ICD-10-CM Diagnosis Codes RELATED to HEARING and VESTIBULAR DISORDERS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assessment of Bone Conduction Thresholds After Surgical Treatment in Patients with Labyrinthine Fistula
Turkish Archives of Otorhinolaryngology Turk Arch Otorhinolaryngol 2018; 56(2): 89-94 89 Türk Otorinolarengoloji Arşivi Assessment of Bone Conduction Thresholds After Surgical Treatment in Patients with Labyrinthine Fistula Müzeyyen Yıldırım Baylan1 , Ümit Yılmaz1 , Zeki Akkuş2 , İsmail Topçu1 1Department of Otorhinolaryngology, Dicle University School of Medicine, Diyarbakır, Turkey Original Investigation 2Department of Biostatistics, Dicle University School of Medicine, Diyarbakır, Turkey Abstract Objective: This study aimed to analyze the bone con- years. In the post-operative period, it was possib- duction thresholds before and after surgery in chronic le to conduct audiological follow-up on 20 patients. otitis media patients with cholesteatoma who had In these follow-ups, 16 patients showed no change labyrinthine fistula and whose cholesteatoma matrix in bone conduction thresholds, two patients showed had been completely cleaned. worsening, and two showed improvement. When Methods: The study was performed between 2013 pre- and post-operative bone conduction thresholds to 2017 with 23 chronic otitis media patients who at each frequency were compared separately, no sig- had labyrinthine fistula with cholesteatoma and who were operated at the Department of Otorhinolar- nificant difference was found (p=0.937). No statis- yngology of Dicle University School of Medicine. tically significant difference was found between the Patients were assessed by anamnesis and examina- pre- and post-operative means at the four frequencies tion and when necessary, by temporal computerized (p=0.712). tomography and diffusion magnetic resonance ima- Conclusion: In this study, we found that to reduce ging. Bone conduction thresholds at frequencies of complications relating to cholesteatoma, it might be 500, 1000, 2000, and 4000 Hz were determined by audiometric examination and they were compared necessary to completely remove the matrix especially before and after surgery. -

Common Urgent ENT Problems APRIL 4, 2019 GERARD MACDONALD MD FRCS
3/21/2019 Common Urgent ENT Problems APRIL 4, 2019 GERARD MACDONALD MD FRCS 1 Course Objectives A review of common Urgent ENT problems presenting to office and ER Clinical Pearls to help you manage in a timely fashion Knowing when to refer 2 1 3/21/2019 I do not have any Conflicts of Interest 3 Top Ten List Of Urgent Calls 1.Acute Otitis Externa 2. Sudden Hearing Loss 3.Facial Palsy 4.Salivary Gland Stone /Infection 5.Peritonsillar Abscess 6.Neck Abscess 7.Nosebleeds 8.Hoarseness 9.Foreign Bodies Ear/Nose 10. Acute Vertigo 4 2 3/21/2019 Acute Otitis Externa Commonly associated with swimming ( swimmer’s ear) Common in diabetics and habitual Q-tip Users Usual presenting symptoms are itching, discharge, pain and swelling. More severe symptoms can include severe pain, parotid swelling,trismus and cellulitiis Most common organism is Pseudomonas Aeruginosa May go on to develop secondary otomycosis if frequent use of topical antibiotics. Malignant External Otitis rare but serious 5 Acute Otitis Externa 6 3 3/21/2019 Acute Otitis Externa - Treatment Debridement/Suctioning ? Culture Avoid syringing Ototopicals : Tobradex, Sofracort, Ciprodex Otowick if canal swollen shut Oral Antibiotic ( Cipro ) and single dose Steroid if severe When to refer : Unrelenting pain and swelling, facial nerve weakness,dysphagia , fever 7 Sudden hearing Loss UNEXPLAINED sudden sensorineural hearing loss occurring over 3 days Not AOM, trauma, acoustic trauma , ototoxicity Often confused with ETD , “fluid” Poorer outcome if not recognized -

