A New Paradigm for Understanding Intrinsic Foot Muscle Function
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plantar Fascia-Specific Stretching Program for Plantar Fasciitis
Plantar Fascia-Specific Stretching Program For Plantar Fasciitis Plantar Fascia Stretching Exercise 1. Cross your affected leg over your other leg. 2. Using the hand on your affected side, take hold of your affected foot and pull your toes back towards shin. This creates tension/stretch in the arch of the foot/plantar fascia. 3. Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string. 4. Hold the stretch for a count of 10. A set is 10 repetitions. 5. Perform at least 3 sets of stretches per day. You cannot perform the stretch too often. The most important times to stretch are before taking the first step in the morning and before standing after a period of prolonged sitting. Plantar Fascia Stretching Exercise 1 2 3 4 URMC Orthopaedics º 4901 Lac de Ville Boulevard º Building D º Rochester, NY 14618 º 585-275-5321 www.ortho.urmc.edu Over, Please Anti-inflammatory Medicine Anti-inflammatory medicine will help decrease the inflammation in the arch and heel of your foot. These include: Advil®, Motrin®, Ibuprofen, and Aleve®. 1. Use the medication as directed on the package. If you tolerate it well, take it daily for 2 weeks then discontinue for 1 week. If symptoms worsen or return, then resume medicine for 2 weeks, then stop. 2. You should eat when taking these medications, as they can be hard on your stomach. Arch Support 1. -
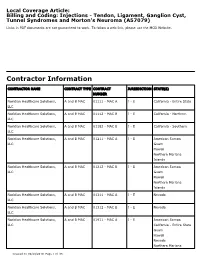
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Advice and Exercises for Patients with Plantar Fasciitis
Advice and exercises for patients with plantar fasciitis This leaflet provides management advice and exercises for people diagnosed with plantar fasciitis, a condition causing pain in the heel, sole and /or arch of the foot. Structures of the foot The plantar fascia is a sheet or broad band of fibrous tissue that runs along the bottom of the foot. This tissue connects the heel to the base of the toes. Under normal circumstances, the plantar fascia supports the arch of the foot and acts as a shock absorbing “bow string” within the arch of the foot. With weight bearing, the foot flattens and the plantar fascia stretches, then springing you forward ready for the next step. While walking, the stresses placed on the foot can be one and a quarter times your body weight (this increases to two and three quarter times your body weight when running). Unsurprisingly then, that heel pain is common. If tension on this “bowstring” becomes too great, irritation or inflammation can occur causing pain. What is plantar fasciitis? Plantar fasciitis is a relatively common foot problem affecting up to 10-15% of the population. It can occur at any age. It is sometimes known as “policeman’s heel”. When placed under too much stress due to abnormal loading, the plantar fascia stretches causing micro tearing and degeneration of the tissue. It can lead to pain in the heel, across the sole of the foot and sometimes into the arch area of the foot too. These micro tears repair with scar tissue, which is less flexible than the fascia and can cause the problem to persist for many months. -

Lower Extremity Focal Neuropathies
LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Arturo A. Leis, MD S.H. Subramony, MD Vettaikorumakankav Vedanarayanan, MD, MBBS Mark A. Ross, MD AANEM 59th Annual Meeting Orlando, Florida Copyright © September 2012 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson Printing Company, Inc. 1 Please be aware that some of the medical devices or pharmaceuticals discussed in this handout may not be cleared by the FDA or cleared by the FDA for the specific use described by the authors and are “off-label” (i.e., a use not described on the product’s label). “Off-label” devices or pharmaceuticals may be used if, in the judgment of the treating physician, such use is medically indicated to treat a patient’s condition. Information regarding the FDA clearance status of a particular device or pharmaceutical may be obtained by reading the product’s package labeling, by contacting a sales representative or legal counsel of the manufacturer of the device or pharmaceutical, or by contacting the FDA at 1-800-638-2041. 2 LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Table of Contents Course Committees & Course Objectives 4 Faculty 5 Basic and Special Nerve Conduction Studies of the Lower Limbs 7 Arturo A. Leis, MD Common Peroneal Neuropathy and Foot Drop 19 S.H. Subramony, MD Mononeuropathies Affecting Tibial Nerve and its Branches 23 Vettaikorumakankav Vedanarayanan, MD, MBBS Femoral, Obturator, and Lateral Femoral Cutaneous Neuropathies 27 Mark A. Ross, MD CME Questions 33 No one involved in the planning of this CME activity had any relevant financial relationships to disclose. -

