The Role of Tumor Necrosis Factor Alpha (TNF-)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dimerization of Ltβr by Ltα1β2 Is Necessary and Sufficient for Signal
Dimerization of LTβRbyLTα1β2 is necessary and sufficient for signal transduction Jawahar Sudhamsua,1, JianPing Yina,1, Eugene Y. Chiangb, Melissa A. Starovasnika, Jane L. Groganb,2, and Sarah G. Hymowitza,2 Departments of aStructural Biology and bImmunology, Genentech, Inc., South San Francisco, CA 94080 Edited by K. Christopher Garcia, Stanford University, Stanford, CA, and approved October 24, 2013 (received for review June 6, 2013) Homotrimeric TNF superfamily ligands signal by inducing trimers survival in a xenogeneic human T-cell–dependent mouse model of of their cognate receptors. As a biologically active heterotrimer, graft-versus-host disease (GVHD) (11). Lymphotoxin(LT)α1β2 is unique in the TNF superfamily. How the TNFRSF members are typically activated by TNFSF-induced three unique potential receptor-binding interfaces in LTα1β2 trig- trimerization or higher order oligomerization, resulting in initiation ger signaling via LTβ Receptor (LTβR) resulting in lymphoid organ- of intracellular signaling processes including the canonical and ogenesis and propagation of inflammatory signals is poorly noncanonical NF-κB pathways (2, 3). Ligand–receptor interactions α β understood. Here we show that LT 1 2 possesses two binding induce higher order assemblies formed between adaptor motifs in sites for LTβR with distinct affinities and that dimerization of LTβR the cytoplasmic regions of the receptors such as death domains or α β fi by LT 1 2 is necessary and suf cient for signal transduction. The TRAF-binding motifs and downstream signaling components such α β β crystal structure of a complex formed by LT 1 2,LT R, and the fab as Fas-associated protein with death domain (FADD), TNFR1- fragment of an antibody that blocks LTβR activation reveals the associated protein with death domain (TRADD), and TNFR-as- lower affinity receptor-binding site. -

The Unexpected Role of Lymphotoxin Β Receptor Signaling
Oncogene (2010) 29, 5006–5018 & 2010 Macmillan Publishers Limited All rights reserved 0950-9232/10 www.nature.com/onc REVIEW The unexpected role of lymphotoxin b receptor signaling in carcinogenesis: from lymphoid tissue formation to liver and prostate cancer development MJ Wolf1, GM Seleznik1, N Zeller1,3 and M Heikenwalder1,2 1Department of Pathology, Institute of Neuropathology, University Hospital Zurich, Zurich, Switzerland and 2Institute of Virology, Technische Universita¨tMu¨nchen/Helmholtz Zentrum Mu¨nchen, Munich, Germany The cytokines lymphotoxin (LT) a, b and their receptor genesis. Consequently, the inflammatory microenviron- (LTbR) belong to the tumor necrosis factor (TNF) super- ment was added as the seventh hallmark of cancer family, whose founder—TNFa—was initially discovered (Hanahan and Weinberg, 2000; Colotta et al., 2009). due to its tumor necrotizing activity. LTbR signaling This was ultimately the result of more than 100 years of serves pleiotropic functions including the control of research—indeed—the first observation that tumors lymphoid organ development, support of efficient immune often arise at sites of inflammation was initially reported responses against pathogens due to maintenance of intact in the nineteenth century by Virchow (Balkwill and lymphoid structures, induction of tertiary lymphoid organs, Mantovani, 2001). Today, understanding the underlying liver regeneration or control of lipid homeostasis. Signal- mechanisms of why immune cells can be pro- or anti- ing through LTbR comprises the noncanonical/canonical carcinogenic in different types of tumors and which nuclear factor-jB (NF-jB) pathways thus inducing cellular and molecular inflammatory mediators (for chemokine, cytokine or adhesion molecule expression, cell example, macrophages, lymphocytes, chemokines or proliferation and cell survival. -

