Evidence of the Standing Committee on Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SCC File No.: in the SUPREME COURT of CANADA (ON APPEAL from the FEDERAL COURT of APPEAL) BETWEEN
SCC File No.: IN THE SUPREME COURT OF CANADA (ON APPEAL FROM THE FEDERAL COURT OF APPEAL) BETWEEN: AIR PASSENGER RIGHTS APPLICANT (Applicant) – and – CANADIAN TRANSPORTATION AGENCY RESPONDENT (Respondent) APPLICATION FOR LEAVE TO APPEAL (AIR PASSENGER RIGHTS, APPLICANT) (Pursuant to s. 40 of the Supreme Court Act, R.S.C. 1985, c. S-26 and Rule 25 of the Rules of the Supreme Court of Canada, SOR/2002-156) SIMON LIN Evolink Law Group 4388 Still Creek Drive, Suite 237 Burnaby, British Columbia, V5C 6C6 Tel: 604-620-2666 [email protected] Counsel for the Applicant, Air Passenger Rights ORIGINAL TO: THE REGISTRAR Supreme Court of Canada 301 Wellington Street Ottawa, ON K1A 0J1 COPIES TO: CANADIAN TRANSPORTATION AGENCY 15 Eddy Street, 17th Floor Gatineau, Quebec K1A 0N9 Allan Matte Tel: 819-994-2226 Fax: 819-953-9269 Email: [email protected] Email: Servicesjuridiques/LegalServicesOTC/CTA@otc- cta.gc.ca Counsel for the Respondent, Canadian Transportation Agency i TABLE OF CONTENTS 1. NOTICE OF APPLICATION FOR LEAVE TO APPEAL 1 JUDGMENTS BELOW 2. Reasons for Order of the Honourable Madam Justice Mactavish of the Federal Court of Appeal, dated May 22, 2020 5 3. Order of the Honourable Madam Justice Mactavish of the Federal Court of Appeal, dated May 22, 2020 20 4. Order of the Honourable Mr. Justice Boivin of the Federal Court of Appeal, dated May 1, 2020 22 5. Order of the Honourable Mr. Justice Locke of the Federal Court of Appeal, dated April 16, 2020 24 6. Order of the Honourable Mr. Justice Pelletier of the Federal Court of Appeal, dated April 9, 2020 28 7. -

Mass Cancellations Put Artists' Livelihoods at Risk; Arts Organizations in Financial Distress
Prime Minister Justin Trudeau March 17, 2020 Deputy Prime Minister Chrystia Freeland The Honourable Steven Guilbeault The Honourable William Francis Morneau Minister of Canadian Heritage Minister of Finance The Honourable Mona Fortier The Honourable Navdeep Bains Minister of Middle-Class Prosperity Minister of Innovation, Science and Industry Associate Minister of Finance The Honourable Mélanie Joly Minister of Economic Development and Official Languages Re: Mass cancellations put artists’ livelihoods at risk; arts organizations in financial distress Dear Prime Minister Trudeau; Deputy Prime Minister Freeland; and Ministers Guilbeault, Morneau, Fortier, Joly, and Bains, We write as the leadership of Opera.ca, the national association for opera companies and professionals in Canada. In light of recent developments around COVID-19 and the waves of cancellations as a result of bans on mass gatherings, Opera.ca is urgently requesting federal aid on behalf of the Canadian opera sector and its artists -- its most essential and vulnerable people -- while pledging its own emergency support for artists in desperate need. Opera artists are the heart of the opera sector, and their economic survival is in jeopardy. In response to the dire need captured by a recent survey conducted by Opera.ca, the board of directors of Opera.ca today voted for an Opera Artists Emergency Relief Fund to be funded by the association. Further details will be announced shortly. Of the 14 professional opera companies in Canada, almost all have cancelled their current production and some the remainder of the season. This is an unprecedented crisis with long-reaching implications for the entire Canadian opera sector. -
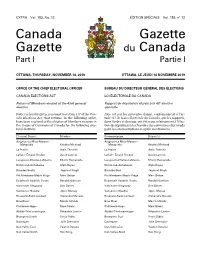
Canada Gazette, Part I
EXTRA Vol. 153, No. 12 ÉDITION SPÉCIALE Vol. 153, no 12 Canada Gazette Gazette du Canada Part I Partie I OTTAWA, THURSDAY, NOVEMBER 14, 2019 OTTAWA, LE JEUDI 14 NOVEMBRE 2019 OFFICE OF THE CHIEF ELECTORAL OFFICER BUREAU DU DIRECTEUR GÉNÉRAL DES ÉLECTIONS CANADA ELECTIONS ACT LOI ÉLECTORALE DU CANADA Return of Members elected at the 43rd general Rapport de député(e)s élu(e)s à la 43e élection election générale Notice is hereby given, pursuant to section 317 of the Can- Avis est par les présentes donné, conformément à l’ar- ada Elections Act, that returns, in the following order, ticle 317 de la Loi électorale du Canada, que les rapports, have been received of the election of Members to serve in dans l’ordre ci-dessous, ont été reçus relativement à l’élec- the House of Commons of Canada for the following elec- tion de député(e)s à la Chambre des communes du Canada toral districts: pour les circonscriptions ci-après mentionnées : Electoral District Member Circonscription Député(e) Avignon–La Mitis–Matane– Avignon–La Mitis–Matane– Matapédia Kristina Michaud Matapédia Kristina Michaud La Prairie Alain Therrien La Prairie Alain Therrien LaSalle–Émard–Verdun David Lametti LaSalle–Émard–Verdun David Lametti Longueuil–Charles-LeMoyne Sherry Romanado Longueuil–Charles-LeMoyne Sherry Romanado Richmond–Arthabaska Alain Rayes Richmond–Arthabaska Alain Rayes Burnaby South Jagmeet Singh Burnaby-Sud Jagmeet Singh Pitt Meadows–Maple Ridge Marc Dalton Pitt Meadows–Maple Ridge Marc Dalton Esquimalt–Saanich–Sooke Randall Garrison Esquimalt–Saanich–Sooke -
Debates of the House of Commons
43rd PARLIAMENT, 2nd SESSION House of Commons Debates Official Report (Hansard) Volume 150 No. 117 Monday, June 14, 2021 Speaker: The Honourable Anthony Rota CONTENTS (Table of Contents appears at back of this issue.) 8309 HOUSE OF COMMONS Monday, June 14, 2021 The House met at 11 a.m. [English] NATIONAL STRATEGY FOR A GUARANTEED BASIC INCOME ACT Prayer Ms. Julie Dzerowicz (Davenport, Lib.) moved that Bill C-273, An Act to establish a national strategy for a guaranteed basic in‐ come, be read the second time and referred to a committee. PRIVATE MEMBERS' BUSINESS She said: Mr. Speaker, I am absolutely honoured to rise in the ● (1105) House today to speak to my private member's bill, Bill C-273, an [Translation] act to establish a national strategy for a guaranteed basic income. I give my thanks to the member for Malpeque, who seconded the bill The Speaker: The Chair would like to take a moment to provide and is a champion for a guaranteed basic income pilot in his home some information to the House regarding the management of Pri‐ province of P.E.I., and to the member for Beaches—East York, a vate Members' Business. true progressive who traded his spot so I could stand in the House today to begin second reading of Bill C-273. I feel blessed to call As members know, certain procedural realities constrain the him a colleague and friend. Speaker and members insofar as legislation is concerned. [English] Basic income is not a new idea. It is one that has been circulating in Canada for decades. -

Evidence of the Standing Committee on Canadian
43rd PARLIAMENT, 2nd SESSION Standing Committee on Canadian Heritage EVIDENCE NUMBER 036 Wednesday, May 19, 2021 Chair: Mr. Scott Simms 1 Standing Committee on Canadian Heritage Wednesday, May 19, 2021 ● (1430) That's all I wanted to say. [English] The Chair: Mr. Rayes. The Chair (Mr. Scott Simms (Coast of Bays—Central—Notre [Translation] Dame, Lib.)): I call this meeting to order. Mr. Alain Rayes (Richmond—Arthabaska, CPC): Thank you, Welcome to meeting number 36 of the House of Commons Mr. Chair. Standing Committee on Canadian Heritage. I would like to ask the committee something. I don't know Pursuant to the order of reference of February 16 and the motion whether it is in keeping with procedure, but I am sure you could en‐ adopted by the committee on Monday, May 10, the committee re‐ lighten me. sumes consideration of Bill C-10, an act to amend the Broadcasting Act and to make related and consequential amendments to other We have met a number of times over the past few weeks. Clearly, acts. the committee came to an impasse after the initially proposed sec‐ tion 4.1 was deleted. We had an opportunity to hear from expert As I mentioned earlier, when we left we were with G-11.1. witnesses, following our unanimous decision to summon them. We I see there is a great deal of interest on the board. There are even had an opportunity to hear from both ministers. The Minister hands up. of Justice produced the requested document. Is it the minister's statement or an explanatory document? We do not agree on this. -

63 Priority Districts for 2019
63 Priority Districts for 2019 These Federal Electoral Districts were the ones in which the 2016 Census Population of First Nations 18+ was either: a) larger than the margin of victory in the 2015 federal election b) within 5% of the margin of victory and at least 1% of the total vote eligible population in the district Legend Underline indicates previous winner (If only the party is underlined the incumbent is not running) Bold Candidates Indicates a First Nations Candidate FN 18+ = Total number of First Nations Eligible Voters MOV = Margin of Victory in total votes in 2015 1 Alberta (Five Districts) 5. Edmonton Mill Woods (Click for Map of District) 1. Calgary Confederation (Click for Map of District) Candidates: Candidates: CPC Tim Uppal GRN Tanya Herbert CPC Len Webber LIB Amarjeet Sohi GRN Natalie AM Odd NDP Nigel Logan LIB Jordan Stein PPC Annie Young NDP Gurcharan Sidhu[ PPC Colin C. Korol FN 18+: 1230 MOV: 92 FN 18+: 1095 MOV: 1586 2. Calgary Centre (Click for Map of District) Candidates: CPC Gary McLean GRN Thana Boolert LIB Kent Hehr NDP essica Buresi PPC Chevy Johnston FN 18+: 1110 MOV: 750 3. Edmonton Centre (Click for Map of District) Candidates: CPC James Cumming GRN Grad Murray LIB Randy Boissonnault NDP Katherine Swampy PPC Paul J. Hookham FN 18+: 2800 MOV: 1199 4. Edmonton Griesbach (Click for Map of District) Candidates: CPC Kerry Diotte GRN Safi Khan LIB Habiba Mohamud NDP Mark W.J. Cherington PPC Barbara Nichols FN 18+: 3465 MOV: 2848 2 British Columbia (15 Districts) 1. Burnaby South (Click for Map of District) 5. -

Vaccine Rollout in Canada
January 12, 2021 Hon. Patty Hajdu Hon. Marc Miller Minister of Health Minister of Indigenous Services House of Commons House of Commons Ottawa, ON K1A 0A6 Ottawa, ON K1A 0A6 Ministers Hajdu and Miller, We are writing to you on behalf of the Canadian Paediatric Society (CPS) and our membership of paediatric health experts across the country to urge you to accelerate the administration of COVID-19 vaccines across Canada. Along with our colleagues in family medicine, geriatrics, nursing, and countless other health professionals, we celebrated when Health Canada announced safe and effective vaccines were approved for use in Canada. But the rollout of the largest vaccination campaign in history has started off far too slow. Indigenous communities where COVID-19 infection can have disproportionate impact need vaccines now. Our frontline healthcare workers, who have been risking their lives to care for Canadians since the start of this pandemic, and Canada’s most vulnerable, especially our elders and those living in long-term care homes, cannot afford to continue waiting. There is another group of Canadians whose lives depend on widespread vaccine coverage—children and youth. Since the start of the pandemic, children and youth have been disproportionately affected by the public health measures designed to keep Canadians safe from COVID-19. We are especially concerned about the effects these restrictions have had on their mental health. It may be years before we fully understand the extent and magnitude of these effects, but here is what we know right now: Paediatricians, child and adolescent psychiatrists, and other health professionals are seeing more youth with mental health problems, including anxiety, depression, eating disorders, and problematic substance use. -

Evidence of the Special Committee on the COVID-19 Pandemic
43rd PARLIAMENT, 1st SESSION Special Committee on the COVID-19 Pandemic EVIDENCE NUMBER 015 Tuesday, June 2, 2020 Chair: The Honourable Anthony Rota 1 Special Committee on the COVID-19 Pandemic Tuesday, June 2, 2020 ● (1200) Right Hon. Justin Trudeau (Papineau, Lib.): Thank you, [Translation] Mr. Chair. The Acting Chair (Mr. Bruce Stanton (Simcoe North, CPC)): Honourable members, I call this meeting to order. [English] Welcome to the 15th meeting of the House of Commons Special I rise today to address what so many people of colour live with Committee on the COVID‑19 Pandemic. This will be a hybrid every day. meeting. Members will be participating via video conference or in person. Over the past few days, we've seen horrific reports of police vio‐ [English] lence against black men and women south of the border, but these are not isolated incidents or “elsewhere” problems. Prejudice, dis‐ I will remind you that in order to avoid issues with sound, mem‐ crimination and violence are a lived reality for far too many people. bers participating in person should not also be connecting by video They are a result of systems that far too often condone, normalize, conference. In order to ensure that those joining the meeting via perpetrate and perpetuate inequality and injustice against people of video conference can be seen and heard by those in the chamber, colour. two screens have been set up here on either side of the Speaker's chair, and members in the chamber can listen to the floor audio or to interpretation using the earpieces on their desks. -

We Put This Together for You and We're Sending It to You Early
Exclusively for subscribers of The Hill Times We put this together for you and we’re sending it to you early. 1. Certified election 2019 results in all 338 ridings, top four candidates 2. The 147 safest seats in the country 3. The 47 most vulnerable seats in the country 4. The 60 seats that flipped in 2019 Source: Elections Canada and complied by The Hill Times’ Samantha Wright Allen THE HILL TIMES | MONDAY, NOVEMBER 11, 2019 13 Election 2019 List Certified 2019 federal election results 2019 2019 2019 2019 2019 2019 Votes Votes% Votes Votes% Votes Votes% ALBERTA Edmonton Riverbend, CPC held BRITISH COLUMBIA Banff-Airdrie, CPC held Matt Jeneroux, CPC 35,126 57.4% Tariq Chaudary, LPC 14,038 23% Abbotsford, CPC held Blake Richards, CPC 55,504 71.1% Ed Fast, CPC 25,162 51.40% Audrey Redman, NDP 9,332 15.3% Gwyneth Midgley, LPC 8,425 10.8% Seamus Heffernan, LPC 10,560 21.60% Valerie Kennedy, GRN 1,797 2.9% Anne Wilson, NDP 8,185 10.5% Madeleine Sauvé, NDP 8,257 16.90% Austin Mullins, GRN 3,315 4.2% Stephen Fowler, GRN 3,702 7.60% Edmonton Strathcona, NDP held Battle River-Crowfoot, CPC held Heather McPherson, NDP 26,823 47.3% Burnaby North-Seymour, LPC held Sam Lilly, CPC 21,035 37.1% Damien Kurek, CPC 53,309 85.5% Terry Beech, LPC 17,770 35.50% Eleanor Olszewski, LPC 6,592 11.6% Natasha Fryzuk, NDP 3,185 5.1% Svend Robinson, NDP 16,185 32.30% Michael Kalmanovitch, GRN 1,152 2% Dianne Clarke, LPC 2,557 4.1% Heather Leung, CPC 9,734 19.40% Geordie Nelson, GRN 1,689 2.7% Amita Kuttner, GRN 4,801 9.60% Edmonton West, CPC held Bow River, CPC held -

LOBBY MONIT R the 43Rd Parliament: a Guide to Mps’ Personal and Professional Interests Divided by Portfolios
THE LOBBY MONIT R The 43rd Parliament: a guide to MPs’ personal and professional interests divided by portfolios Canada currently has a minority Liberal government, which is composed of 157 Liberal MPs, 121 Conservative MPs, 32 Bloc Québécois MPs, 24 NDP MPs, as well as three Green MPs and one Independent MP. The following lists offer a breakdown of which MPs have backgrounds in the various portfolios on Parliament Hill. This information is based on MPs’ official party biographies and parliamentary committee experience. Compiled by Jesse Cnockaert THE LOBBY The 43rd Parliament: a guide to MPs’ personal and professional interests divided by portfolios MONIT R Agriculture Canadian Heritage Children and Youth Education Sébastien Lemire Caroline Desbiens Kristina Michaud Lenore Zann Louis Plamondon Martin Champoux Yves-François Blanchet Geoff Regan Yves Perron Marilène Gill Gary Anandasangaree Simon Marcil Justin Trudeau Claude DeBellefeuille Julie Dzerowicz Scott Simms Filomena Tassi Sean Casey Lyne Bessette Helena Jaczek Andy Fillmore Gary Anandasangaree Mona Fortier Lawrence MacAulay Darrell Samson Justin Trudeau Harjit Sajjan Wayne Easter Wayne Long Jean-Yves Duclos Mary Ng Pat Finnigan Mélanie Joly Patricia Lattanzio Shaun Chen Marie-Claude Bibeau Yasmin Ratansi Peter Schiefke Kevin Lamoureux Francis Drouin Gary Anandasangaree Mark Holland Lloyd Longfield Soraya Martinez Bardish Chagger Pablo Rodriguez Ahmed Hussen Francis Scarpaleggia Karina Gould Jagdeep Sahota Steven Guilbeault Filomena Tassi Kevin Waugh Richard Lehoux Justin Trudeau -

O'toole Ahead, Lewis Gaining for Conservative Leader
Your community... your newspaper! Call 1-844-GNG-NEWS (ext. 222) to renew or subscribe today. THE MELVILLE $1.50 PER COPYCOPY Friday,Friday, GST INCLUDEDINCLUDED JJulyuly 10, 20220200 Vol.Vol. 94 No. 2727 AgreementAgreement # 4001192240011922 PROUDLYPRROUUDDLY SERVINGSESERRVINNG MELVILLEMMELVILLE ANDAND SURROUNDINGSURROUNDING AREAAREA SINCESISINCN E 19291929 • WWW.GRASSLANDSNEWS.CAWWWW .G. RAASSSSLAL NDSNEWS.CA • 1-306-728-54481-306-728-5448 DemolitionD liti dropd CHRISCCHRISSSAS ASHFIELDHFIELD | GRASSLANDSGGRASSSSLANDSS NEWS Demolition of the old water treatment plant in Melville continues and last week crews were using a wrecking ball to break up material to haul it away. The demolition, which began in June, is expected to be completed later this month. There are no water interruptions expected due to the demolition of the facility but access to the water treatment plant has been limited and restricted. O’Toole ahead, Lewis gaining for Conservative leader By Alan Hustak try as a legal analyst. I under- during the last election. Crit- candidates, better than those Grasslands News stand the resource economy,” ics claim MacKay sat out the who have announced,” he told he said.” campaign and did Scheer no Grasslands. There are voters Souris Moose-Mountain favours by complaining that who remain loyal Scheer’ sup- Erin O’Toole appears to have MP Robert Kitchen supported the opposition leader failed porters. “I like Andrew. He’s a the edge among Saskatchewan’s O’Toole in the last leadership to inspire voters. “He missed nice guy,” said Petri Keppo“- voting delegates in the race to race, in which he finished third, the open net on a breakaway,” Conservatives need a fighter, replace Andrew Scheer as Con- and is backing him again. -

Workplace 3.0?
Bad + New book Workplace 3.0? Bitchy captures p. 10 cartoonist’s art of political critique Public service could shift to Andrew home office for the long haul p. 4 Caddell p. 9 Parties of the past p. 21 THIRTY-FIRST YEAR, NO. 1727 CANADA’S POLITICS AND GOVERNMENT NEWSPAPER WEDNESDAY, MAY 13, 2020 $5.00 News Procurement News Conservatives & Quebec Quebec CPC ‘Hard decisions are going to membership votes more have to be made’: can vital important than low leadership defence procurements survive donations, say politicos in a post-pandemic world? BY SAMANTHA WRIGHT ALLEN ll four Conservative leader- Lockheed Martin's Aship hopefuls have reported ‘When you are F-35, pictured, is low fundraising numbers in one of three potential Quebec to start the year, amount- trying to fix a fiscal options that could ing to three per cent of all funds problem, inevitably replace Canada's raised this race in a province that fleet of CF-18s with will be key to the next leaders’ national defence 88 new fighter jets. coronation. That doesn’t mean The procurement they aren’t active and recruiting is part of the way process for the new support in Quebec, suggest some governments planes has already Conservative politicians, who say been delayed by the membership, not money, is most have tended to ongoing coronavirus important, with donors distracted pandemic. Photograph by COVID-19, fatigued by repeat try and fix that,’ courtesy of Wikimedia says defence Commons Continued on page 16 procurement expert David Perry. News Conservative leadership BY NEIL MOSS years to come, questions remain defence procurement projects 15 new warships that will serve on how the COVID-19 pandemic with another delay in the replace- as the backbone of the Canadian Experienced n the midst of critical procure- will affect the oft-delayed projects.