Pulse Oximetry Training Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

Hypoxia Infographic
Understanding HYP XIA Hypoxia is an environmental phenomenon where the concentration of dissolved oxygen in the water column decreases to a level that can no longer 1 support living aquatic organisms. The level is often considered to be 2 mg O2 per liter of water or lower. Hypoxic and anoxic (no oxygen) waters have existed throughout geologic time, but their occurrence in shallow coastal and estuarine areas appears to be increasing as a result of human activities. 2 What causes hypoxia? In 2015, scientists determined the Gulf of Mexico dead zone to be 6,474 square miles, which is an area about the size of Connecticut and Rhode Island combined. 3 Major events leading to the formation of hypoxia in the Gulf of Mexico include: Coastal Hypoxia and Eutrophication Sunlight Watershed Areas of anthropogenically-influenced n> In the past century, Hypoxia has become a global concern with estuarine and coastal hypoxia. 550 over 550 coastal areas identified as experiencing this issue. 4 Runoff and nutrient 1 loading of the Mississippi River. Nutrient-rich water from the Mississippi River forms 1960 a surface lens. 1970 Combined, Dead Zones 1980 cover 4x the area of the 1990 Great Lakes. % 2000 Nutrient-enhanced 4 2 primary production, Only a small fraction of the 550-plus Number of dead zones has approximately Today, there is currently about 1,148,000 km2 or eutrophication. hypoxia zones exhibited any signs doubled each decade since the 1960’s. 5 of seabed covered by Oxygen Minimum Phytoplankton growth of improvement. 5 Zones (OMZs) (<0.5 ml of O /liter) 5 is fueled by nutrients. -

Gulf of Mexico Hypoxia Monitoring Strategy
Gulf of Mexico Hypoxia Monitoring Strategy Hypoxia Zone Areal Extent (km2) Interpolation Observations Data Analysis Workshop Steering Committee Trevor Meckley, Alan Lewitus, A White Paper by the Steering Committee of the: Dave Scheurer, Dave Hilmer NOAA National Ocean Service, National 6th Annual NOAA/NGI Hypoxia Research Centers of Coastal Ocean Science Coordination Workshop: Establishing a Steve Ashby Cooperative Hypoxic Zone Monitoring Program Northern Gulf Institute convened by the NOAA National Centers for Steve DiMarco Texas A&M University Coastal Ocean Science and Northern Gulf Institute Steve Giordano on 12-13 September 2016 at the Mississippi State NOAA National Marine Fisheries Service University Science and Technology Center at Rick Greene NASA's Stennis Space Center in Mississippi. EPA Office of Research and Development Stephan Howden University of Southern Mississippi Barb Kirkpatrick Gulf of Mexico Coastal Ocean Observing System Troy Pierce EPA Gulf of Mexico Program Nancy Rabalais Louisiana Universities Marine Consortium Rick Raynie Louisiana Coastal Protection and Restoration Authority Mike Woodside USGS National Water Quality Program Abstract The Gulf of Mexico Hypoxia Monitoring Strategy is a resource to inform the proceedings of the 6th Annual NOAA/NGI Hypoxia Research Coordination Workshop: Establishing a Cooperative Hypoxic Zone Monitoring Program. It provides a framework for a cooperative hypoxia monitoring program based on programmatic and financial requirements that are designed to meet management needs. The Monitoring Strategy includes sections on management drivers, current monitoring capabilities and gaps, and projected programmatic, data, and financial requirements based on the input of multiple partners and the responses from a survey of modelers currently applying deterministic 3D time variable models to Gulf hypoxia assessment and prediction. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Zooplankton Community Response to Seasonal Hypoxia: a Test of Three Hypotheses
diversity Article Zooplankton Community Response to Seasonal Hypoxia: A Test of Three Hypotheses Julie E. Keister *, Amanda K. Winans and BethElLee Herrmann School of Oceanography, University of Washington, Box 357940, Seattle, WA 98195, USA; [email protected] (A.K.W.); [email protected] (B.H.) * Correspondence: [email protected] Received: 7 November 2019; Accepted: 28 December 2019; Published: 1 January 2020 Abstract: Several hypotheses of how zooplankton communities respond to coastal hypoxia have been put forward in the literature over the past few decades. We explored three of those that are focused on how zooplankton composition or biomass is affected by seasonal hypoxia using data collected over two summers in Hood Canal, a seasonally-hypoxic sub-basin of Puget Sound, Washington. We conducted hydrographic profiles and zooplankton net tows at four stations, from a region in the south that annually experiences moderate hypoxia to a region in the north where oxygen remains above hypoxic levels. The specific hypotheses tested were that low oxygen leads to: (1) increased dominance of gelatinous relative to crustacean zooplankton, (2) increased dominance of cyclopoid copepods relative to calanoid copepods, and (3) overall decreased zooplankton abundance and biomass at hypoxic sites compared to where oxygen levels are high. Additionally, we examined whether the temporal stability of community structure was decreased by hypoxia. We found evidence of a shift toward more gelatinous zooplankton and lower total zooplankton abundance and biomass at hypoxic sites, but no clear increase in the dominance of cyclopoid relative to calanoid copepods. We also found the lowest variance in community structure at the most hypoxic site, in contrast to our prediction. -

