Guidelines for Transfusion of Pediatric Patients Table of Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines for Transfusions
Guidelines for Transfu- sion Prepared by: Community Transfusion Committee Lincoln, Nebraska CHAIR: Aina Silenieks, MD MEMBERS: L. Bausch, M.D. R. Burton, M.D. S. Dunder, M.D. D. Voigt, M.D. B. J. Wilson, M.D. COMMUNITY Becky Croner REPRESENTATIVES: Ellen DiSalvo Christa Engel Phyllis Ericson Kelly Gillaspie Pat Gilles Vic Grdina Jessica Henrichs Kelly Jensen Laurel McReynolds Christina Nickel Angela Novotny Kelley Thiemann Janet Wachter Jodi Wikoff Guidelines For Transfusion Community Transfusion Committee INTRODUCTION The Community Transfusion Committee is a multidisciplinary group that meets to monitor blood utilization practices, establish guidelines for transfusion and discuss relevant transfusion related topics. It is comprised of physicians from local hospitals, invited guests, and community representatives from the hospitals’ transfusion services, nursing services, perfusion services, health information management, and the Nebraska Community Blood Bank. These Guidelines for Transfusion are reviewed and revised biannually by the Community Trans- fusion Committee to ensure that the industry’s most current practices are promoted. The Guidelines are the standard by which utilization practices are evaluated. They are also de- signed to provide helpful information to assist physicians to provide appropriate blood compo- nent therapy to patients. Appendices have been added for informational purposes and are not to be used as guidance for clinical decision making. ADULT RED CELLS A. Indications 1. One of the following a. Hypovolemia and hypoxia (signs/symptoms: syncope, dyspnea, postural hypoten- sion, tachycardia, angina, or TIA) secondary to surgery, trauma, GI tract bleeding, or intravascular hemolysis, OR b. Evidence of acute loss of 15% of total blood volume or >750 mL blood loss, OR c. -

27. Clinical Indications for Cryoprecipitate And
27. CLINICAL INDICATIONS FOR CRYOPRECIPITATE AND FIBRINOGEN CONCENTRATE Cryoprecipitate is indicated in the treatment of fibrinogen deficiency or dysfibrinogenaemia.1 Fibrinogen concentrate is licenced for the treatment of acute bleeding episodes in patients with congenital fibrinogen deficiency, including afibrinogenaemia and hypofibrinogenaemia,2 and is currently funded under the National Blood Agreement. Key messages y Fibrinogen is an essential component of the coagulation system, due to its role in initial platelet aggregation and formation of a stable fibrin clot.3 y The decision to transfuse cryoprecipitate or fibrinogen concentrate to an individual patient should take into account the relative risks and benefits.3 y The routine use of cryoprecipitate or fibrinogen concentrate is not advised in medical or critically ill patients.2,4 y Cryoprecipitate or fibrinogen concentrate may be indicated in critical bleeding if fibrinogen levels are not maintained using FFP. In the setting of major obstetric haemorrhage, early administration of cryoprecipitate or fibrinogen concentrate may be necessary.3 Clinical implications y The routine use of cryoprecipitate or fibrinogen concentrate in medical or critically ill patients with coagulopathy is not advised. The underlying causes of coagulopathy should be identified; where transfusion is considered necessary, the risks and benefits should be considered for each patient. Specialist opinion is advised for the management of disseminated intravascular coagulopathy (MED-PP18, CC-PP7).2,4 y Cryoprecipitate or fibrinogen concentrate may be indicated in critical bleeding if fibrinogen levels are not maintained using FFP. In patients with critical bleeding requiring massive transfusion, suggested doses of blood components is 3-4g (CBMT-PP10)3 in adults or as per the local Massive Transfusion Protocol. -

Cryosupernatant Plasma