A Brief Evaluation and Image Formation of Pediatrics Nutritional Forum in Opinion Sector Disouja Wills* Nutritonal Sciences, Christian Universita Degli Studo, Italy
d Pediatr Wills, Matern Pediatr Nutr 2016, 2:2 an ic l N a u n t DOI: 10.4172/2472-1182.1000113 r r e i t t i o Maternal and Pediatric a n M ISSN: 2472-1182 Nutrition ShortResearch Commentary Article OpenOpen Access Access A Brief Evaluation and Image formation of Pediatrics Nutritional Forum in Opinion Sector Disouja Wills* Nutritonal Sciences, Christian Universita degli studo, Italy Abstract Severe most and one of the main global threat is Nutritional disorders to backward countries, with respect to this issue WHO involved and trying to overcome this issue with the Co-ordination of INF and BNF. International Nutrition Foundation and British Nutrition Foundation, development in weight gain through proper nutrition and proper immune mechanism in the kids is their main role to eradicate and overcome nutritional problems in world. Keywords: INF; BNF; Malnutrition; Merasmus; Rickets; Weight loss; Precautions to Avoid Nutrition Deficiency in Paediatric health issue Paediatrics Introduction Respective disease having respective deficiency dis order but in the case of nutritional diseases. Proper nutrition is the only thing to cure In the mankind a respective one health and weight gain is fully nutritional disorders. Providing sufficient diet like fish, meat, egg, milk based on perfect nutritional intake which he is having daily, poor diet to malnourished kids and consuming beef, fish liver oil, sheep meat, will show the improper impact and injury to the some of the systems boiled eggs from the age of 3 itself (Tables 1 and 2). in the body, total health also in some times. Blindness, Scurvy, Rickets will be caused by nutritional deficiency disorders only, mainly in kids. -

Definitions and Background
1 Definitions and Background Tinnitus is a surprisingly complex subject. Numer- ears.” And, in fact, the word “tinnitus” is derived ous books would be required to adequately cover the from the Latin word tinniere, which means “to current body of knowledge. The present handbook ring.” Patients report many different sounds—not focuses on describing procedures for providing just ringing—when describing the sound of their clinical services for tinnitus using the methodology tinnitus, as we discuss later in this chapter. of progressive tinnitus management (PTM). In this opening chapter we establish common ground with respect to terminology and contextual Transient Ear Noise information. Relevant definitions are provided, many of which are operational due to lack of consensus It seems that almost everyone experiences “tran- in the field. Additional background information sient ear noise,” which typically is described as a includes brief descriptions of epidemiologic data, sudden whistling sound accompanied by the per- patient data, and conditions related to reduced tol- ception of hearing loss (Kiang, Moxon, & Levine, erance (hypersensitivity) to sound. 1970). No systematic studies have been published to date describing the prevalence and properties of transient ear noise; thus, anything known about Basic Concepts and Terminology this phenomenon is anecdotal. The transient auditory event is unilateral and seems to occur completely at random without any- Tinnitus is the experience of perceiving sound that thing precipitating the sudden onset of symptoms. is not produced by a source outside of the body. The Often the ear feels blocked during the episode. The “phantom” auditory perception is generated some- symptoms generally dissipate within a period of where in the auditory pathways or in the head or about a minute. -
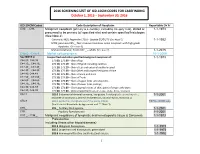
2016 SCREENING LIST of ICD-10CM CODES for CASEFINDING October 1, 2015 – September 30, 2016
2016 SCREENING LIST OF ICD-10CM CODES FOR CASEFINDING October 1, 2015 – September 30, 2016 ICD-10-CM Codes Code Description of Neoplasm Reportable Dx Yr C00._- C96._ Malignant neoplasm (primary & secondary; excluding category C44), stated or 1-1-1973 presumed to be primary (of specified site) and certain specified histologies (See Note 2) Carcinoid, NOS; Appendix C18.0 - Update 01/01/15 (See Note 5) 1-1-1992 MCN; pancreas C25._; Non-invasive mucinous cystic neoplasm with high grade dysplasia. (See note 6) Mature teratoma; Testis C62._ – adults (See note 7) 1-1-2015 C4a.0_-C4a.9_ Merkel cell carcinoma 10-1-2009 See NOTE 4 Unspecified and other specified malignant neoplasm of : 1-1-1973 C44.00.-C44.09 173.00, 173.09 – Skin of Lip C44.10_, C44.19_ 173.10, 173.19 – Skin of Eyelid including canthus C44.20_, C44.29_ 173. 20, 173.29 – Skin of Ear and external auditory canal C44.30_, C44.39_ 173.30, 173.39 – Skin Other and unspecified parts of face C44.40, C44.49 173. 40, 173.49 – Skin of Scalp and neck C44.50_, C44.59_ 173.50, 173.59 – Skin of Trunk C44.60_, C44.69_ 173. 60, 173.69 – Skin of Upper limb and shoulder, C44.70_, C44.79_ 173.70, 173.79 – Skin of Lower limb and hip; C44.80, C44.89 173.80, 173.89 – Overlapping lesions of skin, point of origin unknown; C44.90, C44.99 173.90, 173.99 - Sites unspecified (excludes Labia, Vulva, Penis, Scrotum) C54.1 182.0 Endometrial stromal sarcoma, low grade; Endolymphatic stromal myosis ; 1-1-2001 Endometrial stromatosis, Stromal endometriosis, Stromal myosis, NOS (C54.1) C56.9 183.0 Borderline malignancies -