Contents VII
Contents VII Contents Preface .............................. V 3.2 Supply of the Connective Tissue ....... 28 List of Abbreviations ................... VI Diffusion ......................... 28 Picture Credits ........................ VI Osmosis .......................... 29 3.3 The “Creep” Phenomenon ............ 29 3.4 The Muscle ....................... 29 Part A Muscle Chains 3.5 The Fasciae ....................... 30 Philipp Richter Functions of the Fasciae .............. 30 Manifestations of Fascial Disorders ...... 30 Evaluation of Fascial Tensions .......... 31 1 Introduction ..................... 2 Causes of Musculoskeletal Dysfunctions .. 31 1.1 The Significance of Muscle Chains Genesis of Myofascial Disorders ........ 31 in the Organism ................... 2 Patterns of Pain .................... 32 1.2 The Osteopathy of Dr. Still ........... 2 3.6 Vegetative Innervation of the Organs ... 34 1.3 Scientific Evidence ................. 4 3.7 Irvin M. Korr ...................... 34 1.4 Mobility and Stability ............... 5 Significance of a Somatic Dysfunction in the Spinal Column for the Entire Organism ... 34 1.5 The Organism as a Unit .............. 6 Significance of the Spinal Cord ......... 35 1.6 Interrelation of Structure and Function .. 7 Significance of the Autonomous Nervous 1.7 Biomechanics of the Spinal Column and System .......................... 35 the Locomotor System .............. 7 Significance of the Nerves for Trophism .. 35 .............. 1.8 The Significance of Homeostasis ....... 8 3.8 Sir Charles Sherrington 36 Inhibition of the Antagonist or Reciprocal 1.9 The Nervous System as Control Center .. 8 Innervation (or Inhibition) ............ 36 1.10 Different Models of Muscle Chains ..... 8 Post-isometric Relaxation ............. 36 1.11 In This Book ...................... 9 Temporary Summation and Local, Spatial Summation .................. 36 Successive Induction ................ 36 ......... 2ModelsofMyofascialChains 10 3.9 Harrison H. Fryette ................. 37 2.1 Herman Kabat 1950: Lovett’s Laws ..................... -

Plantar Fasciitis Exercises
Accurate Clinic 2401 Veterans Memorial Blvd. Suite16 Kenner, LA 70062 - 4799 Phone: 504.472.6130 Fax: 504.472.6128 www.AccurateClinic.com Plantar Fasciitis Exercise Getting the right plantar fasciitis exercise is imperative to ensure the injury doesn’t continue to affect performance. If not given the attention it needs, plantar fasciitis can flair up long after an athlete thinks they’ve recovered and badly damage training plans and competition aspirations. What is plantar fascia? Plantar fascia is a thick, fibrous band of connective tissue which originates at the heel bone and runs along the bottom of the foot in a fan-like manner, attaching to the base of each of the toes. A rather tough, resilient structure, the plantar fascia takes on a number of critical functions during running and walking. Although the fascia is invested with countless sturdy 'cables' of connective tissue called collagen fibres, it is certainly not immune to injury. In fact, about 5 to 10 per cent of all running injuries are inflammations of the fascia, an incidence rate which in the United States would produce about a million cases of plantar fasciitis per year, just among runners and joggers. Basketball players, tennis players, volleyballers, step-aerobics participants, and dancers are also prone to plantar problems, as are non-athletic people who spend a lot of time on their feet or suddenly become active after a long period of lethargy. Why does the fascia flare up? Although it is a fairly rugged structure, the plantar fascia is not very receptive to stretching, and yet stretching occurs in the fascia nearly every time the foot hits the ground. -

Axis Scientific 9-Part Foot with Muscles, Ligaments, Nerves & Arteries A-105857
Axis Scientific 9-Part Foot with Muscles, Ligaments, Nerves & Arteries A-105857 DORSAL VIEW LATERAL VIEW 53. Superficial Fibular (Peroneal) Nerve 71. Fibula 13. Fibularis (Peroneus) Longus Tendon 17. Anterior Talofibular Ligament 09. Fibularis (Peroneus) 72. Lateral Malleolus Tertius Tendon 21. Kager’s Fat Pad 07. Superior Extensor 15. Superior Fibular Retinaculum (Peroneal) Retinaculum 51. Deep Fibular Nerve 52. Anterior Tibial Artery 19. Calcaneal (Achilles) Tendon 16. Inferior Fibular 02. Tibialis Anterior Tendon (Peroneal) Retinaculum 42. Intermedial Dorsal 08. Inferior Extensor 73. Calcaneus Bone Cutaneous Nerve Retinaculum 43. Lateral Dorsal Cutaneous Nerve 44. Dorsalis Pedis Artery 11. Extensor Digitorum 32. Abductor Digiti Minimi Muscle Brevis Muscle 04. Extensor Hallucis Longus Tendon 48. Medial Tarsal Artery 06. Extensor Digitorum 10. Extensor Hallucis Longus Tendons Brevis Muscle 41. Medial Dorsal Cutaneous Nerve 49. Dorsal Metatarsal Artery 45. Deep Fibular (Peroneal) Nerve MEDIAL VIEW 22. Flexor Digitorum 46. Arcuate Artery Longus Muscle 68. Tibia 12. Dorsal Interossei Muscle 21. Kager’s Fat Pad 48. Medial Tarsal Artery 69. Medial Malleolus 27. Tibialis Posterior 81. Nail Tendon 18. Flexor Retinaculum 29. Abductor Hallucis Muscle 36. Flexor Muscle POSTERIOR VIEW PLANTAR VIEW 01. Tibialis Anterior Muscle 03. Extensor Hallucis 70. Interosseous Longus Muscle Membrane 23. Flexor Digitorum 05. Extensor Digitorum Longus Tendons Longus Muscle 26. Tibialis Posterior Muscle 14. Fibularis (Peroneus) 20. Soleus Muscle Brevis Muscle 24. Flexor Hallucis Longus Muscle 25. Flexor Hallucis Longus Tendon 67. Proper Plantar 66. Proper Plantar Digital Artery Digital Nerve 65. Proper Plantar Digital Nerve 80. Sesamoid Bone 31. Flexor Digitorum Brevis Tendons 19. Calcaneal (Achilles) Tendon 36. Flexor Muscle 29. -