Cryosupernatant Plasma APPLICABILITY: This document applies to Other Names: Cryopoor Plasma AHS, Covenant Health, and all other health Class: Human blood component care professionals involved in the transfusion of blood components and products in Alberta INTRAVENOUS OTHER Intermittent Continuous ROUTES DIRECT IV SC IM OTHER Infusion Infusion Acceptable No Yes No No No N/A Routes* * Professionals performing these restricted activities have received authorization from their regulatory college and have the knowledge and skill to perform the skill competently. DESCRIPTION OF PRODUCT: . Cryosupernatant Plasma (CSP) is prepared from slowly thawed Frozen Plasma that is centrifuged to separate the insoluble cryopreciptate from the plasma. The remaining Cryosupernatant plasma is then refrozen. The approximate volume of a unit is 273 mL . CSP has reduced levels of Factor VIII and von Willebrand Factor (vWF), and does not contain measurable amounts of Factor VIII or fibrinogen. Donors are screened and blood donations are tested for: . ABO/Rh and clinically significant antibodies . Antibodies to human immunodeficiency virus (HIV-1 and HIV-2), hepatitis C virus (HCV), human T-cell lymphotropic virus type I and II (HTLV-I/II), hepatitis B core antigen (HBcore) . Hepatitis B Surface Antigen (HBsAg) . Presence of viral RNA (HIV-1 and HCV) and viral DNA (hepatitis B virus (HBV)) . Syphilis AVAILABILITY: . Not all laboratories/transfusion services stock CSP. Product is stored frozen, and as a result requires preparation time prior to issuing. Patient blood type should be determined when possible to allow for ABO specific/compatible plasma transfusion INDICATIONS FOR USE: . Plasma exchange in patients with Thrombotic Thrombocytopenic Purpura (TTP) or Hemolytic Uremic Syndrome (HUS). -
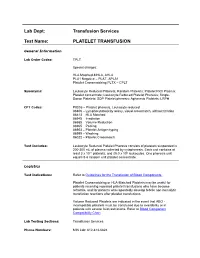
Platelet Transfusion
Lab Dept: Transfusion Services Test Name: PLATELET TRANSFUSION General Information Lab Order Codes: TPLT Special charges: HLA Matched-MHLA, AHLA PLA1 Negative – PLAT, APLA1 Platelet Crossmatching PLTX – CPLT Synonyms: Leukocyte Reduced Platelets; Random Platelets; Platelet Rich Plasma; Platelet concentrate; Leukocyte Reduced Platelet Pheresis; Single- Donor Platelets; SDP Platelet pheresis; Apheresis Platelets; LRPH CPT Codes: P9035 – Platelet pheresis, Leukocyte reduced 86806 – Lymphocytotoxicity assay, visual crossmatch, without titration 86813 – HLA Matched 86945 – Irradiation 86985 – Volume Reduction 86965 – Pooling 86903 – Platelet Antigen typing 86999 – Washing 86022 – Platelet Crossmatch Test Includes: Leukocyte Reduced Platelet Pheresis consists of platelets suspended in 200-300 mL of plasma collected by cytapheresis. Each unit contains at least 3 x 1011 platelets, and ≤5.0 x 106 leukocytes. One pheresis unit equals 5-6 random unit platelet concentrate. Logistics Test Indications: Refer to Guidelines for the Transfusion of Blood Components. Platelet Crossmatching or HLA-Matched Platelets may be useful for patients receiving repeated platelet transfusions who have become refractile, and for patients who repeatedly develop febrile non-hemolytic transfusion reactions after platelet transfusions. Volume Reduced Platelets are indicated in the event that ABO - incompatible platelets must be transfused due to availability or in patients with severe fluid restrictions. Refer to Blood Component Compatibility Chart Lab Testing Sections: Transfusion Services Phone Numbers: MIN Lab: 612-813-6824 STP Lab: 651-220-6558 Test Availability: Daily, 24 hours Turnaround Time: 1 - 2 hours Standard Dose/Volume: <10 kg: 10 – 15 mL/kg up to one unit or 50 mL maximum 10 – 15 kg: 1/3 pheresis unit 15 – 25 kg: 1/2 pheresis unit >25 kg: 1 pheresis unit Rate of Infusion: 10 minutes/unit, <4 hours Administration: Must be administered through a blood component administration filter. -

Policy and Procedure
Policy and Procedure Title: Exchange Transfusion for Sickle Cell Division: Medical Management Disease Department: Utilization Management Approval Date: 2/9/18 LOB: Medicaid, Medicare, HIV SNP, CHP, MetroPlus Gold, Goldcare I&II, Market Plus, Essential, HARP Effective Date: 2/9/18 Policy Number: UM-MP224 Review Date: 1/18/19 Cross Reference Number: Retired Date: Page 1 of 7 1. POLICY: Exchange Transfusion for Sickle Cell Disease 2. RESPONSIBLE PARTIES: Medical Management Administration, Utilization Management, Integrated Care Management, Claims Department, Provider Contracting 3. DEFINITIONS • Sickle cell disease – Sickle cell disease (SCD) refers to a group of inherited disorders characterized by sickled red blood cells (RBCs), caused either by homozygosity for the sickle hemoglobin mutation (HbSS; sickle cell anemia) or by compound heterozygosity for the sickle mutation and a second beta globin gene mutation (e.g., sickle-beta thalassemia, HbSC disease). In either HbSS or compound heterozygotes, the majority of Hgb is sickle Hgb (HgbS; i.e., >50 percent). • Transfusion – Simple transfusion refers to transfusion of RBCs without removal of the patient's blood. • Exchange Transfusion – Exchange transfusion involves transfusion of RBCs together with removal of the patient's blood. Exchange transfusion can be performed manually or via apheresis (also called cytapheresis or hemapheresis) using an extracorporeal continuous flow device. 4. PROCEDURE: A. Exchange transfusion for sickle cell disease will be covered as an ambulatory surgery procedure when all the following criteria are met: i) The member has documented SCD. ii) The exchange transfusion is a pre-scheduled procedure. iii) The purpose of the exchange transfusion is to prevent stroke, acute chest syndrome, or recurrent painful episodes. -

