Unicompartmental Knee Replacement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arthroscopy - Orthoinfo - AAOS 6/10/12 3:40 PM
Arthroscopy - OrthoInfo - AAOS 6/10/12 3:40 PM Copyright 2010 American Academy of Orthopaedic Surgeons Arthroscopy Arthroscopy is a surgical procedure orthopaedic surgeons use to visualize, diagnose, and treat problems inside a joint. The word arthroscopy comes from two Greek words, "arthro" (joint) and "skopein" (to look). The term literally means "to look within the joint." In an arthroscopic examination, an orthopaedic surgeon makes a small incision in the patient's skin and then inserts pencil-sized instruments that contain a small lens and lighting system to magnify and illuminate the structures inside the joint. Light is transmitted through fiber optics to the end of the arthroscope that is inserted into the joint. By attaching the arthroscope to a miniature television camera, the surgeon is able to see the interior of the joint through this very small incision rather than a large incision needed for surgery. The television camera attached to the arthroscope displays the image of the joint on a television screen, allowing the surgeon to look, for example, throughout the knee. This lets the surgeon see the cartilage, ligaments, and under the kneecap. The surgeon can determine the amount or type of injury and then repair Here are parts of the shoulder joint as or correct the problem, if it is necessary. seen trhough an arthroscope: the rotator cuff (RC), the head fo the humerus Why is arthroscopy necessary? (HH), and the biceps tendon (B). Diagnosing joint injuries and disease begins with a thorough medical history, physical examination, and usually X-rays. Additional tests such as magnetic resonance imaging (MRI) or computed tomography (CT) also scan may be needed. -
Download Program
38th Annual San Diego Course June 4 – 5, 2021 Interactive Virtual Shoulder Course Arthroscopy Arthroplasty Fractures Program Chairmen: James C. Esch, M.D., SDSI President and C.E.O. Patrick J. Denard, M.D., Program Chair Final Program Tornier. A trusted name. A relentless focus. Innovation Now driven by Stryker. We’re doubling down on shoulder arthroplasty and to a T. renewing our promise to you and the patients you serve. Stryker. The leader, committed to making healthcare better. Tornier. The shoulder solutions, driving industry-leading innovation. You. The surgeon, delivering better outcomes for your patients. Coming together is what sets us apart. The innovation continues Summer 2021. TM and ® denote Trademarks and Registered Trademarks of Stryker Corporation or its affiliates. ©2021 Stryker Corporation or its affiliates. AP-015176A 06-MAY-2021 Instability excellence Redefining peak performance Elevate your expertise for shoulder instability repairs. With solutions ranging from simple to complex, Smith+Nephew’s Instability Excellence portfolio is setting new standards to take you to the next level while returning your patients to peak performance. Learn more at smith-nephew.com. Smith & Nephew, Inc., 150 Minuteman Road, Andover, MA 01810, www.smith-nephew.com, T +978 749 1000, US Customer Service: +1 800 343 5717 ◊Trademark of Smith+Nephew. All trademarks acknowledged. ©2021 Smith+Nephew. All rights reserved. Printed in USA. 30280 V1 04/21 Advanced healing solutions Redefining healing potential for rotator cuff repair REGENESORB◊ Material Replaced by bone within 24 months.*1,2 at 6 months at at 18 months at Comparisons of absorption, measured via μCT, at 6 and 18 months.3 Suture Anchor Learn more at smith-nephew.com. -

The Benefit of Arthroscopy for Symptomatic Total Knee Arthroplasty
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Arthroscopy for symptomatic total knee arthroplasty THE BENEFIT OF ARTHROSCOPY FOR SYMPTOMATIC TOTAL KNEE ARTHROPLASTY Hsiu-Peng Teng, Yi-Jiun Chou, Li-Chun Lin, and Chi-Yin Wong Department of Orthopedic Surgery, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan. Thirty-one knees with symptomatic total knee arthroplasty were diagnosed and treated arthroscopically. There were 18 knees with soft tissue impingement and 13 knees without. There were 16 knees with painful arthroplasty and range of motion (ROM) greater than 90°. Hypertrophied synovitis with or without impingement was more easily found by arthroscopy in this group than in the other 15 knees with the chief complaint of limited ROM, where more remarkable fibrotic tissue with intra-articular adhesion was found. Overall, the average improvement in ROM was 43.1° immediately after arthroscopy, and 20° at the final follow-up. Symptoms improved in 90.3% of patients, and 58.1% were satisfied with the outcome of their surgery. Arthroscopy is helpful for intra-articular diagnosis, obtaining a specimen for histopatho- logic analysis, culture for subclinical infection, and better improvement in ROM. In our experience, arthros- copy for symptomatic knee arthroplasty is reliable, safe and effective. Key Words: arthroscopy, total knee arthroplasty (Kaohsiung J Med Sci 2004;20:473–7) Total knee arthroplasty (TKA) is a popular and successful detailed history review, physical examination, and radio- treatment for knee-joint problems. However, a subset of graphic studies (anteroposterior, lateral and Merchant patients will suffer from persistent pain, with or without in- views) to detect possible pathologic conditions (e.g. -

Procedure Name: Knee Arthroscopy Brief Description of Procedure
Procedure Name: Knee Arthroscopy Brief Description of Procedure: Arthroscopic surgery is a common orthopedic procedure that is used to diagnose and treat problems in joints. Greek words: ‘arthro,’ meaning “joint” and ‘scope,’ meaning, “look.” When arthroscopy is per- formed, a telescope with a camera is inserted into the joint through a small incision. The camera is attached to a light source and shows a picture of the inside of the joint on a monitor. One or more incisions may be made to treat the underlying problem. This procedure can be used to diagnose a joint problem, perform surgery that repairs a joint problem, remove a loose or foreign body, or monitor a dis- ease or the effectiveness of a treatment. Arthroscopy is commonly performed on the knee, shoulder, and ankle. It also can be done on the hip, elbow, and wrist. Describe anesthesia type that typically is given: General Anesthesia is usually used for this surgery. See Anesthesia Section. What patients that smoke can expect when having surgery: After surgery your anesthesia specialist will check your breathing and lung sounds to determine if a breathing treatment is needed. Smoking increases airway irritation, which leads to wheezing and coughing. Further breathing treatments and medications are sometimes needed. Average length of surgery time: 45 minutes-1 hour Average length in immediate recovery: 30 minutes Average length for time of discharge: Expect to be here an average of one hour after surgery. During this time you may experience some discomfort. Medication can be given to make pain bearable. When can you go back to work: Depending on your occupation you and your doctor will discuss when you may return to work. -

Combining Orthopedic Special Tests to Improve Diagnosis of Shoulder Pathology
Physical Therapy in Sport 16 (2015) 87e92 Contents lists available at ScienceDirect Physical Therapy in Sport journal homepage: www.elsevier.com/ptsp Masterclass Combining orthopedic special tests to improve diagnosis of shoulder pathology * Eric J. Hegedus a, , Chad Cook b, Jeremy Lewis c, Alexis Wright a, Jin-Young Park d a High Point University, Department of Physical Therapy, High Point, NC 27262, USA b Physical Therapy Program, Duke University, Durham, NC, USA c Physiotherapy, University of Hertfordshire, Department of Allied Health Professions and Midwifery, School of Health and Social Work, United Kingdom d Shoulder, Elbow & Sports Center, Konkuk University, Seoul, South Korea article info abstract Article history: The use of orthopedic special tests (OSTs) to diagnose shoulder pathology via the clinical examination is Received 2 April 2014 standard in clinical practice. There is a great deal of research on special tests but much of the research is Received in revised form of a lower quality implying that the metrics from that research, sensitivity, specificity, and likelihood 5 July 2014 ratios, is likely to vary greatly in the hands of different clinicians and in varying practice environments. A Accepted 1 August 2014 way to improve the clinical diagnostic process is to cluster OSTs and to use these clusters to either rule in or out different pathologies. The aim of the article is to review the best OST clusters, examine the Keywords: methodology by which they were derived, and illustrate, with a case study, the use of these OST clusters Likelihood ratios Shoulder to arrive at a pathology-based diagnosis. © Diagnosis 2014 Elsevier Ltd. -

Procedure Coding in ICD-9-CM and ICD- 10-PCS
Procedure Coding in ICD-9-CM and ICD- 10-PCS ICD-9-CM Volume 3 Procedures are classified in volume 3 of ICD-9-CM, and this section includes both an Alphabetic Index and a Tabular List. This volume follows the same format, organization and conventions as the classification of diseases in volumes 1 and 2. ICD-10-PCS ICD-10-PCS will replace volume 3 of ICD-9-CM. Unlike ICD-10-CM for diagnoses, which is similar in structure and format as the ICD-9-CM volumes 1 and 2, ICD-10-PCS is a completely different system. ICD-10-PCS has a multiaxial seven-character alphanumeric code structure providing unique codes for procedures. The table below gives a brief side-by-side comparison of ICD-9-CM and ICD-10-PCS. ICD-9-CM Volume3 ICD-10-PCS Follows ICD structure (designed for diagnosis Designed and developed to meet healthcare coding) needs for a procedure code system Codes available as a fixed or finite set in list form Codes constructed from flexible code components (values) using tables Codes are numeric Codes are alphanumeric Codes are 3-4 digits long All codes are seven characters long ICD-9-CM and ICD-10-PCS are used to code only hospital inpatient procedures. Hospital outpatient departments, other ambulatory facilities, and physician practices are required to use CPT and HCPCS to report procedures. ICD-9-CM Conventions in Volume 3 Code Also In volume 3, the phrase “code also” is a reminder to code additional procedures only when they have actually been performed. -

Open Reduction and Internal Fixation (ORIF)
FACT SHEET FOR PATIENTS AND FAMILIES Open Reduction and Internal Fixation (ORIF) What is it and why do I need it? Open reduction and internal fixation (ORIF) is surgery to repair a broken bone. Open reduction means the doctor makes an incision (cut) to reach the bones and move them back into their normal position. Internal fixation means metal screws, plates, sutures, or rods are placed on the bone to keep it in place while it heals. The internal fixation will not be removed. Why do I need it? This surgery is done on an arm or a leg to repair fractures Before After that would not heal properly with a cast or splint alone. Your surgeon may recommend ORIF if: In the picture on the left, the arm bone is severely broken. In the picture on the right, the arm bone is held • The bone is broken into many pieces together with metal devices called internal fixation. • The bone is sticking out of the skin They will not be removed after the bone heals. • The bone is not lined up correctly • A closed reduction (without opening the skin) Talking with your doctor was done before and it didn’t heal properly The table below lists the most common potential benefits, • A joint is dislocated risks, and alternatives for ORIF surgery to repair a broken This surgery should allow your bone to heal properly. bone. There may be other benefits or risks in your unique When it does, you will have less pain and be better able to medical situation. -
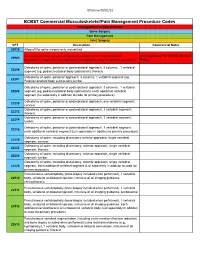
Commercial MSK Procedure Code List Effective 09.01.21.Xlsx
Effective 09/01/21 BCBST Commercial Musculoskeletal/Pain Management Procedure Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery CPT Description Commercial Notes 20930 Allograft for spine surgery only morselized Computer-assisted surgical navigational procedure for musculoskeletal Investigational Per BCBST Medical 20985 procedures, image-less (List separately in addition to code for primary procedure) Policy Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22206 segment (eg, pedicle/vertebral body subtraction); thoracic Osteotomy of spine, posterior approach, 3 columns, 1 vertebral segment (eg. 22207 Pedicle/vertebral body subtraction);lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22208 segment (eg, pedicle/vertebral body subtraction); each additional vertebral segment (list separately in addition to code for primary procedure) Osteotomy of spine, posterior or posterolateral approach, one vertebral segment; 22210 cervical Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22212 thoracic Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22214 lumbar Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22216 each additional vertebral segment (List separately in addition to primary procedure) Osteotomy of spine, including discectomy anterior approach, single vertebral 22220 segment; cervical Osteotomy of spine, including discectomy, anterior approach, single -

Wilson Osteotomy Stabilised by Means of Internal Fixation for the Treatment of Hallux Valgus
Acta Orthop. Belg., 2004, 70, 57-63 Wilson osteotomy stabilised by means of internal fixation for the treatment of hallux valgus Panagiotis GIVISSIS, Dimitrios KARATAGLIS, Anastasios CHRISTODOULOU, Ioannis TERZIDIS, John POURNARAS The results achieved in 20 patients (32 feet) who tomy did not include any type of internal stabilisa- underwent Wilson’s osteotomy of the first metatarsal tion ; the operation therefore frequently necessitat- for the treatment of hallux valgus were reviewed. In ed prolonged plaster cast immobilisation due to the all cases the osteotomy site was stabilised with one or lack of inherent mechanical stability. two cortical screws. The patients’ average age was Some authors have subsequently tried various 50.7 years (range : 34-74 years) and they were fol- types of internal fixation of the osteotomy site, in lowed for a mean period of 33.1 months (range 12- 63 months). order to obviate the need for plaster cast immobili- The average AOFAS score was 85.5 (range : 62-100) sation (1, 8, 21). In this paper the results of Wilson’s at the final follow-up and in 84.4% of the cases the osteotomy stabilised with one or two cortical final outcome was very satisfactory as far as sympto- screws are presented. matic improvement was concerned. Wilson’s osteotomy stabilised with cortical screws PATIENTS AND METHODS was found to reliably give satisfactory correction of the hallux valgus and first intermetatarsal angles, Twenty patients (32 feet) who underwent Wilson’s while allowing safe patient mobilisation and early osteotomy with internal fixation with one or two screws weight bearing. -

Assessment of Discectomy and Eminectomy for Temporomandibular Joint Derangement: Manitoba Experience
Assessment of Discectomy and Eminectomy for Temporomandibular Joint Derangement: Manitoba Experience Bachelor of Science in Dentistry (B.Sc. Dent) Thesis By: Harmeet Manghera B.Sc. Dent 2019 Supervisors: Dr. Reda F. Elgazzar and Dr. Adnan Shah Dental Diagnostic and Surgical Sciences Oral and MaxilloFacial Surgery TABLE OF CONTENTS ACKNOWLEDGEMENTS …….……...…………………………………………………..….… 3 ABSTRACT …………………………………………………………………………………..…..4 INTRODUCTION …………………………………….………………………………………….5 PATIENTS AND METHODS………………………………………………...………………….7 RESULTS………………………………………………………………………..……………......9 DISCUSSION…………………………………………………………………………...……….13 CONCLUSION…………………………………………………………………….…………….17 REFERENCES…………………………………………………………………………………. 18 2 Acknowledgements I wish to express my sincere gratitude towards my mentors Dr. Elgazzar and Dr. Shah, in the department of DDSS/OMFS, for their encouragement and supervision during this project. I am also grateful to Dr. Bhullar, the Associate Dean of Research, for running the BSc (Dent) Program through the Faculty of Dentistry, University of Manitoba. This project was partially supported by the Canadian Association of Oral and Maxillofacial Surgeons. HSC and SOGH Health Records personnel provided the resources needed to complete this thesis. It would not have been possible without their help. I am thankful for my parents for providing moral support and encouragement along the journey. 3 Abstract Temporomandibular joint disorder (TMD) is caused by the loss of function of the intra- articular tissues, leading to a failure in the -

