Identification of P38 MAPK and JNK As New Targets for Correction of Wilson Disease-Causing ATP7B Mutants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Establishing the Pathogenicity of Novel Mitochondrial DNA Sequence Variations: a Cell and Molecular Biology Approach
Mafalda Rita Avó Bacalhau Establishing the Pathogenicity of Novel Mitochondrial DNA Sequence Variations: a Cell and Molecular Biology Approach Tese de doutoramento do Programa de Doutoramento em Ciências da Saúde, ramo de Ciências Biomédicas, orientada pela Professora Doutora Maria Manuela Monteiro Grazina e co-orientada pelo Professor Doutor Henrique Manuel Paixão dos Santos Girão e pela Professora Doutora Lee-Jun C. Wong e apresentada à Faculdade de Medicina da Universidade de Coimbra Julho 2017 Faculty of Medicine Establishing the pathogenicity of novel mitochondrial DNA sequence variations: a cell and molecular biology approach Mafalda Rita Avó Bacalhau Tese de doutoramento do programa em Ciências da Saúde, ramo de Ciências Biomédicas, realizada sob a orientação científica da Professora Doutora Maria Manuela Monteiro Grazina; e co-orientação do Professor Doutor Henrique Manuel Paixão dos Santos Girão e da Professora Doutora Lee-Jun C. Wong, apresentada à Faculdade de Medicina da Universidade de Coimbra. Julho, 2017 Copyright© Mafalda Bacalhau e Manuela Grazina, 2017 Esta cópia da tese é fornecida na condição de que quem a consulta reconhece que os direitos de autor são pertença do autor da tese e do orientador científico e que nenhuma citação ou informação obtida a partir dela pode ser publicada sem a referência apropriada e autorização. This copy of the thesis has been supplied on the condition that anyone who consults it recognizes that its copyright belongs to its author and scientific supervisor and that no quotation from the -

Stelios Pavlidis3, Matthew Loza3, Fred Baribaud3, Anthony
Supplementary Data Th2 and non-Th2 molecular phenotypes of asthma using sputum transcriptomics in UBIOPRED Chih-Hsi Scott Kuo1.2, Stelios Pavlidis3, Matthew Loza3, Fred Baribaud3, Anthony Rowe3, Iaonnis Pandis2, Ana Sousa4, Julie Corfield5, Ratko Djukanovic6, Rene 7 7 8 2 1† Lutter , Peter J. Sterk , Charles Auffray , Yike Guo , Ian M. Adcock & Kian Fan 1†* # Chung on behalf of the U-BIOPRED consortium project team 1Airways Disease, National Heart & Lung Institute, Imperial College London, & Biomedical Research Unit, Biomedical Research Unit, Royal Brompton & Harefield NHS Trust, London, United Kingdom; 2Department of Computing & Data Science Institute, Imperial College London, United Kingdom; 3Janssen Research and Development, High Wycombe, Buckinghamshire, United Kingdom; 4Respiratory Therapeutic Unit, GSK, Stockley Park, United Kingdom; 5AstraZeneca R&D Molndal, Sweden and Areteva R&D, Nottingham, United Kingdom; 6Faculty of Medicine, Southampton University, Southampton, United Kingdom; 7Faculty of Medicine, University of Amsterdam, Amsterdam, Netherlands; 8European Institute for Systems Biology and Medicine, CNRS-ENS-UCBL, Université de Lyon, France. †Contributed equally #Consortium project team members are listed under Supplementary 1 Materials *To whom correspondence should be addressed: [email protected] 2 List of the U-BIOPRED Consortium project team members Uruj Hoda & Christos Rossios, Airways Disease, National Heart & Lung Institute, Imperial College London, UK & Biomedical Research Unit, Biomedical Research Unit, Royal -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Low Abundance of the Matrix Arm of Complex I in Mitochondria Predicts Longevity in Mice
ARTICLE Received 24 Jan 2014 | Accepted 9 Apr 2014 | Published 12 May 2014 DOI: 10.1038/ncomms4837 OPEN Low abundance of the matrix arm of complex I in mitochondria predicts longevity in mice Satomi Miwa1, Howsun Jow2, Karen Baty3, Amy Johnson1, Rafal Czapiewski1, Gabriele Saretzki1, Achim Treumann3 & Thomas von Zglinicki1 Mitochondrial function is an important determinant of the ageing process; however, the mitochondrial properties that enable longevity are not well understood. Here we show that optimal assembly of mitochondrial complex I predicts longevity in mice. Using an unbiased high-coverage high-confidence approach, we demonstrate that electron transport chain proteins, especially the matrix arm subunits of complex I, are decreased in young long-living mice, which is associated with improved complex I assembly, higher complex I-linked state 3 oxygen consumption rates and decreased superoxide production, whereas the opposite is seen in old mice. Disruption of complex I assembly reduces oxidative metabolism with concomitant increase in mitochondrial superoxide production. This is rescued by knockdown of the mitochondrial chaperone, prohibitin. Disrupted complex I assembly causes premature senescence in primary cells. We propose that lower abundance of free catalytic complex I components supports complex I assembly, efficacy of substrate utilization and minimal ROS production, enabling enhanced longevity. 1 Institute for Ageing and Health, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 2 Centre for Integrated Systems Biology of Ageing and Nutrition, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 3 Newcastle University Protein and Proteome Analysis, Devonshire Building, Devonshire Terrace, Newcastle upon Tyne NE1 7RU, UK. Correspondence and requests for materials should be addressed to T.v.Z. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