Noise-Induced Cochlear Neuronal Degeneration and Its Role in Hyperacusis- and Tinnitus-Like Behavior
Noise-Induced Cochlear Neuronal Degeneration and Its Role in Hyperacusis- and Tinnitus-Like Behavior by Ann E. Hickox B.A. French Arizona State University, 2006 MSc Speech and Hearing Sciences University College London, 2007 SUBMITTED TO THE HARVARD-MIT DIVISION OF HEALTH SCIENCES AND TECHNOLOGY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY IN SPEECH AND HEARING BIOSCIENCE AND TECHNOLOGY AT THE MASSACHUSETTS INSTITUTE OF TECHNOLOGY FEBRUARY 2013 @2013 Ann E. Hickox. All rights reserved The author hereby grants to MIT permission to reproduce and to distribute publicly paper and electronic copies of this thesis document in whole or in part in any medium now known or hereafter created. Signature of Author: Ann E. Hickox Harvard-MIT Division of e lthSciences and Technology f/ / I / January 2, 2013 Certified by: M. Charles Liberman, Ph.D. Thesis Supervisor Director, Eaton-Peabody Laboratory, Massachusetts Eye & Ear Infirmary Harold F. Schuknecht Professor of Otology and Laryngology, Harvard Medical School Accepted by Emery Brown, MD, PhD Director, Harvard-MIT Division of Health Sciences and Technology Professor of Computational Neuroscience and Health Sciences and Technology 1 2 Noise-Induced Cochlear Neuronal Degeneration and Its Role in Hyperacusis- and Tinnitus-Like Behavior by Ann E. Hickox Submitted to the Harvard-MIT Division of Health Sciences and Technology on January 2, 2013 in partial fulfillment of the requirements for the Degree of Doctor of Philosophy in Speech and Hearing Bioscience and Technology Abstract Perceptual abnormalities such as hyperacusis and tinnitus often occur following acoustic overexposure. Although such exposure can also result in permanent threshold elevation, some individuals with noise-induced hyperacusis or tinnitus show clinically normal thresholds. -

BMC Ear, Nose and Throat Disorders Biomed Central
BMC Ear, Nose and Throat Disorders BioMed Central Case report Open Access Acute unilateral hearing loss as an unusual presentation of cholesteatoma Daniel Thio*1, Shahzada K Ahmed2 and Richard C Bickerton3 Address: 1Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK, 2Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK and 3Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK Email: Daniel Thio* - [email protected]; Shahzada K Ahmed - [email protected]; Richard C Bickerton - [email protected] * Corresponding author Published: 18 September 2005 Received: 10 July 2005 Accepted: 18 September 2005 BMC Ear, Nose and Throat Disorders 2005, 5:9 doi:10.1186/1472-6815-5-9 This article is available from: http://www.biomedcentral.com/1472-6815/5/9 © 2005 Thio et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Cholesteatomas are epithelial cysts that contain desquamated keratin. Patients commonly present with progressive hearing loss and a chronically discharging ear. We report an unusual presentation of the disease with an acute hearing loss suffered immediately after prolonged use of a pneumatic drill. Case presentation: A 41 year old man with no previous history of ear problems presented with a sudden loss of hearing in his right ear immediately following the prolonged use of a pneumatic drill on concrete. -

Acoustic Trauma and Hyperbaric Oxygen Treatment
Acoustic Trauma and Hyperbaric Oxygen Treatment Mesut MUTLUOGLU Department of Underwater and Hyperbaric Medicine Gulhane Military Medical Academy Haydarpasa Teaching Hospital 34668, Uskudar, Istanbul TURKEY [email protected] ABSTRACT As stated in the conclusions of the HFM-192 report on hyperbaric oxygen therapy (HBOT) in military medical setting, acoustic trauma is a frequent consequence of military activity in operation. Acoustic trauma refers to an acute hearing loss following a single sudden and very intense noise exposure. It differs from chronic noise induced hearing (NIHL) loss in that it is usually unilateral and causes sudden profound hearing loss. Acoustic trauma is a type of sensorineural hearing loss affecting inner ear structures; particularly the inner and outer hair cells of the organ of Corti within the cochlea. Exposure to noise levels above 85 decibel (dB) may cause hearing loss. While long-term exposure to repetitive or continuous noise above 85 dB may cause chronic NIHL, a single exposure above 130-140 dB, as observed in acoustic trauma, may cause acute NIHL. The loudest sound a human ear may tolerate without pain varies individually, but is usually around 120dB. Military personnel are especially at increased risk for acoustic trauma due to fire arm use in the battle zone. While a machine gun generates around 145dB sound, a rifle generates 157- 163dB, a 105 mm towed howitzer 183dB and an improvised explosive device around 180dB sound. Acoustic trauma displays a gradually down-slopping pattern in the audiogram, particularly after 3000Hz and is therefore described as high-frequency hearing loss. Tinnitus is almost always associated with acoustic trauma. -

Cholesteatoma Handout
Cholesteatoma Handout A cholesteatoma is a skin growth that occurs in an abnormal location, usually in the middle ear space behind the eardrum. It often arises from repeated or chronic infection, which causes an in-growth of the skin of the eardrum. Cholesteatomas often take the form of a cyst or pouch that sheds layers of old skin that build up inside the ear. Over time, the cholesteatoma can increase in size and destroy the surrounding delicate bones of the middle ear. Hearing loss, dizziness, and facial muscle paralysis are rare but can result from continued cholesteatoma growth. What are the symptoms? Initially, the ear may drain fluid, sometimes with a foul odor. As the cholesteatoma pouch or sac enlarges, it can cause a full feeling or pressure in the ear, along with hearing loss. Dizziness, or muscle weakness on one side of the face can also occur. Is it dangerous? Ear cholesteatomas can be dangerous and should never be ignored. Bone erosion can cause the infection to spread into the surrounding areas, including the inner ear and brain. If untreated, deafness, brain abscess, meningitis, and rarely death can occur. What treatment can be provided? Initial treatment may consist of a careful cleaning of the ear, antibiotics, and ear drops. Therapy aims to stop drainage in the ear by controlling the infection. The extent or growth characteristics of a cholesteatoma must then be evaluated. Cholesteatomas usually require surgical treatment to protect the patient from serious complications. Hearing and balance tests and CT scans of the ear may be necessary. These tests are performed to determine the hearing level remaining in the ear and the extent of destruction the cholesteatoma has caused. -

ICD-9/10 Mapping Spreadsheet
ICD-9-CM to ICD-10-CM Mappings for Audiology Related Disorders Updated 7/16/2015 Disclaimer: This product is NOT comprehensive and consists only of codes commonly related to audiology services. Mappings are only to ICD-10-CM codes, not ICD-10-PCS. Every effort was made to accurately map codes using detailed analysis. Keep in mind, however, that while many codes in ICD-9-CM map directly to codes in ICD-10, in some cases, additional clinical analysis may be required to determine which code or codes should be selected for your situation. Always review mapping results before applying them. ICD-9-CM ICD-9-CM Description ICD-10- ICD-10-CM Description Notes Code CM Code 315.32 Mixed receptive-expressive F80.2 Mixed receptive-expressive language language disorder disorder Central auditory processing Developmental dysphasia or aphasia, disorder receptive type Developmental Wernicke's aphasia Excludes1: central auditory processing disorder (H93.25), dysphasia or aphasia NOS (R47.-), expressive language disorder (F80.1), expressive type dysphasia or aphasia (F80.1), word deafness (H93.25) Excludes2: acquired aphasia with epilepsy [Landau-Kleffner] (G40.80-), pervasive developmental disorders (F84.-), selective mutism (F94.0), intellectual disabilities (F70-F79) H93.25 Central auditory processing disorder Congenital auditory imperception Word deafness Excludes1: mixed receptive-epxressive language disorder (F80.2) 380.00 Perichondritis of pinna, unspecified H61.001 Unspecified perichondritis of right external ear H61.002 Unspecified perichondritis -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence
3 Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence Various types of apheresis procedures have paucity of high-quality research, conclusions been performed on a clinical basis for many years, about the safety, efficacy, and effectiveness of but the number of patients and types of diseases apheresis are necessarily limited, although some treated have risen significantly in the last 5 years. tentative conclusions and directions for treatment This increase is partially due to increased under- can be discerned. standing of the disease and partially due to engi- The present chapter analyzes the methodolog- neering advances in equipment technologies. By ical problems in conducting apheresis research and almost any standard, treatment by apheresis is still examines available evidence of the safety, ef- in relatively early stages of development—there ficacy, and effectiveness of apheresis. Following are no ideal protocols based on a thorough un- a discussion of methodological issues, several derstanding of reasons for its efficacy. Never- major reviews of apheresis research will be sum- theless, there is an increasing flow of clinical data, marized and evaluated. This chapter will further sometimes describing dramatic patient improve- include the findings of a primary literature review ment, supporting the view that apheresis is a and assessment of apheresis in the treatment of rapidly emerging technology with significant three diseases—namely, hemolytic uremic syn- promise (117). Such evidence of treatment effec- drome, acquired Factor-VIII inhibitor, and Guil- tiveness’ is even today, however, often based on lain-Barré syndrome— where preliminary reports unsystematically collected data.