Antidepressants Comparison Guide Most Commonly Prescribed
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Concomitant Drugs Associated with Increased Mortality for MDMA Users Reported in a Drug Safety Surveillance Database Isaac V
www.nature.com/scientificreports OPEN Concomitant drugs associated with increased mortality for MDMA users reported in a drug safety surveillance database Isaac V. Cohen1, Tigran Makunts2,3, Ruben Abagyan2* & Kelan Thomas4 3,4-Methylenedioxymethamphetamine (MDMA) is currently being evaluated by the Food and Drug Administration (FDA) for the treatment of post-traumatic stress disorder (PTSD). If MDMA is FDA-approved it will be important to understand what medications may pose a risk of drug– drug interactions. The goal of this study was to evaluate the risks due to MDMA ingestion alone or in combination with other common medications and drugs of abuse using the FDA drug safety surveillance data. To date, nearly one thousand reports of MDMA use have been reported to the FDA. The majority of these reports include covariates such as co-ingested substances and demographic parameters. Univariate and multivariate logistic regression was employed to uncover the contributing factors to the reported risk of death among MDMA users. Several drug classes (MDMA metabolites or analogs, anesthetics, muscle relaxants, amphetamines and stimulants, benzodiazepines, ethanol, opioids), four antidepressants (bupropion, sertraline, venlafaxine and citalopram) and olanzapine demonstrated increased odds ratios for the reported risk of death. Future drug–drug interaction clinical trials should evaluate if any of the other drug–drug interactions described in our results actually pose a risk of morbidity or mortality in controlled medical settings. 3,4-Methylenedioxymethamphetamine (MDMA) is currently being evaluated by the Food and Drug Adminis- tration (FDA) for the treatment of posttraumatic stress disorder (PTSD). During the past two decades, “ecstasy” was illegally distributed and is purported to contain MDMA, but because the market is unregulated this “ecstasy” may actually contain adulterants or no MDMA at all1. -

Canadian Stroke Best Practice Recommendations
CANADIAN STROKE BEST PRACTICE RECOMMENDATIONS MOOD, COGNITION AND FATIGUE FOLLOWING STROKE Table 1C: Summary Table for Selected Pharmacotherapy for Post-Stroke Depression Update 2019 Lanctôt KL, Swartz RH (Writing Group Chairs) on Behalf of the Canadian Stroke Best Practice Recommendations Mood, Cognition and Fatigue following Stroke Writing Group and the Canadian Stroke Best Practice and Quality Advisory Committee, in collaboration with the Canadian Stroke Consortium © 2019 Heart & Stroke Heart and Stroke Foundation Mood, Cognition and Fatigue following Stroke Canadian Stroke Best Practice Recommendations Table 1C Table 1C: Summary Table for Selected Pharmacotherapy for Post-Stroke Depression This table provides a summary of the pharmacotherapeutic properties, side effects, drug interactions and other important information on selected classes of medications available for use in Canada and more commonly recommended for post-stroke depression. This table should be used as a reference guide by health care professionals when selecting an appropriate agent for individual patients. Patient compliance, patient preference and/or past experience, side effects, and drug interactions should all be taken into consideration during decision-making, in addition to other information provided in this table and available elsewhere regarding these medications. Selective Serotonin Reuptake Inhibitors (SSRI) Serotonin–norepinephrine reuptake Other inhibitors (SNRI) Medication *citalopram – Celexa *duloxetine – Cymbalta methylphenidate – Ritalin (amphetamine) -