ATP5C1 Monoclonal Antibody
For Research Use Only ATP5C1 Monoclonal antibody Catalog Number:60284-1-Ig 3 Publications www.ptgcn.com Catalog Number: GenBank Accession Number: CloneNo.: Basic Information 60284-1-Ig BC000931 1B5A2 Size: GeneID (NCBI): Recommended Dilutions: 767 μg/ml 509 WB 1:500-1:2000 Source: Full Name: IHC 1:100-1:400 Mouse ATP synthase, H+ transporting, IF 1:50-1:500 Isotype: mitochondrial F1 complex, gamma IgG2a polypeptide 1 Purification Method: Calculated MW: Protein A purification 33 kDa Immunogen Catalog Number: Observed MW: AG1343 33 kDa Applications Tested Applications: Positive Controls: IF, IHC, WB,ELISA WB : human heart tissue; fetal human brain tissue Cited Applications: IHC : human liver cancer tissue; WB IF : HepG2 cells; Species Specificity: human Cited Species: human, zebrafish Note-IHC: suggested antigen retrieval with TE buffer pH 9.0; (*) Alternatively, antigen retrieval may be performed with citrate buffer pH 6.0 ATP5C1(ATP synthase subunit gamma, mitochondrial) is also named as ATP5C, ATP5CL1 and belongs to the ATPase Background Information gamma chain family. Some scientists reported the complete sequence of the gene for the human ATP synthase gamma subunit and described tissue-specific isoforms of the subunit generated by alternative splicing of exon 9. The liver (L) isoform differed from the heart (H) isoform by the addition of a single amino acid (asp273) at the C terminus. (PMID:8227057). Notable Publications Author Pubmed ID Journal Application Zhenhong Ni 29165041 Autophagy WB Danni Chen 30916346 Nucleic Acids Res WB Qinghai Zhang 33836087 Nucleic Acids Res WB Storage: Storage Store at -20ºC. Stable for one year after shipment. -

Fig1-13Tab1-5.Pdf
Supplementary Information Promoter hypomethylation of EpCAM-regulated bone morphogenetic protein genes in advanced endometrial cancer Ya-Ting Hsu, Fei Gu, Yi-Wen Huang, Joseph Liu, Jianhua Ruan, Rui-Lan Huang, Chiou-Miin Wang, Chun-Liang Chen, Rohit R. Jadhav, Hung-Cheng Lai, David G. Mutch, Paul J. Goodfellow, Ian M. Thompson, Nameer B. Kirma, and Tim Hui-Ming Huang Tables of contents Page Table of contents 2 Supplementary Methods 4 Supplementary Figure S1. Summarized sequencing reads and coverage of MBDCap-seq 8 Supplementary Figure S2. Reproducibility test of MBDCap-seq 10 Supplementary Figure S3. Validation of MBDCap-seq by MassARRAY analysis 11 Supplementary Figure S4. Distribution of differentially methylated regions (DMRs) in endometrial tumors relative to normal control 12 Supplementary Figure S5. Network analysis of differential methylation loci by using Steiner-tree analysis 13 Supplementary Figure S6. DNA methylation distribution in early and late stage of the TCGA endometrial cancer cohort 14 Supplementary Figure S7. Relative expression of BMP genes with EGF treatment in the presence or absence of PI3K/AKT and Raf (MAPK) inhibitors in endometrial cancer cells 15 Supplementary Figure S8. Induction of invasion by EGF in AN3CA and HEC1A cell lines 16 Supplementary Figure S9. Knockdown expression of BMP4 and BMP7 in RL95-2 cells 17 Supplementary Figure S10. Relative expression of BMPs and BMPRs in normal endometrial cell and endometrial cancer cell lines 18 Supplementary Figure S11. Microfluidics-based PCR analysis of EMT gene panel in RL95-2 cells with or without EGF treatment 19 Supplementary Figure S12. Knockdown expression of EpCAM by different shRNA sequences in RL95-2 cells 20 Supplementary Figure S13. -

