Notice to Radioactive Materials
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Committee Reports 2005 Midyear Meeting
2004-2005 MIDYEAR REPORT Academic Education Committee Health Physics Society Mark Rudin - Chair Report Prepared by Mark J. Rudin, Ph.D. January 11, 2005 Abstract The Academic Education Committee (AEC) has been and continues to be very active in a number of areas. Accomplishments/activities during the first half of the 2004-2005 time period included: 1. Administration of Health Physics Society (HPS) Fellowship and Travel Grant Awards 2. Maintenance of Student Branch Programs 3. A fifth health physics program participated in the Applied Science Accreditation Commission (ASAC) of the American Board for Engineering and Technology, Inc. (ABET) accreditation process. Page 220 Report Outline: I. Recommendations for Action II. Subcommittee Assignments for 2004-2005 III. Progress Reports 2003-2004 HPS Fellow Selections 2003-2004 Student Travel Grants Student Branch Program Health Physics Education Reference Book Health Physics Program Directors Organization Accreditation Sub-Committee Revision of the Careers in Health Physics brochure I. Recommendations for Action 1. The Committee anxiously awaits the approval of its Rules/Operating Procedures. Once the rules are approved, the AEC will be able to appoint individuals from the AEC Subcommittee on Accreditation to the ANS and the American Academy of Health Physics. John Poston and Rich Brey have agreed to serve as the liasions for the ANS and Academy, respectively. 2. Chuck Roessler has graciously served as the HPS Commissioner on the Applied Sciences Accreditation Commission (ASAC) of ABET for two terms (2003-04 and 2004-05). Note that ASAC is the ABET commission under which accreditation of Health Physics Academic Programs is conducted. Commissioner terms are for one year with members eligible for reappointment for up to five terms. -

Radiation Risk in Perspective
PS010-1 RADIATION RISK IN PERSPECTIVE POSITION STATEMENT OF THE HEALTH HEALTH PHYSICS SOCIETY* PHYSICS SOCIETY Adopted: January 1996 Revised: August 2004 Contact: Richard J. Burk, Jr. Executive Secretary Health Physics Society Telephone: 703-790-1745 Fax: 703-790-2672 Email: [email protected] http://www.hps.org In accordance with current knowledge of radiation health risks, the Health Physics Society recommends against quantitative estimation of health risks below an individual dose of 5 rem1 in one year or a lifetime dose of 10 rem above that received from natural sources. Doses from natural background radiation in the United States average about 0.3 rem per year. A dose of 5 rem will be accumulated in the first 17 years of life and about 25 rem in a lifetime of 80 years. Estimation of health risk associated with radiation doses that are of similar magnitude as those received from natural sources should be strictly qualitative and encompass a range of hypothetical health outcomes, including the possibility of no adverse health effects at such low levels. There is substantial and convincing scientific evidence for health risks following high-dose exposures. However, below 5–10 rem (which includes occupational and environmental exposures), risks of health effects are either too small to be observed or are nonexistent. In part because of the insurmountable intrinsic and methodological difficulties in determining if the health effects that are demonstrated at high radiation doses are also present at low doses, current radiation protection standards and practices are based on the premise that any radiation dose, no matter how small, may result in detrimental health effects, such as cancer and hereditary genetic damage. -

Recommendations for the Follow-Up Assessment of Contaminated Travelers by Radiation Control Health Physics Staff
Recommendations for the Follow-Up Assessment of Contaminated Travelers by Radiation Control Health Physics Staff State radiation control program health physicists will perform the follow-up assessment of contaminated travelers in coordination with the local or state health department. This assessment may be done at the state radiation control program office, the traveler’s place of residence, or other locations as convenient. This screening process may be stressful for travelers. The health physics staff should consider requesting assistance from behavioral health professionals or risk communicators to help reduce anxiety for travelers throughout the process. The follow-up assessment should consist of four main activities: 1) Ensure the effectiveness of external decontamination 2) Assist in completion and review the Epidemiologic Assessment form with the traveler and assess potential for internal contamination 3) Perform a thyroid count 4) Evaluate the need for bioassay, and collect a urine sample if necessary Based on current environmental monitoring results reported from Japan, it is highly unlikely for any external or internal contamination to present a public health concern for people outside of the 50-mile (80-kilometer) radius around the Fukushima nuclear power plant. 1) Ensure the effectiveness of external decontamination Travelers identified as being contaminated with radioactive materials by U.S. Customs and Border Protection (CBP) are offered an opportunity – at the airport – to change into clean clothes and wash exposed skin surfaces, such as their hands and face. Additional washing (such as a full shower) may be necessary to remove all traces of external contamination. The effectiveness of external decontamination performed by the traveler at the airport or at home can be verified using a beta/gamma radiation detection instrument such as a Geiger Muller (GM) pancake probe or equivalent. -