Formulary and Prescribing Guidelines
Formulary and Prescribing Guidelines SECTION 1: TREATMENT OF DEPRESSION Section 1. Treatment of depression 1.1 Introduction This guidance should be considered as part of a stepped care approach in the management of depressive disorders. Antidepressants are not routinely recommended for persistent sub-threshold depressive symptoms or mild depression but can be considered in these categories where there is a past history of moderate or severe depression, initial presentation of sub-threshold depressive symptoms for at least 2 years, and persistence of either mild or sub-threshold depression after other interventions1 have failed. The most current NICE guidance should be consulted wherever possible to obtain the most up to date information. For individuals with moderate or severe depression, a combination of antidepressant medication and a high intensity psychological intervention (CBT or IPT) is recommended. When depression is accompanied by symptoms of anxiety, usually treat the depression first. If the person has an anxiety disorder and co-morbid depression or depressive symptoms, consider treating the anxiety first. Also consider offering advice on sleep hygiene, by way of establishing regular sleep and wake times; avoiding excess eating, avoiding smoking and drinking alcohol before sleep; and taking regular physical exercise if possible. Detailed information on the treatment of depression in children and adolescents can be found in section 12. Further guidance on prescribing for older adults and for antenatal/postnatal service users can be found in section 11 and section 20, respectively. 1.2 Approved Drugs for the treatment of Depression in Adults For licensing indications, see Annex 1 Drug5 Formulation5 Comments2,3,4 Caps 20mg, 60mg Selective serotonin reuptake inhibitor (SSRI) Fluoxetine Liquid 20mg/5ml 1st line SSRI (based on acquisition cost) Tabs 10mg, 25mg, 50mg Amitriptyline Tricyclic (TCA). -

Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2012 Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors Marisa Rosenberg Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2715 This Thesis is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. ANTINOCICEPTIVE EFFECTS OF MONOAMINE REUPTAKE INHIBITORS IN ASSAYS OF PAIN-STIMULATED AND PAIN-DEPRESSED BEHAVIOR A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science at Virginia Commonwealth University By Marisa B. Rosenberg Bachelor of Science, Temple University, 2008 Advisor: Sidney Stevens Negus, Ph.D. Professor, Department of Pharmacology/Toxicology Virginia Commonwealth University Richmond, VA May, 2012 Acknowledgement First and foremost, I’d like to thank my advisor Dr. Steven Negus, whose unwavering support, guidance and patience throughout my graduate career has helped me become the scientist I am today. His dedication to education, learning and the scientific process has instilled in me a quest for knowledge that I will continue to pursue in life. His thoroughness, attention to detail and understanding of pharmacology has been exemplary to a young person like me just starting out in the field of science. I’d also like to thank all of my committee members (Drs. -
Print Your Symptom Diary
MEDICATION GUIDE FETZIMA® (fet-ZEE-muh) (levomilnacipran) extended-release capsules, for oral use What is the most important information I should know about FETZIMA? FETZIMA may cause serious side effects, including: • Increased risk of suicidal thoughts or actions in some children, adolescents, and young adults. FETZIMA and other antidepressant medicines may increase suicidal thoughts or actions in some children and young adults, especially within the first few months of treatment or when the dose is changed. FETZIMA is not for use in children. o Depression or other serious mental illnesses are the most important causes of suicidal thoughts or actions. Some people may have a higher risk of having suicidal thoughts or actions. These include people who have (or have a family history of) depression, bipolar illness (also called manic-depressive illness) or have a history of suicidal thoughts or actions. How can I watch for and try to prevent suicidal thoughts and actions? o Pay close attention to any changes, especially sudden changes in mood, behavior, thoughts, or feelings, or if you develop suicidal thoughts or actions. This is very important when an antidepressant medicine is started or when the dose is changed. o Call your healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings. o Keep all follow-up visits with your healthcare provider as scheduled. Call your healthcare provider between visits as needed, especially if you have concerns about symptoms. Call your healthcare provider or -

