists, press & curl, wet sets with $40 & up $40 & up detailed finish, up-do’s, spiral curls, freeze curls or flat-iron) detailed finish, up-do’s, spiral curls, freeze curls or flat-iron) 203 Keratin Straightening 203 Keratin Straightening 202 Dominican -

ELSEVIER Mosby's Textbook for Long-Term Care Nursing Assistants, 6'H Edit 446 Chapter 21 I Grooming
. - .._ _---_.__._._------_ ......• Chapter 21 I Grooming 4 61. A resident with dementia is having problems dressing. 64. A person has an IV. When putting on the clean gown, YOl Which measure will not help? first put it A. Let the person dress himself or herself to the extent A. On the arm with the IV possible. B. On the ann without the IV B. Let the person choose what to wear from 2 or 3 outfits. C. Over the person's head C. Stack clothes in the order that they will be put on. D. So that the ties are in the front D. Complete the process as quickly as possible. 65. A resident has an IV in his right arm. He wears a standarc 62. A person has an IV. When changing the person's gown, you gown and has an IV pump. Which is correct? first A. Put his gown on the right arm first and then on the left ar A. Remove the gown from the arm with no IV B. Put his gown on the left ann first and then on the right ar B. Remove the gown from the arm with the IV C. His right arm is not put through the sleeve of the gown. C. Remove the IV D. TIle gown is put on so that the ties are in the front. D. Ask the person what he or she wants to wear 63. When changing the gown of a person with an IV, you keep the IV bag A. -

Barber Shops Full Page
July/Aug 2012 Edition The Fayetteville Press Page 5b Community Barber Shops Flat Top Haircut Barbershop 360 Waves Brushing Techniques It is easy to achieve a flattop haircut, barbershop style As a guy who wants a perfect waved up hairstyle right from home. People are generally more familiar with you may want to consider 360 waves brushing tech- the flattops cousin hairstyle, the crew cut. The flattop is niques. To get those waves to spinning there is a certain similar to the crew cut in many ways, the difference is that way you need to handle your brush when stroking your with a flattop hairstyle the hair on the tops of the head is thirsty roots. A grooming plan that involves a strategic made to stand up, and is then cut in a flat style. This is what regiment of brushing is imperative to get your hair fol- gives this hairstyle is square shape. licles spinning. Some guys figure it out on there own but You would commonly find this hairstyle on boys. Girls others prefer a training guide. do sometimes wear this hairstyle or different variations or Are there tricks and trade secrets to getting these it, but this is uncommon. The flattop is a popular military style haircut because it is similar to the military crew cut. deep waves? Well yes and no. To get the effective and People commonly created this hairstyle with electric desired results you seek follow the instructions below clippers, which cut the sides and back of the hair. Using the provided by Wave Builder which includes their mainte- clippers, a stylist will cut the hair very close to the scalp; it nance preferences.