Shieldalloy Metallurgical Corporation, Ltr Dtd 01/25/1993 Re: Application for Amendment of USNRC Source Material License
i S H I E L DA L LOY M ETA L LU R G I CA L C 0 R P0 RAT I 0 N WEST BOULEVARD P 0 BOX 768 NEWFIELD, NJ 08344 TELEPHONE (609) 692-4200 TWX (510) 687-8918 FAX (609) 692-4017 ENVIRONMENTAL DEPARTMENT FAX Certified Mail: P 284 355 015 (609) 697-9025 Return Receipt Requested January 25, 1993 Mr. Yawar H. Faraz Mail Stop 6H-3 Advanced Fuel & Special Facilities Section Fuel Cycle Safety Branch Division of Industrial and Medical Nuclear Safety Office of Nuclear Material Safety and Safeguards U.S. Nuclear Regulatory Commission Washington, D.C. 20555 RE: Application for Amendment of USNRC Source Material License Number SMB-743, Docket No. 40-7102 Dear Mr. Faraz: As recommended in your letter of December 15, 1992, Shieldalloy Metallurgical Corporation (SMC) is requesting amendment of Condition 12 of Source Material License Number SMB-743 to reflect the following administrative changes in its radiation protection program: 1. Overall control and authority for radiological protection at SMC shall rest with the Senior Vice President of Manufacturing, Mr. Richard D. Way. 2. The Radiation Safety Officer for SMC is Mr. Craig R. Rieman. A copy of Mr. Rieman s resume is attached. 3. The Assistant Radiation Safety Officer (ARSO) is Mr. James P. Valenti. A copy of Mr. Valenti I s resume is attached. 9305030276 530125 PDR ADOCK 04007102 C PDR Mr. Yawar H. Faraz U.S. Nuclear Regulatory Commission January 25, 1993 Page 2 4. In addition, Authorized Users for SMC are: David R. Smith Bill Grabus Knud Clausen Brian Martin AI Lashley Richard Bodine Robert A. -