Sickle Cell Disease: Chronic Blood Transfusions
Sickle Cell Disease: Chronic Blood Transfusions There may be times when sickle cell patients require a blood transfusion. Such situations include preparing for surgery, during pregnancy, or during a severe complication such as an aplastic crisis, splenic sequestration or acute chest syndrome. In these cases, transfusion is a one-time intervention used to reduce the severity of the complication you are experiencing. However, if you have had a stroke, or an MRI or TCD shows that you are at high risk for having a stroke, your hematologist may recommend you begin chronic blood transfusions. What Does a Blood Transfusion Do? What are The Risks? Chronic (monthly) blood transfusions have been proven to Blood transfusions are not without risks. One risk is drastically reduce a sickle cell patient’s risk of stroke. They alloimmunization, a process in which the patient receiving have also been shown to reduce the frequency, severity blood transfusions creates antibodies to certain types of and duration of other sickle cell complications. Sickle cell blood. As a result he/she may have a reaction to the blood patients usually have a hemoglobin S level of about 80- that was transfused. Alloimmunization makes it more 90%. This means 80-90% of the circulating red blood cells difficult to find blood that is a good match for the patient. are cells that can sickle and cause complications. The goal In order to prevent alloimmunization, some centers of chronic blood transfusion therapy is to bring that routinely perform RBC phenotyping (special testing for percentage down below 30%. This will mean fewer sickle antibodies) on sickle cell disease patients so that they may cells circulating in the body, and a lower risk of give blood that is a better match for the patient. -
Guidelines for Transfusion and Patient Blood Management, and Discuss Relevant Transfusion Related Topics
Guidelines for Transfusion and Community Transfusion Committee Patient Blood Management Community Transfusion Committee CHAIR: Aina Silenieks, M.D., [email protected] MEMBERS: A.Owusu-Ansah, M.D. S. Dunder, M.D. M. Furasek, M.D. D. Lester, M.D. D. Voigt, M.D. B. J. Wilson, M.D. COMMUNITY Juliana Cordero, Blood Bank Coordinator, CHI Health Nebraska Heart REPRESENTATIVES: Becky Croner, Laboratory Services Manager, CHI Health St. Elizabeth Mackenzie Gasper, Trauma Performance Improvement, Bryan Medical Center Kelly Gillaspie, Account Executive, Nebraska Community Blood Bank Mel Hanlon, Laboratory Specialist - Transfusion Medicine, Bryan Medical Center Kyle Kapple, Laboratory Quality Manager, Bryan Medical Center Lauren Kroeker, Nurse Manager, Bryan Medical Center Christina Nickel, Clinical Laboratory Director, Bryan Medical Center Rachael Saniuk, Anesthesia and Perfusion Manager, Bryan Medical Center Julie Smith, Perioperative & Anesthesia Services Director, Bryan Medical Center Elaine Thiel, Clinical Quality Improvement/Trans. Safety Officer, Bryan Med Center Kelley Thiemann, Blood Bank Lead Technologist, CHI Health St. Elizabeth Cheryl Warholoski, Director, Nebraska Operations, Nebraska Community Blood Bank Jackie Wright, Trauma Program Manager, Bryan Medical Center CONSULTANTS: Jed Gorlin, M.D., Innovative Blood Resources [email protected] Michael Kafka, M.D., LifeServe Blood Center [email protected] Alex Smith, D.O., LifeServe Blood Center [email protected] Nancy Van Buren, M.D., Innovative -

Blood Product Modifications: Leukofiltration, Irradiation and Washing