Hypoxia the Gulf of Mexico’S Summertime Foe
Louisiana Coastal Wetlands Planning, Protection and Restoration News September 2004 Number 26 HYPOXIA THE GULF OF MEXICO’S SUMMERTIME FOE More Nitrogen Upstream, Fewer Filters Downstream Caernarvon: A Case Study WaterMarks Interview: John Day, LSU www.lacoast.gov September 2004 Number 26 WaterMarks is published three times a Louisiana Coastal Wetlands Planning, Protection and Restoration News year by the Louisiana Coastal Wetlands Conservation and Restoration Task Force to communicate news and issues Contents of interest related to the Coastal Wetlands Planning, Protection and Restoration Act of 1990. This legislation 3 Hypoxia: funds wetlands enhancement projects The Gulf of Mexico’s Summertime Foe nationwide, designating approximately $50 million annually for work in More Nitrogen Upstream, Louisiana. The state contributes 6 Fewer Filters Downstream 15 percent of the total cost of the project. Can Wetlands Restoration 8 Revitalize Offshore Waters? Caernarvon: 10 A Case Study What Lies Ahead 12 for the Dead Zone? Please address all questions, comments and changes of address to: WaterMarks Interview: James D. Addison 14 John Day, LSU WaterMarks Editor New Orleans District US Army Corps of Engineers P.O. Box 60267 Special thanks to Doug Daigle, Mississippi River Basin Alliance; Dugan Sabins, New Orleans, LA 70160-0267 (504) 862-2201 Louisiana State Hypoxia Committee; Ken Teague, U.S. Environmental Protection Agency; and Robert Twilley, Louisiana State University, for their assistance with e-mail: this issue of WaterMarks. [email protected] For more information about Louisiana’s coastal wetlands and the efforts planned and under way to ensure their survival, check out these sites on the web: www.lacoast.gov www.btnep.org www.saveLAwetlands.org About the Cover Blue Runners, a common Gulf Subscribe species, have the ability to escape To receive WaterMarks, e-mail [email protected] from waters with low oxygen con- For current meetings, events, and other news concerning Louisiana’s coastal tent. -

The Economics of Dead Zones: Causes, Impacts, Policy Challenges, and a Model of the Gulf of Mexico Hypoxic Zone S
58 The Economics of Dead Zones: Causes, Impacts, Policy Challenges, and a Model of the Gulf of Mexico Hypoxic Zone S. S. Rabotyagov*, C. L. Klingy, P. W. Gassmanz, N. N. Rabalais§ ô and R. E. Turner Downloaded from Introduction The BP Deepwater Horizon oil spill in the Gulf of Mexico in 2010 increased public awareness and http://reep.oxfordjournals.org/ concern about long-term damage to ecosystems, and casual readers of the news headlines may have concluded that the spill and its aftermath represented the most significant and enduring environmental threat to the region. However, the region faces other equally challenging threats including the large seasonal hypoxic, or “dead,” zone that occurs annually off the coast of Louisiana and Texas. Even more concerning is the fact that such dead zones have been appearing worldwide at proliferating rates (Conley et al. 2011; Diaz and Rosenberg 2008). Nutrient over- enrichment is the main cause of these dead zones, and nutrient-fed hypoxia is now widely at Iowa State University on January 27, 2014 considered an important threat to the health of aquatic ecosystems (Doney 2010). The rather alarming term dead zone is surprisingly appropriate: hypoxic regions exhibit oxygen levels that are too low to support many aquatic organisms including commercially desirable species. While some dead zones are naturally occurring, their number, size, and *School of Environmental and Forest Sciences, University of Washington, Seattle, Washington, USA; e-mail: [email protected] yCenter for Agricultural and Rural Development, -