Electrical Safety Policy and Manual
ELECTRICAL SAFETY POLICY AND MANUAL ELECTRICAL SAFETY POLICY IX. HIGH-VOLTAGE PLATFORMS ELECTRICAL SAFETY COMMITTEE CHARTER X. CAPACITORS ELECTRICAL SAFETY MANUAL XI. HAZARDOUS GASES AND LIQUIDS I. NATIONAL AND LOCAL STANDARDS XII. MAGNETS AND INDUCTORS • Permanent Installations 1. Fringe Fields • Temporary Experimental 2. Warning Signs Installations 3. Discharge 4. Connections II. SUPPLEMENTARY STANDARDS 5. Eddy Currents 6. Cooling III. POWER AND DISTRIBUTION 7. Construction CIRCUIT • Outlets and Power Supply XIII. ELECTROMAGNETIC RADIATION Output 8. Warning • Conductors 9. Monitoring • Circuits 10. Protection IV. SYSTEM NEUTRAL XIV. LASERS V. EQUIPMENT GROUNDING XV. WORKING ON ENERGIZED CIRCUITS VI. EXPOSED LIVE PARTS XVI. LOCKOUT/TAGOUT VII. ELECTRICAL EQUIPMENT XVII. TABLES PROTECTIVE MEASURES • Up to 600 V and Over 20 A • Over 600 V and 0.025 A or Stored Energy of 10 J VIII. OPERATIONS • General • Portable Electrical Equipment Electrical Safety Policy In keeping with the Physics Division Policy to give the highest priority to Environmental, Health, and Safety concerns in its operations, it is the intent of Physics Division management to prevent electrical hazards to staff and visitors and to assure adherence to applicable electrical safety codes. This will be accomplished through the development of operational procedures, the proper training of personnel, the design of equipment, and the establishment of an Electrical Safety Committee. ELECTRICAL SAFETY COMMITTEE CHARTER Responsibilities and Functions • Develop and revise as needed the Physics Division Electrical Safety Policy and Manual. • Annually review Lock-out/Tag-out log books. • Identify unsafe conditions and/or practices and assist in the development of remedial action plans. • Review electrical incidents, near-misses, and formulate preventive measures. -
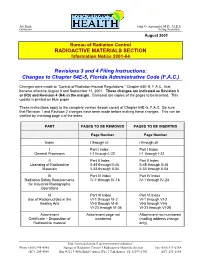
RADIOACTIVE MATERIALS SECTION Revisions 3 and 4 Filing Instructions
Jeb Bush John O. Agwunobi, M.D., M.B.A Governor Acting Secretary August 2001 Bureau of Radiation Control RADIOACTIVE MATERIALS SECTION Information Notice 2001-04 Revisions 3 and 4 Filing Instructions: Changes to Chapter 64E-5, Florida Administrative Code (F.A.C.) Changes were made to “Control of Radiation Hazard Regu lations,” Chapter 64E-5, F.A.C., that became effective August 8 and September 11, 2001. These changes are indicated as Revision 3 or (R3) and Revision 4 (R4) in the margin. Enclosed are copies of the pages to be inserted. This update is printed on blue paper. These instructions apply to the complete version (brown cover) of Chapter 64E -5, F.A.C. Be sure that Revision 1 and Revision 2 changes have been made before making these changes. This can be verified by checking page ii of the index. PART PAGES TO BE REMOVED PAGES TO BE INSERTED Page Number Page Number Index i through xii i through xii I Part I Index Part I Index General Provisions I-1 through I-22 I-1 through I-22 II Part II Index Part II Index Licensing of Radioactive II-45 through II-46 II-45 through II-46 Materials II-53 through II-54 II-53 through II-54 IV Part IV Index Part IV Index Radiation Safety Requirements IV-1 through IV-16 IV-1 through IV-24 for Industrial Radiographic Operations VI Part VI Index Part VI Index Use of Radionuclides in the VI-1 through VI-2 VI-1 through VI-2 Healing Arts VI-5 through VI-6 VI-5 through VI-6 VI-23 through VI-26 VI-23 through VI-26 Attachment Attachment page not Attachment not numbered Certificate – Disposition of numbered (mailing -

Radiation and Risk: Expert Perspectives Radiation and Risk: Expert Perspectives SP001-1
Radiation and Risk: Expert Perspectives Radiation and Risk: Expert Perspectives SP001-1 Published by Health Physics Society 1313 Dolley Madison Blvd. Suite 402 McLean, VA 22101 Disclaimer Statements and opinions expressed in publications of the Health Physics Society or in presentations given during its regular meetings are those of the author(s) and do not necessarily reflect the official position of the Health Physics Society, the editors, or the organizations with which the authors are affiliated. The editor(s), publisher, and Society disclaim any responsibility or liability for such material and do not guarantee, warrant, or endorse any product or service mentioned. Official positions of the Society are established only by its Board of Directors. Copyright © 2017 by the Health Physics Society All rights reserved. No part of this publication may be reproduced or distributed in any form, in an electronic retrieval system or otherwise, without prior written permission of the publisher. Printed in the United States of America SP001-1, revised 2017 Radiation and Risk: Expert Perspectives Table of Contents Foreword……………………………………………………………………………………………………………... 2 A Primer on Ionizing Radiation……………………………………………………………………………... 6 Growing Importance of Nuclear Technology in Medicine……………………………………….. 16 Distinguishing Risk: Use and Overuse of Radiation in Medicine………………………………. 22 Nuclear Energy: The Environmental Context…………………………………………………………. 27 Nuclear Power in the United States: Safety, Emergency Response Planning, and Continuous Learning…………………………………………………………………………………………….. 33 Radiation Risk: Used Nuclear Fuel and Radioactive Waste Disposal………………………... 42 Radiation Risk: Communicating to the Public………………………………………………………… 45 After Fukushima: Implications for Public Policy and Communications……………………. 51 Appendix 1: Radiation Units and Measurements……………………………………………………. 57 Appendix 2: Half-Life of Some Radionuclides…………………………………………………………. 58 Bernard L. -