Blood Product Modifications: Leukofiltration, Irradiation and Washing 1. Leukocyte Reduction Definitions and Standards: o Process also known as leukoreduction, or leukofiltration o Applicable AABB Standards, 25th ed. Leukocyte-reduced RBCs At least 85% of original RBCs < 5 x 106 WBCs in 95% of units tested . Leukocyte-reduced Platelet Concentrates: At least 5.5 x 1010 platelets in 75% of units tested < 8.3 x 105 WBCs in 95% of units tested pH≥6.2 in at least 90% of units tested . Leukocyte-reduced Apheresis Platelets: At least 3.0 x 1011 platelets in 90% of units tested < 5.0 x 106 WBCs 95% of units tested pH≥6.2 in at least 90% of units tested Methods o Filter: “Fourth-generation” filters remove 99.99% WBCs o Apheresis methods: most apheresis machines have built-in leukoreduction mechanisms o Less efficient methods of reducing WBC content . Washing, deglycerolizing after thawing a frozen unit, centrifugation . These methods do not meet requirement of < 5.0 x 106 WBCs per unit of RBCs/apheresis platelets. Types of leukofiltration/leukoreduction o “Pre-storage” . Done within 24 hours of collection . May use inline filters at time of collection (apheresis) or post collection o “Pre-transfusion” leukoreduction/bedside leukoreduction . Done prior to transfusion . “Bedside” leukoreduction uses gravity-based filters at time of transfusion. Least desirable given variability in practice and absence of proficiency . Alternatively performed by transfusion service prior to issuing Benefits of leukoreduction o Prevention of alloimmunization to donor HLA antigens . Anti-HLA can mediate graft rejection and immune mediated destruction of platelets o Leukoreduced products are indicated for transplant recipients or patients who are likely platelet transfusion dependent o Prevention of febrile non-hemolytic transfusion reactions (FNHTR) . -

Transfusion Triggers for Platelets and Other Blood Products Sunil Karanth Indian Journal of Critical Care Medicine (2019): 10.5005/Jp-Journals-10071-23250
INVITED ARTICLE Transfusion Triggers for Platelets and Other Blood Products Sunil Karanth Indian Journal of Critical Care Medicine (2019): 10.5005/jp-journals-10071-23250 INTRODUCTION Department of Intensive Care Unit, Manipal Hospital, Bengaluru, Transfusion of whole blood is not associated with any significant Karnataka, India benefit, rather can be harmful. Significant advances have been Corresponding Author: Sunil Karanth, Department of Intensive made in transfusion medicine, facilitating the use of blood product Care Unit, Manipal Hospital, Bengaluru, Karnataka, India, e-mail: or component therapy than use of whole blood (Fig. 1). In 2009, a [email protected] report on Serious Hazards of Transfusion in the UK, estimated that How to cite this article: Karanth S. Transfusion Triggers for Platelets a total of 3 million units of blood components were released. The and Other Blood Products. Indian J Crit Care Med 2019;23(Suppl requirement of the same in South-East Asia is much higher to the 3):S189–S190. tune of 15 million units annually. The current recommendation Source of support: Nil is to use blood only in life-threatening situations, rather than to Conflict of interest: None normalize abnormal numbers. PLATELETS Platelets are derived from the buffy coat of whole blood donations. A pooled platelet concentrate includes pooled buffy-coat derived platelets from four whole-blood donations suspended in platelet additive solution and plasma of one of the four donors. It contains 240000 platelets pooled from 4–6 donors. A Single donor platelet is derived from a single-donor by a process of apheresis. In view of the lesser number of donors and the theoretical advantage of involving a single-donor platelet (SDP) may be preferred over the use of platelets from multiple donors. -

Pediatric Orthotopic Heart Transplant Requiring Perioperative Exchange Transfusion: a Case Report
JECT. 2004;36:361–363 The Journal of The American Society of Extra-Corporeal Technology Case Reports Pediatric Orthotopic Heart Transplant Requiring Perioperative Exchange Transfusion: A Case Report Brian McNeer, BS; Brent Dickason, BS, RRT; Scott Niles, BA, CCP; Jay Ploessl, CCP The University of Iowa Hospitals and Clinics, Iowa City, Iowa Presented at the 41st International Conference of the American Society of Extra-Corporeal Technology, Las Vegas, Nevada, March 6–9, 2003 Abstract: An 11-month-old patient with idiopathic cardio- the venous line just proximal to the venous reservoir while si- myopathy was scheduled for orthotopic heart transplantation. A multaneously transfusing the normalized prime at normother- perioperative exchange transfusion was performed because of mia. Approximately 125% of the patients calculated blood vol- elevated panel reactive antibody levels. This process was accom- ume was exchanged. This technique greatly reduces the likeli- plished in the operating room