Coupling and Decoupling of High Biomass Phytoplankton Production and Hypoxia in a Highly Dynamic Coastal System: the Changjiang (Yangtze River) Estuary
fmars-07-00259 May 26, 2020 Time: 17:51 # 1 ORIGINAL RESEARCH published: 28 May 2020 doi: 10.3389/fmars.2020.00259 Coupling and Decoupling of High Biomass Phytoplankton Production and Hypoxia in a Highly Dynamic Coastal System: The Changjiang (Yangtze River) Estuary Feng Zhou1,2*, Fei Chai1,3*, Daji Huang1, Mark Wells3,1, Xiao Ma1, Qicheng Meng1, Huijie Xue3,4, Jiliang Xuan1, Pengbin Wang1,5, Xiaobo Ni1, Qiang Zhao6, Chenggang Liu1,5, Jilan Su5 and Hongliang Li1 1 State Key Laboratory of Satellite Ocean Environment Dynamics, Second Institute of Oceanography, Ministry of Natural Resources, Hangzhou, China, 2 School of Oceanography, Shanghai Jiao Tong University, Shanghai, China, 3 School Edited by: of Marine Science, University of Maine, Orono, ME, United States, 4 State Key Laboratory of Tropical Oceanography, South Marta Marcos, China Sea Institute of Oceanology, Chinese Academy of Sciences, Guangzhou, China, 5 Key Laboratory of Marine University of the Balearic Islands, Ecosystem Dynamics, Second Institute of Oceanography, Ministry of Natural Resources, Hangzhou, China, 6 Ningbo Marine Spain Environment Monitoring Center Station, Ministry of Natural Resources, Ningbo, China Reviewed by: Sabine Schmidt, The global increase in coastal hypoxia over the past decades has resulted from a Centre National de la Recherche Scientifique (CNRS), France considerable rise in anthropogenically-derived nutrient loading. The spatial relationship Antonio Olita, between surface phytoplankton production and subsurface hypoxic zones often can Italian National Research Council (CNR), Italy be explained by considering the oceanographic conditions associated with basin size, *Correspondence: shape, or bathymetry, but that is not the case where nutrient-enriched estuarine Feng Zhou waters merge into complex coastal circulation systems. -
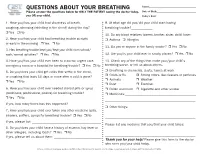
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7. -

Scientific Assessment of Hypoxia in U.S. Coastal Waters
Scientific Assessment of Hypoxia in U.S. Coastal Waters 0 Dissolved oxygen (mg/L) 6 0 Depth (m) 80 32 Salinity 34 Interagency Working Group on Harmful Algal Blooms, Hypoxia, and Human Health September 2010 This document should be cited as follows: Committee on Environment and Natural Resources. 2010. Scientific Assessment of Hypoxia in U.S. Coastal Waters. Interagency Working Group on Harmful Algal Blooms, Hypoxia, and Human Health of the Joint Subcommittee on Ocean Science and Technology. Washington, DC. Acknowledgements: Many scientists and managers from Federal and state agencies, universities, and research institutions contributed to the knowledge base upon which this assessment depends. Many thanks to all who contributed to this report, and special thanks to John Wickham and Lynn Dancy of NOAA National Centers for Coastal Ocean Science for their editing work. Cover and Sidebar Photos: Background Cover and Sidebar: MODIS satellite image courtesy of the Ocean Biology Processing Group, NASA Goddard Space Flight Center. Cover inset photos from top: 1) CTD rosette, EPA Gulf Ecology Division; 2) CTD profile taken off the Washington coast, project funded by Bonneville Power Administration and NOAA Fisheries; Joseph Fisher, OSU, was chief scientist on the FV Frosti; data were processed and provided by Cheryl Morgan, OSU); 3) Dead fish, Christopher Deacutis, Rhode Island Department of Environmental Management; 4) Shrimp boat, EPA. Council on Environmental Quality Office of Science and Technology Policy Executive Office of the President Dear Partners and Friends in our Ocean and Coastal Community, We are pleased to transmit to you this report, Scientific Assessment ofHypoxia in u.s. -

Value of Pulse Oximetry in Screening for Long-Term Oxygen Therapy Requirement
Copyright CERS Journals Ltd 1993 Eur Reaplr J, 1993, 6, 559-562 European Respiratory Journal Printed In UK • all rlghta reaerved ISSN 0903 • 1936 TECHNICAL NOTE Value of pulse oximetry In screening for long-term oxygen therapy requirement C.M. Roberts, J.R. Bugler, R. Melchor, M.R. Hetzel, S.G. Spire Value of pulse oximetry in screening for long-term oxygen therapy requirement. C.M. Dept of Thoracic Medicine, University Roberts, J.R. Bugler, R. Melcltor, M.R. Hetzel, S.G. Spiro. aRS Journals Ltd 1993. College Hospital, Gower Street, London, ABSTRACT: Pulse oximetry, combined with spirometry, was evaluated as a method UK. of selecting chronic obstructive pulmonary disease (COPD) out-patients requiring definitive arterial blood gas analysis for long-term oxygen therapy (LTO'I} assess· Correspondence: C.M. Roberts The Chest Clinic ment. A relatively blgb screening arterial oxygen saturation by pulse oximetry Whipps Cross Hospital (Sao ) level was set, In order to maximize sensitivity. London Ell Ail 113 COPD out-patients att.endlng the hospital clinic over a 6 month period UK wet-e screened. Sixty bad a forced expiratory volume In one second d.S I and 26 Keywords: Chronic obstructive pulmonary bad an Sao1 s92 %. These 26 underwent arterial blood gas analysis. Nine had an ) disease arterial oxygen tension <7 .3 kPa all with an arterial carbon dioxide tension (Paco1 >6 kPa. A further eight had a Pao <8 kPa. This produced a sensitivity or 100% hypoxaemia and speclftclty or 69% for oximetry fn the detectl.on of Pao <7.3 kPa detenn.lned by oxygen therapy 1 pulse oximetry direct arterial puncture and 100% and 86% respectively for detecting a Pao1 <8 kPa.