ANL Physics Division ELECTRICAL SAFETY POLICY and MANUAL
ANL Physics Division ELECTRICAL SAFETY POLICY AND MANUAL 2007 ELECTRICAL SAFETY POLICY VII. ELECTRICAL EQUIPMENT PROTECTIVE MEASURES ELECTRICAL SAFETY COMMITTEE A. Up to 600 V and Over 20 A CHARTER B. Over 600 V and 0.025 A or Stored Energy of 10 J ELECTRICAL SAFETY MANUAL VIII. OPERATIONS I. NATIONAL AND LOCAL STANDARDS A. General A. Permanent Installations B. Portable Electrical Equipment B. Temporary Experimental Installations II. SUPPLEMENTARY STANDARDS IX. HIGH-VOLTAGE PLATFORMS III. POWER AND DISTRIBUTION CIRCUIT X. CAPACITORS A. Outlets and Power Supply Output XI. HAZARDOUS GASES AND LIQUIDS B. Conductors C. Circuits XII. MAGNETS AND INDUCTORS A. Fringe Fields IV. SYSTEM NEUTRAL B. Warning Signs C. Discharge V. EQUIPMENT GROUNDING D. Connections E. Eddy Currents F. Cooling VI. EXPOSED LIVE PARTS G. Construction XIII. ELECTROMAGNETIC RADIATION A. Warning XVI. TABLES B. Monitoring C. Protection XIV. WORKING ON ENERGIZED CIRCUITS XV. LOCKOUT/TAGOUT The official version of this Physics Division manual is found at www.phy.anl.gov/div/esh. This paper copy may be obsolete soon after it is printed. Call Tom Mullen with any content questions. Electrical Safety Policy In keeping with the Physics Division Policy to give the highest priority to Environmental, Health, and Safety concerns in its operations, it is the intent of Physics Division management to prevent electrical hazards to staff and visitors and to assure adherence to applicable electrical safety codes. This will be accomplished through the development of operational procedures, the proper training of personnel, the design of equipment, and the establishment of an Electrical Safety Committee. ELECTRICAL SAFETY COMMITTEE CHARTER Authorization The Physics Division Electrical Safety Committee is authorized by and reports to the Director of the Physics Division. -

Release of Patients Administered Radioactive Materials
NEW YORK STATE DEPARTMENT OF HEALTH BUREAU OF ENVIRONMENTAL RADIATION PROTECTION DRAFT RADIATION GUIDE 10.17 RELEASE OF PATIENTS ADMINISTERED RADIOACTIVE MATERIALS A. INTRODUCTION Section 16.123(b) of 10 NYCRR Part 16 requires licensees to assess the radiation exposure to individuals from patients administered radioactive materials and take action, as appropriate, to reduce exposures to other individuals. These requirements apply for both diagnostic and therapeutic uses regardless of the amount administered. Section 16.123(b), Medical uses of radioactive material, states: P The licensee shall confine patients undergoing procedures authorized by ...until the total effective dose equivalent for the individuals (other than the patient) likely to receive the greatest dose is 5 mSv (500 mrem) or less. P When the total effective dose equivalent to any individual that could result from the release of a patient is likely to exceed 1 mSv (100 mrem), the licensee shall: • provide the patient, or his/her competent representative, written information on risks of radiation and methods for reducing the exposure of individuals; and • keep records of such patients release for a period of five years. This document is designed to provide guidance on determining the potential dose to an individual likely to receive the highest dose from exposure to the patient, to establish appropriate activities and dose rates for release, to provide guidelines for instructions to patients on how to reduce exposures to other individuals, to describe recordkeeping requirements, and to inform licensees of other potential problems associated with the release of patients containing radioactive materials. B. DISCUSSION The radiation dose to another individual from a patient is highly dependent on a number of factors, including the amount and type of radioactive material administered, the patient's living/working arrangements, ability/willingness to follow instructions, etc. -
Radiation Sources- Radiating Health and Progress…
RADIATION SOURCES- RADIATING HEALTH AND PROGRESS…. ….. BUT NEED REGULATION NEVERTHELESS!!! Anuradha V ATOMIC ENERGY REGULATORY BOARD Contents- The four W’s What are radiation sources? Where are they used? Why do we need them? When is their use dangerous and how to overcome this? 3 Applications of Radiation- All areas of life Medical- Diagnosis and treatment Industrial- Food processing, Radiography, Gauges and measurement Research – Irradiation of samples, Calibration sources, tracers Agriculture- Tracer studies MEDICAL USES RADIOTHERAPY INTERVENTIONAL RADIOLOGY RADIO-PHARMACEUTICALS COMPUTED TOMOGRAPHY BLOOD/TISSUE IRRADIATOR INDUSTRIAL USES FOOD IRRADIATION INDUSTRIAL RADIOGRAPHY NUCLEONIC GAUGES RESEARCH TRACER STUDY IRRADIATION OF SAMPLES Department of Atomic Energy Atomic Department of Image courtesy: courtesy: Image Alexander L.- Polonium poisoning of Russian spy Atomic bomb survivors “RADIATION GOOGLE IS INDEED DISASTROUS” Image courtesy: socialistworld.net Image courtesy: courtesy: Image THE QUESTION TO ASK IS NOT "IS THERE ANY RADIOACTIVITY PRESENT?" BUT RATHER, "HOW MUCH, AND IS IT ENOUGH TO BE HARMFUL?" Atomic Energy Regulatory Board, Anushakti nagar Mumbai 10 Safety Research Institute at Kalpakkam Regional Centers at Chennai, New Delhi and Kolkata Effects Linear- Non Threshold model for Radiation AERB mandates in this area for safety DNA damage reduction CANCER RISK Epilation Erythema GI/ CNS Symptoms area for Prevention Prevention area for Death mandates in this AERB These effects are more profound in the foetus and children “Licence in accordance with Atomic Energy (Radiation Protection)Rules, 2004 from AERB is mandatory requirement for the procurement and use of radiation sources in India”. 12 Safety Research funding Safety in application of nuclear and radiation facilities Environmental Impact Assessment Transport of Radioactive material Radioactive Waste Management Civil and Structural Engineering Spent Fuel Storage Reactor Physics Thermal Hydraulics/Fluid Structure Interactions in Reactors under Accident Conditions . -

Fucus Gardneri Using Gamma-Ray Spectroscopy
Determination of 131I Uptake in Fucus Gardneri Using Gamma-Ray Spectroscopy Determination de 1'Accumulation de I dans Fucus Gardneri par Spectroscopie Gamma A thesis submitted to the Division of Graduate Studies of the Royal Military College of Canada By Kristine Margaret Mattson In Partial Fulfillment of the Requirements for the Degree of Master of Applied Science in Nuclear Engineering August 2011 © This thesis may be used within the Department of National Defence, but copyright for open publication remains the property of the author. Library and Archives Bibliotheque et Canada Archives Canada Published Heritage Direction du in Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington Ottawa ON K1A 0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-83402-2 Our file Notre reference ISBN: 978-0-494-83402-2 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, preter, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distrbute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriete du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette these. -

Industrial Radiography
RADIATION PROTECTION OF WORKERS Industrial Radiography RADIATION AND RADIOGRAPHS RADIOACTIVE SOURCES PROCEDURES RADIOGRAPHERS DO follow the procedures. Ionizing radiation can pen- Materials of higher den Sealed sources are small þ Safe storage Precautions þ DO use the appropriate equipment, including collimators. in size and contain material etrate objects and create sity absorb more radiation. þ DO confi rm that there are no other people working in the images on photographic The metal components are which emits penetrating area of radiography. fi lm. The technique is revealed inside this tele radiation continuously. Radioactive sources should be kept in a secure, fi re þ DO use clear working signs and signals. called radiography and phone because they have Special containers made þ DO set up the controlled area and the necessary barriers. the processed fi lms are absorbed more radiation of dense metal shielding resistant and adequately shielded storage location þ DO confi rm the location of the source, or that X rays are called radiographs. than the surrounding plastic. are necessary to store, not being generated, by use of a survey meter. when not in use, and should move and manipulate these þ DO secure and store the source or X ray machine when sources. Due to their small be kept separate from other not in use. materials. The storage loca- size and manoeuvrability, Portable and mobile radiographic þ DO wear your personal dosimeter. sealed sources can be containers. ~ tion for X ray machines that used in confined spaces. are not in use is not required to be shielded. OTHER WORKERS Iridium-192 is a common radioactive source used þ DO observe the access restrictions, however remote it may in gamma radiography.