Coagadex, Human Coagulation Factor X
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Rare Coagulation Disorders
Treatment OF HEMOPHILIA April 2006 · No. 39 THE RARE COAGULATION DISORDERS Paula HB Bolton-Maggs Department of Haematology Manchester Royal Infirmary Manchester, United Kingdom Published by the World Federation of Hemophilia (WFH) © World Federation of Hemophilia, 2006 The WFH encourages redistribution of its publications for educational purposes by not-for-profit hemophilia organizations. In order to obtain permission to reprint, redistribute, or translate this publication, please contact the Communications Department at the address below. This publication is accessible from the World Federation of Hemophilia’s web site at www.wfh.org. Additional copies are also available from the WFH at: World Federation of Hemophilia 1425 René Lévesque Boulevard West, Suite 1010 Montréal, Québec H3G 1T7 CANADA Tel. : (514) 875-7944 Fax : (514) 875-8916 E-mail: [email protected] Internet: www.wfh.org The Treatment of Hemophilia series is intended to provide general information on the treatment and management of hemophilia. The World Federation of Hemophilia does not engage in the practice of medicine and under no circumstances recommends particular treatment for specific individuals. Dose schedules and other treatment regimes are continually revised and new side effects recognized. WFH makes no representation, express or implied, that drug doses or other treatment recommendations in this publication are correct. For these reasons it is strongly recommended that individuals seek the advice of a medical adviser and/or to consult printed instructions provided by the pharmaceutical company before administering any of the drugs referred to in this monograph. Statements and opinions expressed here do not necessarily represent the opinions, policies, or recommendations of the World Federation of Hemophilia, its Executive Committee, or its staff. -

The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target
Thrombosis and Circulation Open Access Cimmino et al., J Thrombo Cir 2017, 3:1 Review Article Open Access The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target? Giovanni Cimmino*, Salvatore Fischetti and Paolo Golino Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, Naples, Italy *Corresponding author: Giovanni Cimmino, MD, PhD, Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, via Leonardo Bianchi, 180131 Naples, Italy. Tel: +39-081-7064175, Fax: +39-081-7064234; E-mail: [email protected] Received date: Dec 28, 2016, Accepted date: Jan 27, 2017, Published date: Jan 31, 2017 Copyright: © 2017 Giovanni C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acute thrombus formation is the pathophysiological substrate underlying several clinical conditions, such as acute coronary syndrome (ACS) and stroke. Activation of coagulation cascade is a key step of the thrombotic process: vessel injury results in exposure of the glycoprotein tissue factor (TF) to the flowing blood. Once exposed, TF binds factor VII/VIIa (FVII/FVIIa) and in presence of calcium ions, it forms a tertiary complex able to activate FX to FXa, FIX to FIXa, and FVIIa itself. The final step is thrombin formation at the site of vessel injury with subsequent platelet activation, fibrinogen to fibrin conversion and ultimately thrombus formation. Platelets are the key cells in primary hemostasis. -

RIASTAP®, Fibrinogen Concentrate (Human) Lyophilized Powder for Solution for Intravenous Injection
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------------CONTRAINDICATIONS ------------------------------------ These highlights do not include all the information needed to use RIASTAP • Known anaphylactic or severe systemic reactions to human plasma-derived products (4). safely and effectively. See full prescribing information for RIASTAP. ---------------------------------WARNINGS AND PRECAUTIONS---------------------------- RIASTAP®, Fibrinogen Concentrate (Human) • Monitor patients for early signs of anaphylaxis or hypersensitivity reactions and if necessary, discontinue administration and institute appropriate treatment (5.1). Lyophilized Powder for Solution for Intravenous Injection • Thrombotic events have been reported in patients receiving RIASTAP. Weigh the benefits of administration versus the risks of thrombosis (5.2). Initial U.S. Approval: 2009 • Because RIASTAP is made from human blood, it may carry a risk of transmitting ------------------------------------RECENT MAJOR CHANGES--------------------------------- infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent Indications and Usage (1) 06/2021 and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent (5.3). Dosage and Administration (2.2) 07/2020 -------------------------------------ADVERSE REACTIONS-------------------------------------- ----------------------------------INDICATIONS AND USAGE----------------------------------- • The most serious adverse reactions observed are thrombotic episodes (pulmonary RIASTAP, Fibrinogen -