Antagonist Antibodies Against Various Forms of BAFF: Trimer, 60-Mer, and Membrane-Bound S
Supplemental material to this article can be found at: http://jpet.aspetjournals.org/content/suppl/2016/07/19/jpet.116.236075.DC1 1521-0103/359/1/37–44$25.00 http://dx.doi.org/10.1124/jpet.116.236075 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 359:37–44, October 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Unexpected Potency Differences between B-Cell–Activating Factor (BAFF) Antagonist Antibodies against Various Forms of BAFF: Trimer, 60-Mer, and Membrane-Bound s Amy M. Nicoletti, Cynthia Hess Kenny, Ashraf M. Khalil, Qi Pan, Kerry L. M. Ralph, Julie Ritchie, Sathyadevi Venkataramani, David H. Presky, Scott M. DeWire, and Scott R. Brodeur Immune Modulation and Biotherapeutics Discovery, Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, Connecticut Received June 20, 2016; accepted July 18, 2016 Downloaded from ABSTRACT Therapeutic agents antagonizing B-cell–activating factor/B- human B-cell proliferation assay and in nuclear factor kB reporter lymphocyte stimulator (BAFF/BLyS) are currently in clinical assay systems in Chinese hamster ovary cells expressing BAFF development for autoimmune diseases; belimumab is the first receptors and transmembrane activator and calcium-modulator Food and Drug Administration–approved drug in more than and cyclophilin ligand interactor (TACI). In contrast to the mouse jpet.aspetjournals.org 50 years for the treatment of lupus. As a member of the tumor system, we find that BAFF trimer activates the human TACI necrosis factor superfamily, BAFF promotes B-cell survival and receptor. Further, we profiled the activities of two clinically ad- homeostasis and is overexpressed in patients with systemic vanced BAFF antagonist antibodies, belimumab and tabalumab. -

TRAIL and Cardiovascular Disease—A Risk Factor Or Risk Marker: a Systematic Review
Journal of Clinical Medicine Review TRAIL and Cardiovascular Disease—A Risk Factor or Risk Marker: A Systematic Review Katarzyna Kakareko 1,* , Alicja Rydzewska-Rosołowska 1 , Edyta Zbroch 2 and Tomasz Hryszko 1 1 2nd Department of Nephrology and Hypertension with Dialysis Unit, Medical University of Białystok, 15-276 Białystok, Poland; [email protected] (A.R.-R.); [email protected] (T.H.) 2 Department of Internal Medicine and Hypertension, Medical University of Białystok, 15-276 Białystok, Poland; [email protected] * Correspondence: [email protected] Abstract: Tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) is a pro-apoptotic protein showing broad biological functions. Data from animal studies indicate that TRAIL may possibly contribute to the pathophysiology of cardiomyopathy, atherosclerosis, ischemic stroke and abdomi- nal aortic aneurysm. It has been also suggested that TRAIL might be useful in cardiovascular risk stratification. This systematic review aimed to evaluate whether TRAIL is a risk factor or risk marker in cardiovascular diseases (CVDs) focusing on major adverse cardiovascular events. Two databases (PubMed and Cochrane Library) were searched until December 2020 without a year limit in accor- dance to the PRISMA guidelines. A total of 63 eligible original studies were identified and included in our systematic review. Studies suggest an important role of TRAIL in disorders such as heart failure, myocardial infarction, atrial fibrillation, ischemic stroke, peripheral artery disease, and pul- monary and gestational hypertension. Most evidence associates reduced TRAIL levels and increased TRAIL-R2 concentration with all-cause mortality in patients with CVDs. It is, however, unclear Citation: Kakareko, K.; whether low TRAIL levels should be considered as a risk factor rather than a risk marker of CVDs. -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