Pathogenesis, Diagnosis, and Treatment of the Tarsal-Tunnel Syndrome
CLEVELAND CLINIC QUARTERLY Volume 37, January 1970 Copyright © 1970 by The Cleveland Clinic Foundation Printed in U.S.A. Pathogenesis, diagnosis, and treatment of the tarsal-tunnel syndrome THOMAS E. GRETTER, M.D. Department o£ Neurology ALAN H. WILDE, M.D. Department of Orthopaedic Surgery N recent years many peripheral nerve compression syndromes have been I recognized. The carpal-tunnel syndrome, or compression of the median nerve at the wrist beneath the transverse carpal ligament, is the com- monest nerve entrapment syndrome. Less familiar but no less important is the tarsal-tunnel syndrome. Since the first case reports of the tarsal-tunnel syndrome by Keck1 and by Lam,2 in 1962, this syndrome is being diag- nosed with increasing frequency. Within the last two years 17 patients with the tarsal-tunnel syndrome have been treated at the Cleveland Clinic. Our report presents a review of the pathogenesis, diagnosis, and treatment of the tarsal-tunnel syndrome. Anatomy The tarsal tunnel is a canal formed on the medial side of the foot and ankle by the medial malleolus of the tibia and the flexor retinaculum. The flexor retinaculum spans the medial malleolus of the tibia and the medial tubercle of the os calcis (Fig. 1). The space beneath the ligament is divided by septae into four compartments. Each compartment contains one of the four structures of the tarsal tunnel. These structures are the pos- terior tibial tendon, flexor digitorum longus tendon, posterior tibial nerve, artery and veins, and the flexor hallucis longus tendon. Each tendon is invested with a separate synovial sheath. -

Hallux Varus As Complication of Foot Compartment Syndrome
The Journal of Foot & Ankle Surgery 50 (2011) 504–506 Contents lists available at ScienceDirect The Journal of Foot & Ankle Surgery journal homepage: www.jfas.org Tips, Quips, and Pearls “Tips, Quips, and Pearls” is a special section in The Journal of Foot & Ankle Surgery which is devoted to the sharing of ideas to make the practice of foot and ankle surgery easier. We invite our readers to share ideas with us in the form of special tips regarding diagnostic or surgical procedures, new devices or modifications of devices for making a surgical procedure a little bit easier, or virtually any other “pearl” that the reader believes will assist the foot and ankle surgeon in providing better care. Please address your tips to: D. Scot Malay, DPM, MSCE, FACFAS, Editor, The Journal of Foot & Ankle Surgery, PO Box 590595, San Francisco, CA 94159-0595; E-mail: [email protected] Hallux Varus as Complication of Foot Compartment Syndrome Paul Dayton, DPM, MS, FACFAS 1, Jean Paul Haulard, DPM, MS 2 1 Director, Podiatric Surgical Residency, Trinity Regional Medical Center, Fort Dodge, IA 2 Resident, Trinity Regional Medical Center, Fort Dodge, IA article info abstract Keywords: Hallux varus can present as a congenital deformity or it can be acquired secondary to trauma, surgery, or deformity neuromuscular disease. In the present report, we describe the presence of hallux varus as a sequela of great toe calcaneal fracture with entrapment of the medial plantar nerve in the calcaneal tunnel and recommend that metatarsophalangeal joint clinicians be wary of this when they clinically, and radiographically, evaluate patients after calcaneal fracture. -
Top 10 Positional-Release Therapy Techniques to Break the Chain of Pain, Part 1 Timothy E
Sacred Heart University DigitalCommons@SHU All PTHMS Faculty Publications Physical Therapy & Human Movement Science 2006 Top 10 Positional-Release Therapy Techniques to Break the Chain of Pain, Part 1 Timothy E. Speicher Sacred Heart University David O. Draper Brigham Young University - Utah Follow this and additional works at: http://digitalcommons.sacredheart.edu/pthms_fac Part of the Physical Therapy Commons, and the Somatic Bodywork and Related Therapeutic Practices Commons Recommended Citation Speicher, Tim and David O. Draper. "Top-10 Positional-Release Therapy Techniques to Break the Chjin of Pain: Part 1. Athletic Therapy Today 11.5 (2006): 69-71. This Peer-Reviewed Article is brought to you for free and open access by the Physical Therapy & Human Movement Science at DigitalCommons@SHU. It has been accepted for inclusion in All PTHMS Faculty Publications by an authorized administrator of DigitalCommons@SHU. For more information, please contact [email protected], [email protected]. THERAPEUTIC MODALITIES David O. Draper, EdD, ATC, Column Editor Top 10 Positional-Release Therapy Techniques to Break the Chain of Pain, Part 1 Tim Speicher, MS, ATC, CSCS • Sacred Heart University David O. Draper, EdD, ATC • Brigham Young University OSITIONAL-RELEASE therapy (PRT) is a counterstrained tissue, decreasing abberent gamma and treatment technique that is gaining popu- alpha neuronal activity, thereby breaking the sustained P larity. The purpose of this two-part column contraction.1 Jones’s original work and PRT theory have -