prior to instituting cardiopulmo- hood of hyperacute rejection. The exchange transfusion process, nary bypass using a modified cardiopulmonary bypass circuit. In in addition to the patient immature immune system, provides preparation for the procedure, the cardiopulmonary bypass cir- additional options in orthotopic heart transplantation for pa- cuit was primed with washed leukocyte-filtered banked packed tients that may otherwise not be considered suitable candi- red blood cells, fresh-frozen plasma, albumin, and heparin. Pump dates. Keywords: exchange transfusion, heart transplant, pediat- prime laboratory values were normalized prior to beginning the ric, panel reactive antibodies. JECT. 2004;36:361–363 exchange transfusion. The patient’s blood was downloaded from Despite continuing advances in the management of end- humoral sensitization is determined by the presence of a stage cardiac failure, cardiac transplantation remains the positive panel reactive antibody (PRA) screen. -

Blood-Platelet-Orders-Outpatient-V3
Blood / Platelet Orders Outpt v3 USE THIS ORDER SET FOR OUTPATIENT NON URGENT BLOOD OR PLATELET TRANSFUSION 24 Hours advanced notice required for infusion center NO MORE THAN 2 UNITS OF RED BLOOD CELLS CAN BE INFUSED IN THE INFUSION CENTER PER DAY BMH Outpatient Infusion Center: Fax completed order set to 843-522-7313/Phone 843-522-7680 Hospital Outpatient: Fax Completed order set to Registration at 843-522-5741 and notify Nursing Supervisor at 843-522-7653 Service Designation THIS IS NOT AN ADMISSION SET Patient Name ___________________________________ Patient DOB ____________ Service Designation Blood Platelet Outpatient Attending ___________________________________ Date Requested ___________________________________ Status Outpatient Check Appropriate Diagnosis Below: [ Anemia of chronic renal disease Anemia related to chemotherapy Aplastic anemia Anemia related to cancer Anemia related to blood loss Sickle cell disease Anemia unspecified Thombocytopenia (platelets) Other _________________________ ] Allergies Update Allergies in the Summary Panel in MEDITECH Special Requirement: (REQUIRES SPECIAL ORDER ONE DAY IN ADVANCE) Special Requirement RBC or Platelets REQUIRES SPECIAL ORDER ONE DAY IN ADVANCE [ Irradiated CMV Negative HgBS Negative ] Medications diphenhydrAMINE HCl (Benadryl) 25 mg orally single dose premedicate prior to transfusion diphenhydrAMINE HCl (Benadryl) 50 mg orally single dose premedicate prior to transfusion diphenhydrAMINE HCl (Benadryl) 25 mg intravenously single dose premedicate prior to transfusion diphenhydrAMINE -
Laboratory Best Transfusion Practice for Neonates, Infants and Children
Laboratory Best Transfusion Practice for Neonates, Infants and Children This summary guidance should be used in conjunction with the appropriate 20161 and 20122 BSH Guidelines and laboratory SOPs Compatibility testing Neonates and infants < 4 months Obtain neonatal and maternal transfusion history (including any fetal transfusions) for all admissions. Obtain a maternal sample for initial testing where possible, in addition to the patient sample. Red cell selection: no maternal antibodies present Select appropriate group and correct neonatal specification red cells. Group O D-negative red cells may be issued electronically without serological crossmatch. If the laboratory does not universally select group O D-negative red cells for this age group, blood group selection should either be controlled by the LIMS or an IAT crossmatch should be performed using maternal or neonatal plasma to serologically confirm ABO compatibility with both mother and neonate. Red cell selection: where there is maternal antibody Select appropriate group red cells, compatible with maternal alloantibody/ies. An IAT crossmatch should be performed using the maternal plasma. If it is not possible to obtain a maternal sample it is acceptable to crossmatch antigen-negative units against the infant’s plasma. Where paedipacks are being issued from one donor unit it is only necessary to crossmatch the first split pack. Subsequent split packs from this multi-satellite unit can be automatically issued without further crossmatch until the unit expires or the infant is older than 4 months. If packs from a different donor are required, an IAT crossmatch should be performed. Infants and children ≥ 4 months For infants and children from 4 months of age, pre-transfusion testing and compatibility procedures should be performed as recommended for adults.