Single-Cell RNA Sequencing Reveals Renal Endothelium Heterogeneity and Metabolic Adaptation to Water Deprivation
BASIC RESEARCH www.jasn.org Single-Cell RNA Sequencing Reveals Renal Endothelium Heterogeneity and Metabolic Adaptation to Water Deprivation Sébastien J. Dumas,1,2 Elda Meta,1,2 Mila Borri,1,2 Jermaine Goveia,1,2 Katerina Rohlenova ,1,2 Nadine V. Conchinha,1,2 Kim Falkenberg,1,2 Laure-Anne Teuwen,1,2 Laura de Rooij,1,2 Joanna Kalucka,1,2 Rongyuan Chen,3 Shawez Khan,1,2 Federico Taverna,1,2 Weisi Lu,3 Magdalena Parys,1,2 Carla De Legher,1,2 Stefan Vinckier,1,2 Tobias K. Karakach ,1,2 Luc Schoonjans,1,2,3 Lin Lin,4,5 Lars Bolund,4,5 Mieke Dewerchin,1,2 Guy Eelen,1,2 Ton J. Rabelink,6 Xuri Li,3 Yonglun Luo,4,5,7,8 and Peter Carmeliet1,2,3 Due to the number of contributing authors, the affiliations are listed at the end of this article. ABSTRACT Background Renal endothelial cells from glomerular, cortical, and medullary kidney compartments are exposed to different microenvironmental conditions and support specific kidney processes. However, the heterogeneous phenotypes of these cells remain incompletely inventoried. Osmotic homeostasis is vitally important for regulating cell volume and function, and in mammals, osmotic equilibrium is regulated through the countercurrent system in the renal medulla, where water exchange through endothelium occurs against an osmotic pressure gradient. Dehydration exposes medullary renal endothelial cells to extreme hyperosmolarity, and how these cells adapt to and survive in this hypertonic milieu is unknown. Methods We inventoried renal endothelial cell heterogeneity by single-cell RNA sequencing .40,000 mouse renal endothelial cells, and studied transcriptome changes during osmotic adaptation upon water deprivation. -

ATP5D Shrna (M) Lentiviral Particles: Sc-141346-V
SANTA CRUZ BIOTECHNOLOGY, INC. ATP5D shRNA (m) Lentiviral Particles: sc-141346-V BACKGROUND APPLICATIONS Mitochondrial ATP synthase is composed of two multi-subunit complexes ATP5D shRNA (m) Lentiviral Particles is recommended for the inhibition of that utilize an inner membrane electrochemical gradient to catalyze the syn- ATP5D expression in mouse cells. thesis of ATP during oxidative phosphorylation. The two multi-subunit com- plexes are designated F1 and F0, the former of which comprises the soluble SUPPORT REAGENTS catalytic core and the latter of which comprises the membrane-spanning Control shRNA Lentiviral Particles: sc-108080. Available as 200 µl frozen proton channel of ATP synthase. F1 consists of five distinct subunits, desig- viral stock containing 1.0 x 106 infectious units of virus (IFU); contains an nated ATP5A, ATP5B, ATP5C1, ATP5D and ATP5E, while F0 consists of ten shRNA construct encoding a scrambled sequence that will not lead to the subunits, designated ATP5H, ATP5G1, ATP5I, ATP5G2, ATP5J2, ATP5J, specific degradation of any known cellular mRNA. ATP5G3, ATP5S, ATP5F1 and ATP5L. ATP5D (ATP synthase, H+ transporting, δ mitochondrial F1 complex, subunit) is a 168 amino acid protein that local- RT-PCR REAGENTS izes to the mitochondrial inner membrane and is encoded by a gene that maps to human chromosome 19p13.3. Semi-quantitative RT-PCR may be performed to monitor ATP5D gene expres- sion knockdown using RT-PCR Primer: ATP5D (m)-PR: sc-141346-PR (20 µl). REFERENCES Annealing temperature for the primers should be 55-60° C and the extension temperature should be 68-72° C. 1. Jordan, E.M., et al. -

Expression Profiling of Substantia Nigra in Parkinson Disease, Progressive Supranuclear Palsy, and Frontotemporal Dementia with Parkinsonism
ORIGINAL CONTRIBUTION Expression Profiling of Substantia Nigra in Parkinson Disease, Progressive Supranuclear Palsy, and Frontotemporal Dementia With Parkinsonism Michael A. Hauser, PhD; Yi-Ju Li, PhD; Hong Xu, MA; Maher A. Noureddine, PhD; Yujun S. Shao, PhD; Steven R. Gullans, PhD; Clemens R. Scherzer, MD; Roderick V. Jensen, PhD; Adam C. McLaurin, BA; Jason R. Gibson, BA; Burton L. Scott, MD; Rita M. Jewett, RN; Judith E. Stenger, PhD; Donald E. Schmechel, MD; Christine M. Hulette, MD, PhD; Jeffery M. Vance, MD, PhD Background: Parkinson disease (PD) is characterized Results: There were 142 genes that were significantly by loss of dopaminergic neurons in the substantia nigra. differentially expressed between PD cases and controls Genes contributing to rare mendelian forms of PD have and 96 genes that were significantly differentially ex- been identified, but the genes involved in the more com- pressed between the combined progressive supra- mon idiopathic PD are not well understood. nuclear palsy and frontotemporal dementia with parkin- sonism cases and controls. The 12 genes common to all Objectives: To identify genes important to PD patho- 3 disorders may be related to secondary effects. Hierar- genesis using microarrays and to investigate their poten- chical cluster analysis after exclusion of these 12 genes tial to aid in diagnosing parkinsonism. differentiated 4 of the 6 PD cases from progressive su- pranuclear palsy and frontotemporal dementia with par- Design: Microarray expression analysis of postmortem kinsonism. substantia nigra tissue. Conclusions: Four main molecular pathways are al- Patients: Substantia nigra samples from 14 unrelated tered in PD substantia nigra: chaperones, ubiquitina- individuals were analyzed, including 6 with PD, 2 with tion, vesicle trafficking, and nuclear-encoded mitochon- progressive supranuclear palsy, 1 with frontotemporal de- drial genes. -
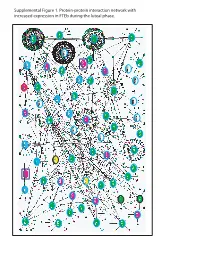
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

Integrating Bioinformatics and Physiology to Describe Genetic Effects in Complex Polygenic Diseases
Integrating bioinformatics and physiology to describe genetic effects in complex polygenic diseases Parikh, Hemang 2009 Link to publication Citation for published version (APA): Parikh, H. (2009). Integrating bioinformatics and physiology to describe genetic effects in complex polygenic diseases. Department of Clinical Sciences, Lund University. Total number of authors: 1 General rights Unless other specific re-use rights are stated the following general rights apply: Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Read more about Creative commons licenses: https://creativecommons.org/licenses/ Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. LUND UNIVERSITY PO Box 117 221 00 Lund +46 46-222 00 00 Integrating bioinformatics and physiology to describe genetic effects in complex polygenic diseases ACADEMIC DISSERTATION Hemang Parikh Lund University Department of Clinical Sciences Diabetes and Endocrinology Malmö University Hospital With the permission of the Medical Faculty of Lund University, to be presented for public examination in the Grand Hall at the Medical Research Center, Entrance 59, Malmö University Hospital, on January 23rd, 2009, at 9:00 a.m.