Platelet Surface Glycoproteins. Studies on Resting and Activated Platelets and Platelet Membrane Microparticles in Normal Subjec
Platelet surface glycoproteins. Studies on resting and activated platelets and platelet membrane microparticles in normal subjects, and observations in patients during adult respiratory distress syndrome and cardiac surgery. J N George, … , N Kieffer, P J Newman J Clin Invest. 1986;78(2):340-348. https://doi.org/10.1172/JCI112582. Research Article The accurate definition of surface glycoprotein abnormalities in circulating platelets may provide better understanding of bleeding and thrombotic disorders. Platelet surface glycoproteins were measured on intact platelets in whole blood and platelet membrane microparticles were assayed in cell-free plasma using 125I-monoclonal antibodies. The glycoproteins (GP) studied were: GP Ib and GP IIb-IIIa, two of the major intrinsic plasma membrane glycoproteins; GMP-140, an alpha- granule membrane glycoprotein that becomes exposed on the platelet surface following secretion; and thrombospondin (TSP), an alpha-granule secreted glycoprotein that rebinds to the platelet surface. Thrombin-induced secretion in normal platelets caused the appearance of GMP-140 and TSP on the platelet surface, increased exposure of GP IIb-IIIa, and decreased antibody binding to GP Ib. Patients with adult respiratory distress syndrome had an increased concentration of GMP-140 and TSP on the surface of their platelets, demonstrating in vivo platelet secretion, but had no increase of platelet microparticles in their plasma. In contrast, patients after cardiac surgery with cardiopulmonary bypass demonstrated changes consistent with membrane fragmentation without secretion: a decreased platelet surface concentration of GP Ib and GP IIb with no increase of GMP-140 and TSP, and an increased plasma concentration of platelet membrane microparticles. These methods will help to define acquired abnormalities of platelet surface glycoproteins. -

Factor V Leiden Thrombophilia
Factor V Leiden thrombophilia Description Factor V Leiden thrombophilia is an inherited disorder of blood clotting. Factor V Leiden is the name of a specific gene mutation that results in thrombophilia, which is an increased tendency to form abnormal blood clots that can block blood vessels. People with factor V Leiden thrombophilia have a higher than average risk of developing a type of blood clot called a deep venous thrombosis (DVT). DVTs occur most often in the legs, although they can also occur in other parts of the body, including the brain, eyes, liver, and kidneys. Factor V Leiden thrombophilia also increases the risk that clots will break away from their original site and travel through the bloodstream. These clots can lodge in the lungs, where they are known as pulmonary emboli. Although factor V Leiden thrombophilia increases the risk of blood clots, only about 10 percent of individuals with the factor V Leiden mutation ever develop abnormal clots. The factor V Leiden mutation is associated with a slightly increased risk of pregnancy loss (miscarriage). Women with this mutation are two to three times more likely to have multiple (recurrent) miscarriages or a pregnancy loss during the second or third trimester. Some research suggests that the factor V Leiden mutation may also increase the risk of other complications during pregnancy, including pregnancy-induced high blood pressure (preeclampsia), slow fetal growth, and early separation of the placenta from the uterine wall (placental abruption). However, the association between the factor V Leiden mutation and these complications has not been confirmed. Most women with factor V Leiden thrombophilia have normal pregnancies. -

Factor V Leiden Thrombophilia Jody Lynn Kujovich, MD
GENETEST REVIEW Genetics in Medicine Factor V Leiden thrombophilia Jody Lynn Kujovich, MD TABLE OF CONTENTS Pathogenic mechanisms and molecular basis.................................................2 Obesity ...........................................................................................................8 Prevalence..............................................................................................................2 Surgery...........................................................................................................8 Diagnosis................................................................................................................2 Thrombosis not convincingly associated with Factor V Leiden....................8 Clinical diagnosis..............................................................................................2 Arterial thrombosis...........................................................................................8 Testing................................................................................................................2 Myocardial infarction.......................................................................................8 Indications for testing......................................................................................3 Stroke .................................................................................................................8 Natural history and clinical manifestations......................................................3 Genotype-phenotype -