Plantar Fasciitis Stage 1
PLANTAR FASCIITIS STAGE 1 ADVICE Avoid those activities which aggravate your pain (e.g walking or running). SETS & REPS: N/A FREQUENCY: N/A AVOID FLIP-FLOPS Avoid wearing flip-flops SETS & REPS: N/A FREQUENCY: N/A AVOID HIGH HEELS Avoid high heels. SETS & REPS: N/A FREQUENCY: N/A PLANTAR FASCIA ICE MASSAGE Place a frozen water bottle on the floor and roll the bottle back and forth under your foot for 10 minutes. Do this at the end of each day and after activity. SETS & REPS: 10 mins FREQUENCY: Daily PLANTAR FASCIA MASSAGE Sitting, place a golf ball on the floor and roll the ball around under your foot concentrating on the tight, tender areas. SETS & REPS: 2-5 mins FREQUENCY: As needed © 2013 The Rehab Lab Limited. Used under license. No reproduction permitted without permission. www.therehablab.com PLANTAR FASCIITIS STAGE 1 PRONE GLUTEAL CONTRACTION Lie face-down and place your hands on your buttock muscles. Contract your gluteals, feeling the muscles tightening beneath your hands and hold for 5 seconds. Relax and repeat. SETS & REPS: 10 reps FREQUENCY: 1-2 x daily GLUTEAL STRETCH Sit on a chair and place your ankle on your opposite knee. With both hands, gently push down the knee of the crossed leg. Maintaining a straight back, bend forwards from the hips until you feel a stretch. Hold. SETS & REPS: 2 minute hold FREQUENCY: 1-2 x daily HAMSTRING STRETCH Place your heel on a knee-height table/chair with your knee slightly bent and tilt your pelvis forwards. While keeping your back straight, lean forwards until you feel a stretch in your hamstring. -

Measuring and Managing Foot Muscle Weakness Submitted by Penelope Jane Latey in Fulfilment of the Requirements for the Degree Of
MEASURING AND MANAGING FOOT MUSCLE WEAKNESS Penelope Jane Latey A thesis submitted in fulfilment of the requirement for the degree of Doctorate of Philosophy Faculty of Health Sciences The University of Sydney 2018 CANDIDATE’S CERTIFICATE I, Penelope Jane Latey, hereby declare that the work contained within this thesis is my own and has not been submitted to any other university or institution for any higher degree. I, Penelope Jane Latey, hereby declare that I was the principal researcher of all work contained in this thesis, including work published with multiple authors. I, Penelope Jane Latey, understand that if I am awarded a higher degree for my thesis titled Measuring and managing foot muscles weakness being submitted herewith for examination, the thesis will be lodged in the University Library and be will available immediately for use. I agree that the University Librarian (or in the case of the department, the Head of the Department) may supply a photocopy or microform of the thesis to an individual for research or study or to a library. Penelope Jane Latey 29th June 2018 i SUPERVISOR’S CERTIFICATE This is to certify that the thesis titled Measuring and managing foot muscle weakness submitted by Penelope Jane Latey in fulfilment of the requirements for the degree of Doctorate of Philosophy is in a form ready for examination. Professor Joshua Burns The University of Sydney and Sydney Children’s Hospitals Network 19th June 2018 ii ACKNOWLEDGEMENTS I would like to begin my acknowledgements with mention of my family, particularly my children, Frederick and Camilla for reminding me of what really matters.