Commentary Mechanisms of Tumor Necrosis Factor Α Action On
Proc. Natl. Acad. Sci. USA Vol. 96, pp. 9449–9451, August 1999 Commentary Mechanisms of tumor necrosis factor ␣ action on neurodegeneration: Interaction with insulin-like growth factor-1 Sarah A. Loddick and Nancy J. Rothwell* School of Biological Sciences, University of Manchester, Manchester M13 9PT, United Kingdom The role of cytokines and growth factors in diverse forms of cause cell death when infused into a normal rodent brain, there neurodegeneration is now widely recognized. Several proin- is considerable evidence that TNF␣ mediates neuronal death flammatory cytokines, notably tumor necrosis factor (TNF) ␣ in an injured brain (e.g., ref. 9). Administration of exogenous and IL-1, have been shown to mediate diverse forms of TNF␣ markedly exacerbates ischemic injury in vivo (7) and, experimental neurodegeneration (1, 2), although in several most importantly, acute inhibition of TNF␣ action, by admin- cases both neurotoxic and neuroprotective actions have been istration of TNF soluble receptor (which prevents its action) (7, reported. Similarly numerous growth factors, including insu- 11) or a neutralizing antibody to TNF␣ (e.g., refs. 7 and 12) lin-like growth factor (IGF), fibroblast growth factor, trans- markedly attenuates ischemic brain damage in rat and mouse. forming growth factor , ciliary neurotrophic factor, vascular In contrast, studies in mice lacking TNF␣ receptor suggest endothelial growth factor, glia-derived neurotrophic factor, that TNF␣ may also have neuroprotective actions, mediated by brain-derived neurotrophic factor, nerve growth factor, and the p55 receptor (13, 14). Ischemic and excitotoxic injury is several neurotrophins have neuroprotective and͞or neurotro- greater in animals that lack either the p55 receptor or both phic actions in vivo and in vitro (e.g., refs. -
Report, Please Call the Telephone Number Listed
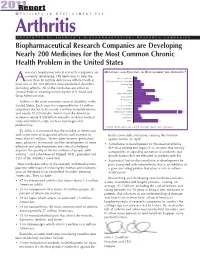
201R1e port M E D I C I N E S I N D E V E L O P M E N T F O R Arthritis P R E S E N T E D B Y A M E R I C A ’ S B I O P H A R M A C E U T I C A L R E S E A R C H C O M P A N I E S Biopharmaceutical Research Companies are Developing Nearly 200 Medicines for the Most Common Chronic Health Problem in the United States merica’s biopharmaceutical research companies are MEDICINES AND VACCINES IN DEVELOPMENT FOR ARTHRITIS* currently developing 198 medicines to help the Behcet’s Syndrome 3 more than 50 million Americans afflicted with at A Duchenne Muscular Dystrophy 6 least one of the 100 different musculoskeletal disorders, Fibromyalgia 9 including arthritis. All of the medicines are either in Gout 7 clinical trials or awaiting review by the U.S. Food and Lupus 19 Muscle Disorders 11 Drug Administration. Osteoarthritis 19 Osteoporosis 23 Arthritis is the most common cause of disability in the Pain 15 United States. Each year, it is responsible for 44 million Psoriatic Arthritis 7 outpatient doctor visits, nearly 1 million hospitalizations, Raynaud’s Disease 4 and nearly 10,000 deaths. And it costs the American Rheumatoid Arthritis 67 Scleroderma 6 economy nearly $128 billion annually in direct medical Spondylitis 7 costs and indirect costs, such as lost wages and Other 22 productivity. * Some medicines are listed in more than one category. -