Levomilnacipran (Fetzima®) Indication
Levomilnacipran (Fetzima®) Indication: Indicated for the treatment of major depressive disorder (MDD), FDA approved July 2013. Mechanism of action Levomilnacipran, the more active enantiomer of racemic milnacipran, is a selective SNRI with greater potency for inhibition of norepinephrine relative to serotonin reuptake Compared with duloxetine or venlafaxine, levomilnacipran has over 10-fold higher selectivity for norepinephrine relative to serotonin reuptake inhibition The exact mechanism of the antidepressant action of levomilnacipran is unknown Dosage and administration Initial: 20 mg once daily for 2 days and then increased to 40 mg once daily. The dosage can be increased by increments of 40 mg at intervals of two or more days Maintenance: 40-120 mg once daily with or without food. Fetzima should be swallowed whole (capsule should not be opened or crushed) Levomilnacipran and its metabolites are eliminated primarily by renal excretion o Renal impairment Dosing: Clcr 30-59 mL/minute: 80 mg once daily Clcr 15-29 mL/minute: 40 mg once daily End-stage renal disease (ESRD): Not recommended Discontinuing treatment: Gradually taper dose, if intolerable withdrawal symptoms occur, consider resuming the previous dose and/or decrease dose at a more gradual rate How supplied: Capsule ER 24 Hour Fetzima Titration: 20 & 40 mg (28 ea) Fetzima: 20 mg, 40 mg, 80 mg, 120 mg Warnings and Precautions Elevated Blood Pressure and Heart Rate: measure heart rate and blood pressure prior to initiating treatment and periodically throughout treatment Narrow-angle glaucoma: may cause mydriasis. Use caution in patients with controlled narrow- angle glaucoma Urinary hesitancy or retention: advise patient to report symptoms of urinary difficulty Discontinuation Syndrome Seizure disorders: Use caution with a previous seizure disorder (not systematically evaluated) Risk of Serotonin syndrome when taken alone or co-administered with other serotonergic agents (including triptans, tricyclics, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. -

Meta-Analysis of the Dose-Response Relationship of SSRI in Obsessive
Molecular Psychiatry (2010) 15, 850–855 & 2010 Macmillan Publishers Limited All rights reserved 1359-4184/10 www.nature.com/mp ORIGINAL ARTICLE Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder MH Bloch1, J McGuire1, A Landeros-Weisenberger1, JF Leckman1 and C Pittenger2 1Yale Child Study Center, Yale University School of Medicine, New Haven, CT, USA and 2Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA We sought to determine differences in efficacy and tolerability between different doses of selective serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder (OCD) using meta-analysis. We identified 9 studies involving 2268 subjects that were randomized, double-blind placebo-controlled clinical trials that compared multiple, fixed- doses of selective serotonin reuptake inhibitors (SSRIs) to each other and to placebo in the treatment of adults with OCD. Change in Y-BOCS score, proportion of treatment responders, and dropouts (all-cause and due to side-effects) were determined for each included study. Weighted mean difference was used to examine mean change in Y-BOCS score. Pooled absolute risk difference was used to examine dichotomous outcomes. Meta-analysis was performed using a fixed effects model in RevMan 4.2.8. We found that compared with either low or medium doses, higher doses of SSRIs were associated with improved treatment efficacy, using either Y-BOCS score or proportion of treatment responders as an outcome. Dose of SSRIs was not associated with the number of all-cause dropouts. Higher doses of SSRIs were associated with significantly higher proportion of dropouts due to side-effects. -

Cipramil® 20 Mg Film-Coated Tablets
NEW ZEALAND DATA SHEET 1 NAME OF THE MEDICINE Cipramil® 20 mg Film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Cipramil 20 mg Film-coated tablets contain 24.98 mg citalopram hydrobromide, corresponding to 20 mg citalopram base. Excipients with known effect: lactose For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Cipramil tablets are oval, white, film-coated tablets, 8 mm × 5.5 mm, marked “C” and “N” symmetrically around the score-line. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of depressive illness in the initial phase and as maintenance against potential relapse/ recurrence. 4.2 Dose and method of administration The dose may be taken in the morning or evening without regard for food. As the treatment result in general can be evaluated only after 2-3 weeks’ treatment, a possible dose increase in increments of 10 mg should take place with intervals of 2-3 weeks. Adults Cipramil should be administered as a single oral dose of 20 mg daily. Dependent on individual patient response and severity of depression the dose may be increased to a maximum of 40 mg daily. The maximum daily dose should not be exceeded as doses above 40mg/day are associated with an increased risk of QT prolongation. Elderly patients The starting dose is 10mg/day. The dose can be increased by 10mg to a maximum of 20mg/day. Use in children and adolescents (under 18 years of age) Safety and efficacy have not been established in this population. Consequently, citalopram should not be used in children and adolescents under 18 years of age (see Section 4.4 Special warnings and precautions or use). -