Factor X Deficiency
FACTSHEET Factor X deficiency This factsheet is about a bleeding disorder If you carry one copy of the gene fault for that is related to problems with a blood factor X deficiency, you are known as a clotting factor called factor X (pronounced carrier. You can only pass the condition on to factor 10). It is written to go with our Rare your children if your partner also carries the bleeding disorders booklet, where you will gene fault. You will not have the condition find much more information on living with yourself, but any children that inherit the one of these conditions. gene fault from you will also be carriers of the condition. What is factor X deficiency? It is also possible to develop a factor X Factor X deficiency is a bleeding disorder deficiency later in life. This is called acquired caused by the body producing less of the factor X deficiency. Acquired factor X clotting factor than it should. This causes deficiency is not inherited and occurs in problems because the clotting reaction individuals with no family history of the that would normally control any bleeding disorder. This is rare, but may be caused is blocked too early. So, your body doesn’t by other diseases, including severe liver make the blood clots it needs to stop disease, amyloidosis, cancer and infections. bleeding. Factor X needs vitamin K from the liver to be activated. Symptoms of factor X deficiency Factor X deficiency is rare. Doctors estimate Symptoms of factor X deficiency can be that it affects about one in a million people. -
![PROTEIN C DEFICIENCY 1215 Adulthood and a Large Number of Children and Adults with Protein C Mutations [6,13]](https://docslib.b-cdn.net/cover/8040/protein-c-deficiency-1215-adulthood-and-a-large-number-of-children-and-adults-with-protein-c-mutations-6-13-1348040.webp)
PROTEIN C DEFICIENCY 1215 Adulthood and a Large Number of Children and Adults with Protein C Mutations [6,13]
Haemophilia (2008), 14, 1214–1221 DOI: 10.1111/j.1365-2516.2008.01838.x ORIGINAL ARTICLE Protein C deficiency N. A. GOLDENBERG* and M. J. MANCO-JOHNSON* *Hemophilia & Thrombosis Center, Section of Hematology, Oncology, and Bone Marrow Transplantation, Department of Pediatrics, University of Colorado Denver and The ChildrenÕs Hospital, Aurora, CO; and Division of Hematology/ Oncology, Department of Medicine, University of Colorado Denver, Aurora, CO, USA Summary. Severe protein C deficiency (i.e. protein C ment of acute thrombotic events in severe protein C ) activity <1 IU dL 1) is a rare autosomal recessive deficiency typically requires replacement with pro- disorder that usually presents in the neonatal period tein C concentrate while maintaining therapeutic with purpura fulminans (PF) and severe disseminated anticoagulation; protein C replacement is also used intravascular coagulation (DIC), often with concom- for prevention of these complications around sur- itant venous thromboembolism (VTE). Recurrent gery. Long-term management in severe protein C thrombotic episodes (PF, DIC, or VTE) are common. deficiency involves anticoagulation with or without a Homozygotes and compound heterozygotes often protein C replacement regimen. Although many possess a similar phenotype of severe protein C patients with severe protein C deficiency are born deficiency. Mild (i.e. simple heterozygous) protein C with evidence of in utero thrombosis and experience deficiency, by contrast, is often asymptomatic but multiple further events, intensive treatment and may involve recurrent VTE episodes, most often monitoring can enable these individuals to thrive. triggered by clinical risk factors. The coagulopathy in Further research is needed to better delineate optimal protein C deficiency is caused by impaired inactiva- preventive and therapeutic strategies. -
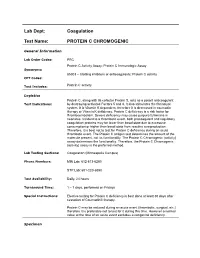
Lab Dept: Coagulation Test Name: PROTEIN C CHROMOGENIC
Lab Dept: Coagulation Test Name: PROTEIN C CHROMOGENIC General Information Lab Order Codes: PRC Protein C Activity Assay; Protein C Immunologic Assay Synonyms: 85303 – Clotting inhibitors or anticoagulants; Protein C activity CPT Codes: Test Includes: Protein C activity Logistics Protein C, along with its cofactor Protein S, acts as a potent anticoagulant Test Indications: by destroying activated Factors 5 and 8. It also stimulates the fibrinolytic system. It is Vitamin K dependent, therefore it is decreased in coumadin therapy or Vitamin K deficiency. Protein C deficiency is a risk factor for thromboembolism. Severe deficiency may cause purpura fulminans in neonates. Incident to a thrombotic event, both procoagulant and regulatory coagulation proteins may be lower than basal state due to excessive consumption or higher than basal state from reactive overproduction. Therefore, it is best not to test for Protein C deficiency during an acute thrombotic event. The Protein C antigen test determines the amount of the molecule present, not its functionality. The Protein C Chromogenic (activity) assay determines the functionality. Therefore, the Protein C Chromogenic (activity) assay is the preferred method. Lab Testing Sections: Coagulation (Minneapolis Campus) Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 – 7 days, performed on Fridays Special Instructions: Elective testing for Protein C deficiency is best done at least 30 days after cessation of Coumadin® therapy. Protein C may be reduced during an acute event (thrombotic, surgical, etc.) therefore it is preferable not to test for it during this time. However a normal value at the time of an acute event excludes a congenital deficiency. -

Assessing Plasmin Generation in Health and Disease
International Journal of Molecular Sciences Review Assessing Plasmin Generation in Health and Disease Adam Miszta 1,* , Dana Huskens 1, Demy Donkervoort 1, Molly J. M. Roberts 1, Alisa S. Wolberg 2 and Bas de Laat 1 1 Synapse Research Institute, 6217 KD Maastricht, The Netherlands; [email protected] (D.H.); [email protected] (D.D.); [email protected] (M.J.M.R.); [email protected] (B.d.L.) 2 Department of Pathology and Laboratory Medicine and UNC Blood Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +31-(0)-433030693 Abstract: Fibrinolysis is an important process in hemostasis responsible for dissolving the clot during wound healing. Plasmin is a central enzyme in this process via its capacity to cleave fibrin. The ki- netics of plasmin generation (PG) and inhibition during fibrinolysis have been poorly understood until the recent development of assays to quantify these metrics. The assessment of plasmin kinetics allows for the identification of fibrinolytic dysfunction and better understanding of the relationships between abnormal fibrin dissolution and disease pathogenesis. Additionally, direct measurement of the inhibition of PG by antifibrinolytic medications, such as tranexamic acid, can be a useful tool to assess the risks and effectiveness of antifibrinolytic therapy in hemorrhagic diseases. This review provides an overview of available PG assays to directly measure the kinetics of plasmin formation and inhibition in human and mouse plasmas and focuses on their applications in defining the role of plasmin in diseases, including angioedema, hemophilia, rare bleeding disorders, COVID- 19, or diet-induced obesity. -

Factor X Deficiency
Factor X deficiency Description Factor X deficiency is a rare bleeding disorder that varies in severity among affected individuals. The signs and symptoms of this condition can begin at any age, although the most severe cases are apparent in childhood. Factor X deficiency commonly causes nosebleeds, easy bruising, bleeding under the skin, bleeding of the gums, blood in the urine (hematuria), and prolonged or excessive bleeding following surgery or trauma. Women with factor X deficiency can have heavy or prolonged menstrual bleeding ( menorrhagia) or excessive bleeding in childbirth, and may be at increased risk of pregnancy loss (miscarriage). Bleeding into joint spaces (hemarthrosis) occasionally occurs. Severely affected individuals have an increased risk of bleeding inside the skull ( intracranial hemorrhage), in the lungs (pulmonary hemorrhage), or in the gastrointestinal tract, which can be life-threatening. Frequency Factor X deficiency occurs in approximately 1 per million individuals worldwide. Causes The inherited form of factor X deficiency, known as congenital factor X deficiency, is caused by mutations in the F10 gene, which provides instructions for making a protein called coagulation factor X. This protein plays a critical role in the coagulation system, which is a series of chemical reactions that forms blood clots in response to injury. Some F10 gene mutations that cause factor X deficiency reduce the amount of coagulation factor X in the bloodstream, resulting in a form of the disorder called type I. Other F10 gene mutations result in the production of a coagulation factor X protein with impaired function, leading to type II factor X deficiency. Reduced quantity or function of coagulation factor X prevents blood from clotting normally, causing episodes of abnormal bleeding that can be severe. -

Dental Management of a Patient with Factor X Deficiency
Clinical P RACTIC E Dental Management of a Patient with Factor X Deficiency Contact Author Abi Adewumi, BDS, FDSRCS (Eng), MPedDent RCS (Eng); Vishwas Sakhalkar, MD Dr. Adewumi Email: aadewumi@ dental.ufl.edu ABSTRACT Factor X deficiency (also known as Stuart-Prower factor deficiency) is an extremely rare hereditary hematologic disorder, affecting 1 person in 2 million. The gene causing this condition is autosomal recessive; thus, only those inheriting from both parents exhibit clinical symptoms, such as moderate bleeding, easy bruising and subcutaneous bleeding from mucous membranes. Patients with marked deficiency may have severe post- traumatic or spontaneous internal or external bleeding, leading to such complications as hemarthrosis or hemorrhagic strokes. This case report describes the dental manage- ment of a patient with severe factor X deficiency whose development was delayed due to multiple episodes of intracranial hemorrhage in early childhood. It also highlights the importance of timely interdisciplinary communication and consultation to promote a successful outcome. For citation purposes, the electronic version is the definitive version of this article: www.cda-adc.ca/jcda/vol-75/issue-6/461.html actor X deficiency is a coagulation dis- Case Report order reported in the mid-1950s by work- A 17-year-old presented to the pediatric Fers who were studying patients with a dental department of the University of Florida hemorrhagic disease resembling factor VII with the chief complaint of toothache. His deficiency. It was named after the first male medical history indicated severe factor X de- and female patients (Stuart and Prower) in ficiency, intracranial bleeding episodes and whom it was recognized.