Primary Arthrodesis Versus Open Reduction Internal
ORTHOPAEDIC SURGERY ANZJSurg.com Primary arthrodesis versus open reduction internal fixation for complete Lisfranc fracture dislocations: a retrospective study comparing functional and radiological outcomes Nathan Kirzner , Wesley Teoh, Sianne Toemoe, Tim Maher, Rejith Mannambeth, Andrew Hughes, Daniel Goldbloom, Hamish Curry and Harvinder Bedi Alfred Hospital, Melbourne, Victoria, Australia Key words Abstract anatomical reduction, complete Lisfranc fracture dislocation, functional outcome, open reduction Background: The aims of this retrospective study were to compare the functional and internal fixation, primary arthrodesis. radiological outcomes of primary arthrodesis and open reduction internal fixation (ORIF) for the treatment of complete Lisfranc fracture dislocations. Correspondence Methods: A retrospective cohort study of 39 patients treated for a complete Lisfranc frac- Dr Nathan Kirzner, Alfred Hospital, 55 Commercial ture dislocation, defined as Myerson types A and C2, over a period of 8 years at a level Road, Melbourne, VIC 3004, Australia. 1 trauma centre was performed. Of these, 18 underwent primary arthrodesis, and 21 ORIF. Email: [email protected] The primary outcome measures included the American Orthopaedic Foot and Ankle Society N. Kirzner MBBS, BSc, MSurgSC, MRadTher; score, the validated Manchester Oxford Foot Questionnaire functional tool, and the second- W. Teoh MBBS; S. Toemoe MBBS; T. Maher ary outcome was the radiological Wilppula classification of anatomical reduction. MBBS; R. Mannambeth MBBS, MS (Ortho), DNB Results: Significantly better functional outcomes were seen in the primary arthrodesis (Ortho); A. Hughes FRACS (Ortho); D. Goldbloom group. These patients had a mean Manchester Oxford Foot Questionnaire score of 30.1 MBBS, FRACS (Ortho); H. Curry MBBS, FRACS points, compared with 45.1 for the ORIF group (P = 0.017). -

Minimally Invasive Orthopedic Surgery: Arthroscopy
Minimally Invasive Orthopedic Surgery: Arthroscopy Robert Treuting, MD Department of Surgery, Ochsner Clinic and Alton Ochsner Medical Foundation, New Orleans, LA Arthroscopy,aminimallyinvasivealternativetostandardopensurgicaltechniquesandnowthemostcommonly performedorthopedicsurgicalprocedure,wasoneofthegreatestadvancesinorthopedicsurgeryofthe20 th century.Minimallyinvasivesurgeriesresultinlesspostoperativeswellingthanopentechniquesandreduce pain,riskofcomplications,andrecoverytimes.Arthroscopyhasevolvedfromadiagnostictooltoatherapeutic toolcapableoftreatingawiderangeofinjuriesanddisorders.Manyinjuries,particularlythosethatatonetime wouldhavebeencareerendingforathletes,cannowbeaddressedwitharthroscopyallowingaquickerreturnto fullfunction.Whilearthroscopyhasresultedinanoveralldecreaseinmorbiditycomparedwithopentechniques, itisstillaninvasiveprocedureandinherentlyinvolvesrisks.Almostallarthroscopicprocedurescanbeperformed inanoutpatientsetting.In1999,211arthroscopicprocedureswereperformedatOchsner. TreutingR.Minimallyinvasiveorthopedicsurgery:arthroscopy.TheOchsnerJournal2000;2:158-163. rthopedicsurgery,likeallfieldsofmedicine,experienced outbreakofWorldWarII.In1921,Bircher(1882-1956)useda tremendousprogressinthe20thcentury.Alongwithan modifiedJacobaeuslaparoscopetovisualizetheinteriorofthe O improvedunderstandingofbasicmolecular,cellular, kneein18patientsinSwitzerlandandlaterpublishedhisfindings genetic,andbiomechanicalfactorsofthemusculoskeletalsystem, onposttraumaticarthritisandthediagnosisofmeniscalpathology jointreplacementsurgeryandarthroscopicsurgerywerethetwo