A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
A synbiotic mixture augmented the efficacy of doxepin, venlafaxine, and fluvoxamine in mice model of depression Azadeh Mesripour1, Andiya Meshkati1, Valiolah Hajhashemi2 1Department of Pharmacology and Toxicology, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. 2‐ Isfahan Pharmaceutical Sciences Research Center, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. ABSTRACT Objective: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals, may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicineproof in order to augment the efficacy of therapeutic doses of antidepressant drugs seems to be very important. Therefore the effect of adding a synbiotic cocktail in drinking water was assessed in mice model of despair following administrating three antidepressant drugs belonging to different classes. Methods: The marble burring test (MBT), and forced swimming test (FST) were used as animal model of obsessive behavior and despair. The synbiotic cocktail was administered in mice drinking water (6.25×106 CFU) for 14 days and the tests were performed on the days 7 and 14 thirty minutes after injecting the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg). Results: After 7 days of the synbiotic ingestion immobility time decreased in FST for doxepin (92 sec ± 5.5) and venlafaxine (17.3 sec ± 2.5) compared to their control group (drinking water) but fluvoxamine could decrease immobility time after 14 days of ingesting the synbiotic (70 sec ± 7.5). -

Sertraline and Venlafaxine-Induced Nocturnal Enuresis
Case Report DOI: 10.5455/bcp.20140304091103 Sertraline and Venlafaxine-Induced Nocturnal Enuresis Inci Meltem Atay1, Gulin Ozdamar Unal2 ABS TRACT: Sertraline and venlafaxine-induced nocturnal enuresis Nocturnal enuresis is defined as the involuntary discharge of urine after the age of expected continence that occurs during sleep at night. Although there are a few reports in adults for nocturnal enuresis associated 1Assist. Prof., 2M.D., Suleyman Demirel University, School of Medicine, Department with serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs), the of Psychiatry, Isparta - Turkey mechanism or frequency of this side effect have not been identified yet. We report here a case of nocturnal Corresponding author: Dr. İnci Meltem Atay enuresis associated with both sertraline and venlafaxine in different major depressive episodes in an adult Süleyman Demirel Universitesi, Tıp Fakültesi, Psikiyatri Anabilim Dalı, Isparta - Türkiye patient that resolves after the discontinuation of the medications and continuation with escitalopram. To our E-ma il add ress: knowledge, in literature there have been no reports about nocturnal enuresis caused by those two agents in [email protected] the same patient. This case is discussed in detail for the recurrence of nocturnal enuresis, the importance of Date of submission: detailed assessment of even rare side effects and for their possible mechanisms. February 11, 2014 Date of acceptance: March 04, 2014 Keywords: nocturnal enuresis, venlafaxine, sertraline, depression Declaration of interest: I.M.A, G.O.U.: The authors reported no Klinik Psikofarmakoloji Bulteni - Bulletin of Clinical Psychopharmacology 2015;25(3):287-90 conflict of interest related to this article. INTRODUCTION side effect1-6. -
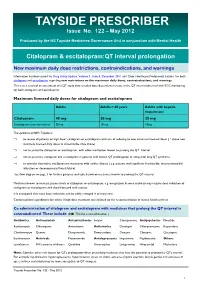
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution.