DNA Methylation in the Pathogenesis of Polycystic Ovary Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

The Transcriptomic Landscape of Prostate Cancer Development and Progression: an Integrative Analysis
cancers Article The Transcriptomic Landscape of Prostate Cancer Development and Progression: An Integrative Analysis Jacek Marzec 1,† , Helen Ross-Adams 1,*,† , Stefano Pirrò 1 , Jun Wang 1 , Yanan Zhu 2, Xueying Mao 2, Emanuela Gadaleta 1 , Amar S. Ahmad 3, Bernard V. North 3, Solène-Florence Kammerer-Jacquet 2, Elzbieta Stankiewicz 2, Sakunthala C. Kudahetti 2, Luis Beltran 4, Guoping Ren 5, Daniel M. Berney 2,4, Yong-Jie Lu 2 and Claude Chelala 1,6,* 1 Bioinformatics Unit, Centre for Cancer Biomarkers and Biotherapeutics, Barts Cancer Institute, Queen Mary University of London, London EC1M 6BQ, UK; [email protected] (J.M.); [email protected] (S.P.); [email protected] (J.W.); [email protected] (E.G.) 2 Centre for Cancer Biomarkers and Biotherapeutics, Barts Cancer Institute, Queen Mary University of London, London EC1M 6BQ, UK; [email protected] (Y.Z.); [email protected] (X.M.); solenefl[email protected] (S.-F.K.-J.); [email protected] (E.S.); [email protected] (S.C.K.); [email protected] (D.M.B.); [email protected] (Y.-J.L.) 3 Centre for Cancer Prevention, Wolfson Institute of Preventive Medicine, Barts and the London School of Medicine, Queen Mary University of London, London EC1M 6BQ, UK; [email protected] (A.S.A.); [email protected] (B.V.N.) 4 Department of Pathology, Barts Health NHS, London E1 F1R, UK; [email protected] 5 Department of Pathology, The First Affiliated Hospital, Zhejiang University Medical College, Hangzhou 310058, China; [email protected] 6 Centre for Computational Biology, Life Sciences Initiative, Queen Mary University London, London EC1M 6BQ, UK * Correspondence: [email protected] (H.R.-A.); [email protected] (C.C.) † These authors contributed equally to this work. -

Confidential: for Review Only Can the Impact of Childhood Adiposity on Disease Risk Be Reversed?: Mendelian Randomization Study
BMJ Confidential: For Review Only Can the impact of childhood adiposity on disease risk be reversed?: Mendelian randomization study Journal: BMJ Manuscript ID BMJ-2019-052821 Article Type: Research BMJ Journal: BMJ Date Submitted by the 28-Sep-2019 Author: Complete List of Authors: Richardson, Tom; University of Bristol Faculty of Health Sciences, MRC Integrative Epidemiology Unit Sanderson, Eleanor; University of Bristol, Population Health Sciences Elsworth, Benjamin; University of Bristol, MRC Integrative Epidemiology Unit (IEU), Bristol Medical School: Population Health Science Tilling, Kate; University of Bristol Faculty of Health Sciences Davey Smith, George; MRC Centre for Causal Analyses in Translational Epidemiology, Department of Social Medicine Keywords: Mendelian randomization, Mediation, Early life adiposity https://mc.manuscriptcentral.com/bmj Page 1 of 173 BMJ 1 2 3 4 Can the impact of childhood adiposity on disease risk be reversed? 5 6 A Mendelian randomization study 7 8 9 10 11 Tom G. Confidential:Richardson1,*, Eleanor Sanderson1 , ForBenjamin ReviewElsworth1, Kate Tilling Only1, George Davey Smith1 12 13 1MRC Integrative Epidemiology Unit (IEU), Population Health Sciences, Bristol Medical School, University of 14 15 Bristol, Oakfield House, Oakfield Grove, Bristol, BS8 2BN, United Kingdom 16 17 18 19 *Corresponding author: Dr Tom G. Richardson, MRC Integrative Epidemiology Unit, Population 20 21 Health Sciences, Bristol Medical School, University of Bristol, Oakfield House, Oakfield Grove, Bristol 22 23 BS8 2BN, UK. Tel: +44 (0)117 3313370; E-mail: [email protected] 24 25 26 27 28 Word Count: 4,344 29 30 Key words: Mendelian randomization, Early life adiposity, Mediation 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 https://mc.manuscriptcentral.com/bmj BMJ Page 2 of 173 1 2 3 4 5 Abstract 6 Objective: To evaluate whether early life adiposity has an independent effect on later life 7 8 disease risk or whether its influence is mediated by adulthood body mass index (BMI). -

Apoptotic Actions of Estrogen Receptor Β in Prostate Cancer
Antiproliferative and pro-apoptotic actions of Estrogen receptor β in prostate cancer A Dissertation Presented to the Faculty of the Department of Biology and Biochemistry University of Houston In Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy By Prasenjit Dey May 2013 Antiproliferative and pro-apoptotic actions of Estrogen receptor β in prostate cancer Prasenjit Dey APPROVED: Dr. Jan-Åke Gustafsson, Chairman Dr. Anders M. Ström Dr. Robert Schwartz Dr. Paul Webb Dr. Yuhong Wang Dr. Dan Wells, Dean, College of Natural Sciences and Mathematics ii Dedicated to my parents, brother, sister and my beloved wife for their support and encouragement. iii Acknowledgements I would like to express my sincere thanks to my advisor, Dr. Jan-Åke Gustafsson, for giving me the opportunity and his relentless guidance, encouragement, support, and valuable inputs throughout this endeavor. I would also like to thank him especially for the valuable inputs towards my dissertation. His readiness to discuss the progress of the work and expert suggestions helped me to complete the studies. I am also immensely thankful to my co-supervisor Dr. Anders M Ström. In many of the conversations we have had over the last three and half years, he generously shared with me his deep insight about estrogen receptor and its impact on cancer. I would also like to thank him for his extreme patience in listening to every single question I came up with and providing immensely helpful solutions. Without his time and effort, completion of all this work would have been impossible. I would also like to sincerely thank my committee members Dr. -

Studies on Mature Endothelial Cells and CD34+ Stem Cells
Exploring Mechanisms for Improvement of Cardiovascular Disease; Studies on Mature + Endothelial Cells and CD34 Stem Cells Sherin M. Bakhashab Institute of Cellular Medicine Faculty of Medical Sciences University of Newcastle A thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy May 2015 Abstract ABSTRACT Cardiovascular disease (CVD) is the major cause of morbidity and mortality worldwide and in particular in diabetes mellitus (DM). Although metformin has been shown to reduce CVD in Type-2 DM clinical trials, the underlying cardioprotective mechanism remains unexplored. Objective: to determine the effect of metformin on mature endothelial and stem cells exposed to hypoxia, hyperglycaemia or both conditions combined. Human umbilical vein endothelial cells (HUVEC) were studied by scratch test for migration and flow cytometry for apoptosis after culture in euglycaemia or hyperglycaemia, and/or hypoxia with or without metformin. mRNA was assayed by whole transcript microarrays. Genes of interest were confirmed by quantitative real-time PCR (qRT-PCR), proteins by western blot assay or flow cytometry. Metformin increased cell survival and migration via activation of vascular endothelial growth factor (VEGF) signalling, through upregulation of matrix metalloproteinase 16, and ERK/mitogen-activated protein kinase signalling under hyperglycaemia-hypoxia. Paracrine secretion of CD34+ cells treated with euglycaemia or hyperglycaemia, and/or hypoxia with or without metformin was assessed by measuring pro-inflammatory cytokines, VEGFA, chemokine (C-X-C Motif) ligand 10 (CXCL10), tissue inhibitor of metalloproteinase 1 (TIMP1) and efficacy to promote in vitro tube formation by HUVECs. Additionally, miR-126 was evaluated in exosomes and exosome-depleted medium, which was found to be increased by metformin. -

UC San Diego Electronic Theses and Dissertations
UC San Diego UC San Diego Electronic Theses and Dissertations Title Cardiac Stretch-Induced Transcriptomic Changes are Axis-Dependent Permalink https://escholarship.org/uc/item/7m04f0b0 Author Buchholz, Kyle Stephen Publication Date 2016 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California UNIVERSITY OF CALIFORNIA, SAN DIEGO Cardiac Stretch-Induced Transcriptomic Changes are Axis-Dependent A dissertation submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Bioengineering by Kyle Stephen Buchholz Committee in Charge: Professor Jeffrey Omens, Chair Professor Andrew McCulloch, Co-Chair Professor Ju Chen Professor Karen Christman Professor Robert Ross Professor Alexander Zambon 2016 Copyright Kyle Stephen Buchholz, 2016 All rights reserved Signature Page The Dissertation of Kyle Stephen Buchholz is approved and it is acceptable in quality and form for publication on microfilm and electronically: Co-Chair Chair University of California, San Diego 2016 iii Dedication To my beautiful wife, Rhia. iv Table of Contents Signature Page ................................................................................................................... iii Dedication .......................................................................................................................... iv Table of Contents ................................................................................................................ v List of Figures ................................................................................................................... -

Thousands of Cpgs Show DNA Methylation Differences in ACPA-Positive Individuals
G C A T T A C G G C A T genes Article Thousands of CpGs Show DNA Methylation Differences in ACPA-Positive Individuals Yixiao Zeng 1,2, Kaiqiong Zhao 2,3, Kathleen Oros Klein 2, Xiaojian Shao 4, Marvin J. Fritzler 5, Marie Hudson 2,6,7, Inés Colmegna 6,8, Tomi Pastinen 9,10, Sasha Bernatsky 6,8 and Celia M. T. Greenwood 1,2,3,9,11,* 1 PhD Program in Quantitative Life Sciences, Interfaculty Studies, McGill University, Montréal, QC H3A 1E3, Canada; [email protected] 2 Lady Davis Institute for Medical Research, Jewish General Hospital, Montréal, QC H3T 1E2, Canada; [email protected] (K.Z.); [email protected] (K.O.K.); [email protected] (M.H.) 3 Department of Epidemiology, Biostatistics and Occupational Health, McGill University, Montréal, QC H3A 1A2, Canada 4 Digital Technologies Research Centre, National Research Council Canada, Ottawa, ON K1A 0R6, Canada; [email protected] 5 Cumming School of Medicine, University of Calgary, Calgary, AB T2N 1N4, Canada; [email protected] 6 Department of Medicine, McGill University, Montréal, QC H4A 3J1, Canada; [email protected] (I.C.); [email protected] (S.B.) 7 Division of Rheumatology, Jewish General Hospital, Montréal, QC H3T 1E2, Canada 8 Division of Rheumatology, McGill University, Montréal, QC H3G 1A4, Canada 9 Department of Human Genetics, McGill University, Montréal, QC H3A 0C7, Canada; [email protected] 10 Center for Pediatric Genomic Medicine, Children’s Mercy, Kansas City, MO 64108, USA 11 Gerald Bronfman Department of Oncology, McGill University, Montréal, QC H4A 3T2, Canada * Correspondence: [email protected] Citation: Zeng, Y.; Zhao, K.; Oros Abstract: High levels of anti-citrullinated protein antibodies (ACPA) are often observed prior to Klein, K.; Shao, X.; Fritzler, M.J.; Hudson, M.; Colmegna, I.; Pastinen, a diagnosis of rheumatoid arthritis (RA). -

Immuntherapeutische Ansätze Beim Rhabdomyosarkom
Immuntherapeutische Ansätze beim Rhabdomyosarkom: Therapeutische Antikörper und Phagozytose Dissertation der Mathematisch-Naturwissenschaftlichen Fakultät der Eberhard Karls Universität Tübingen zur Erlangung des Grades eines Doktors der Naturwissenschaften (Dr. rer. nat.) vorgelegt von Delia Herrmann aus Ulm Tübingen 2011 Tag der mündlichen Qualifikation: 29.11.2011 Dekan: Prof. Dr. Wolfgang Rosenstiel 1. Berichterstatter: Prof. Dr. Sorin Armeanu-Ebinger 2. Berichterstatter: Prof. Dr. Olaf Rieß Inhaltsverzeichnis I Inhaltsverzeichnis Inhaltsverzeichnis .................................................................................................... I Abkürzungsverzeichnis ......................................................................................... V 1. Einleitung ........................................................................................................... 1 1.1 Das Rhabdomyosarkom (RMS) .......................................................................... 1 1.1.1 “Klassisches” ERMS ................................................................................ 2 1.1.2 ARMS ...................................................................................................... 2 1.2 Tumorimmunologie ............................................................................................. 4 1.2.1 Spezifische Tumorerkennung .................................................................. 4 1.2.2 Unspezifische Mechanismen ................................................................... 8 1.2.3 Immunevasion -
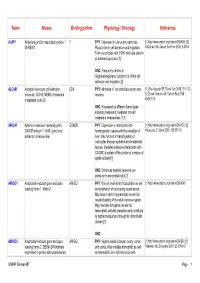
Name Aliases Binding Partner Physiology / Oncology References
Name Aliases Binding partner Physiology / Oncology References AJAP1 Adherens junction associated protein 1, ? PHY : Expressed in uterus and pancreas. [1] http://www.uniprot.org/uniprot/Q9UKB5. [2] SHREW1 Plays a role in cell adhesion and migration. McDonald JM, Cancer Biol Ther 2006, 5:300-4 Forms a complex with CDH1 and beta-catenin at adherens junctions [1] ONC : Frequently deleted in oligodendrogliomas, functions to inhibit cell adhesion and migration [2] ALCAM Activated leukocyte cell adhesion CD6 PHY : Adhesion of activated leukocytes and [1] Ofori-Acquah SF, Transl Res 2008, 151:122- molecule, CD166, MEMD (melanoma neurons 8. [2] van Kilsdonk JW, Cancer Res 2008, metastasis clone D) 68:3671-9 ONC : Expressed by different tumor types including melanoma; mediates cancer/ melanoma invasiveness [1,2] AMICA1 Adhesion molecule interacting with CXADR PHY : Expression is restricted to the [1] http://www.uniprot.org/uniprot/Q86YT9. [2] CXADR antigen 1, JAML (junctional hematopoietic tissues with the exception of Moog-Lutz C, Blood 2003, 102:3371-8 adhesion molecule-like) liver. May function in transmigration of leukocytes through epithelial and endothelial tissues. Mediates adhesive interactions with CXADR, a protein of the junctional complex of epithelial cells [1] ONC : Enhances myeloid leukemia cell adhesion to endothelial cells [2] AMIGO1 Amphoterin-induced gene and open AMIGO PHY : May be involved in fasciculation as well [1] http://www.uniprot.org/uniprot/Q86WK6 reading frame 1, Alivin-2 as myelination of developing neural axons. May have a role in regeneration as well as neural plasticity in the adult nervous system. May mediate homophilic as well as heterophilic cell-cell interaction and contribute to signal transduction through its intracellular domain [1] ONC : - AMIGO2 Amphoterin-induced gene and open AMIGO PHY : Highest levels in breast, ovary, cervix, [1] http://www.uniprot.org/uniprot/Q86SJ2. -

Deletion of 4Q28.3-31.23 in the Background of Multiple
Duga et al. Molecular Cytogenetics 2014, 7:36 http://www.molecularcytogenetics.org/content/7/1/36 CASE REPORT Open Access Deletion of 4q28.3-31.23 in the background of multiple malformations with pulmonary hypertension Balazs Duga1,2, Marta Czako1,2, Katalin Komlosi1,2, Kinga Hadzsiev1,2, Katalin Torok3, Katalin Sumegi1,2, Peter Kisfali1,2, Gyorgy Kosztolanyi1,2 and Bela Melegh1,2* Abstract The 4q deletion syndrome shows a broad spectrum of clinical manifestations consisting of key features comprising growth failure, developmental delay, craniofacial dysmorphism, digital anomalies, and cardiac and skeletal defects. We have identified a de novo interstitial distal deletion in a 9 month-old girl with growth failure, developmental delay, ventricular septum defect in the subaortic region, patent foramen ovale and patent ductus arteriosus, vascular malformation of the lung, dysgenesis of the corpus callosum and craniofacial dysmorphism using array-comparative genomic hybridization. This de novo deletion is located at 4q28.3-31.23 (136,127,048 - 150,690,325), its size is 14.56 Mb, and contains 8 relevant genes (PCDH18, SETD7, ELMOD2, IL15, GAB1, HHIP, SMAD1, NR3C2) with possible contributions to the phenotype. Among other functions, a role in lung morphogenesis and tubulogenesis can be attributed to the deleted genes in our patient, which may explain the unique feature of vascular malformation of the lung leading to pulmonary hypertension. With the detailed molecular characterization of our case with 4q- syndrome we hope to contribute to the -

Genome-Wide Associations and Functional Genomics
The Pharmacogenomics Journal (2013) 13, 456–463 & 2013 Macmillan Publishers Limited All rights reserved 1470-269X/13 www.nature.com/tpj ORIGINAL ARTICLE Pharmacogenomics of selective serotonin reuptake inhibitor treatment for major depressive disorder: genome-wide associations and functional genomics YJi1,7, JM Biernacka2,7, S Hebbring1, Y Chai1, GD Jenkins2, A Batzler2, KA Snyder3, MS Drews4, Z Desta5, D Flockhart5, T Mushiroda6, M Kubo6, Y Nakamura6, N Kamatani6, D Schaid2, RM Weinshilboum1 and DA Mrazek3 A genome-wide association (GWA) study of treatment outcomes (response and remission) of selective serotonin reuptake inhibitors (SSRIs) was conducted using 529 subjects with major depressive disorder. While no SNP associations reached the genome-wide level of significance, 14 SNPs of interest were identified for functional analysis. The rs11144870 SNP in the riboflavin kinase (RFK)geneon chromosome 9 was associated with 8-week treatment response (odds ratio (OR) ¼ 0.42, P ¼ 1.04 Â 10 À 6). The rs915120 SNP in the G protein-coupled receptor kinase 5 (GRK5) gene on chromosome 10 was associated with 8-week remission (OR ¼ 0.50, P ¼ 1.15 Â 10 À 5). Both SNPs were shown to influence transcription by a reporter gene assay and to alter nuclear protein binding using an electrophoretic mobility shift assay. This report represents an example of joining functional genomics with traditional GWA study results derived from a GWA analysis of SSRI treatment outcomes. The goal of this analytical strategy is to provide insights into the potential relevance of biologically plausible observed associations. The Pharmacogenomics Journal (2013) 13, 456–463; doi:10.1038/tpj.2012.32; published online 21 August 2012 Keywords: selective serotonin reuptake inhibitors; SSRI; genome-wide association study; GWA; functional genomics; major depressive disorder INTRODUCTION determine whether any identified candidate SNPs were associated Major depressive disorder (MDD) is a serious and prevalent with a change in function. -

Histone H2bub1 Deubiquitylation Is Essential for Mouse Development, but Does Not Regulate Global RNA Polymerase II Transcription
Cell Death & Differentiation (2021) 28:2385–2403 https://doi.org/10.1038/s41418-021-00759-2 ARTICLE Histone H2Bub1 deubiquitylation is essential for mouse development, but does not regulate global RNA polymerase II transcription 1,2,3,4 1,2,3,4,6 1,2,3,4,5 1,2,3,4 1,2,3,4 Fang Wang ● Farrah El-Saafin ● Tao Ye ● Matthieu Stierle ● Luc Negroni ● 1,2,3,4 1,2,3,4 1,2,3,4 1,2,3,4 1,2,3,4 Matej Durik ● Veronique Fischer ● Didier Devys ● Stéphane D. Vincent ● László Tora Received: 7 July 2020 / Revised: 18 February 2021 / Accepted: 23 February 2021 / Published online: 17 March 2021 © The Author(s) 2021. This article is published with open access Abstract Co-activator complexes dynamically deposit post-translational modifications (PTMs) on histones, or remove them, to regulate chromatin accessibility and/or to create/erase docking surfaces for proteins that recognize histone PTMs. SAGA (Spt-Ada-Gcn5 Acetyltransferase) is an evolutionary conserved multisubunit co-activator complex with modular organization. The deubiquitylation module (DUB) of mammalian SAGA complex is composed of the ubiquitin-specific protease 22 (USP22) and three adaptor proteins, ATXN7, ATXN7L3 and ENY2, which are all needed for the full activity of 1234567890();,: 1234567890();,: the USP22 enzyme to remove monoubiquitin (ub1) from histone H2B. Two additional USP22-related ubiquitin hydrolases (called USP27X or USP51) have been described to form alternative DUBs with ATXN7L3 and ENY2, which can also deubiquitylate H2Bub1. Here we report that USP22 and ATXN7L3 are essential for normal embryonic development of mice, however their requirements are not identical during this process, as Atxn7l3−/− embryos show developmental delay already at embryonic day (E) 7.5, while Usp22−/− embryos are normal at this stage, but die at E14.5.