MEDICAL JOURNAL Yongwen Jiang, Phd (USPS 464-820), a Monthly Publication, Is Deborah N
RHODE ISLAND M EDICAL J OURNAL Body Worlds Vital visits Rhode Island, page 66 R SPECIAL SECTION ADVANCES IN AUTOIMMUNE DISEASES GUEST EDITOR: EDWARD V. LALLY, MD DECember 2016 VOLUME 99 • NUMBER 12 ISSN 2327-2228 Your records are secure. Until they’re not. Data theft can happen to anyone, anytime. A misplaced mobile device can compromise your personal or patient records. RIMS IBC can get you the cyber liability insurance you need to protect yourself and your patients. Call us. 401-272-1050 IN COOPERATION WITH RIMS IBC RIMS INSURANCE BROKERAGE CORPORATION 405 PROMENADE STREET, SUITE B, PROVIDENCE RI 02908-4811 MEDICAL PROFESSIONAL/ CYBER LIABILITY PROPERTY/ CASUALTY LIFE/HEALTH/ DISABILITY RHODE ISLAND M EDICAL J OURNAL 18 Newer Treatment Strategies for Autoimmune Diseases EDWARD V. LALLY, MD GUEST EDITOR E. Lally, MD 19 Targeted Immunomodulatory Therapy: An Overview ASHLEY L. LEFEBVRE, PharmD, CDOE LAURA MCAULIFFE, PharmD: PGY2 23 Systemic Lupus Erythematosus: A. Lefebvre, PharmD A Review of the Clinical Approach to Diagnosis and Update on Current Targeted Therapies JOANNE SZCZYGIEL CUNHA, MD KATARZYNA GILEK-SEIBERT, MD J. Cunha, MD 28 Pemphigus: Pathogenesis to Treatment K. Gilek-Siebert, MD CHRISTOPHER DIMARCO, MD 32 Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP): C. DiMarco, MD Clinical Features, Diagnosis, and Current Treatment Strategies JACQUES REYNOLDS, DO GEORGE SACHS, MD, PhD G. Sachs, MD, PhD KARA STavROS, MD 36 Autoimmune Cytopenias: Diagnosis & Management CHRISTIAN P. NIXON, MD, PhD JOSEPH D. SWEENEY, MD C. Nixon, MD, PhD RHODE ISLAND M EDICAL J OURNAL 8 COMMENTARY Medical Tourism JOSEPH H. FRIEDMAN, MD Dickensian Diagnostics: The Diseases of Christmas Past What ailed Scrooge and Tiny Tim? HERBERT RAKATANSKY, MD Reconnecting with my Purpose in the Kingdom of Bhutan ERIC COHEN, MD 17 RIMJ AROUND THE WORLD New York, New York 58 RIMS NEWS Are you reading RIMS Notes? Working for You Weight + Wellness Summit Why You Should Join RIMS 66 SPOTLIGHT Body Worlds Exhibit: Anatomy Up Close & Personal MARY KORR 78 HeritaGE Dec. -

Immunfarmakológia Immunfarmakológia
Gergely: Immunfarmakológia Immunfarmakológia Prof Gergely Péter Az immunpatológiai betegségek döntő többsége gyulladásos, és ennek következtében általában szövetpusztulással járó betegség, melyben – jelenleg – a terápia alapvetően a gyulladás csökkentésére és/vagy megszűntetésére irányul. Vannak kizárólag gyulladásgátló gyógyszereink és vannak olyanok, amelyek az immunreakció(k) bénításával (=immunszuppresszió révén) vagy emellett vezetnek a gyulladás mérsékléséhez. Mind szerkezetileg, mind hatástanilag igen sokféle csoportba oszthatók, az alábbi felosztás elsősorban didaktikus célokat szolgál. 1. Nem-szteroid gyulladásgátlók (‘nonsteroidal antiinflammatory drugs’ NSAID) 2. Kortikoszteroidok 3. Allergia-elleni szerek (antiallergikumok) 4. Sejtoszlás-gátlók (citosztatikumok) 5. Nem citosztatikus hatású immunszuppresszív szerek 6. Egyéb gyulladásgátlók és immunmoduláns szerek 7. Biológiai terápia 1. Nem-szteroid gyulladásgátlók (NSAID) Ezeket a vegyületeket, melyek őse a szalicilsav (jelenleg, mint acetilszalicilsav ‘aszpirin’ használatos), igen kiterjedten alkalmazzák a reumatológiában, az onkológiában és az orvostudomány szinte minden ágában, ahol fájdalom- és lázcsillapításra van szükség. Egyes felmérések szerint a betegek egy ötöde szed valamilyen NSAID készítményt. Szerkezetük alapján a készítményeket több csoportba sorolhatjuk: szalicilátok (pl. acetilszalicilsav) pyrazolidinek (pl. fenilbutazon) ecetsav származékok (pl. indometacin) fenoxiecetsav származékok (pl. diclofenac, aceclofenac)) oxicamok (pl. piroxicam, meloxicam) propionsav -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -

The Recent History of Tumour Necrosis Factor (Tnf)
THE RECENT HISTORY OF TUMOUR NECROSIS FACTOR (TNF) The transcript of a Witness Seminar held by the History of Modern Biomedicine Research Group, Queen Mary University of London, on 14 July 2015 Edited by A Zarros, E M Jones, and E M Tansey Volume 60 2016 ©The Trustee of the Wellcome Trust, London, 2016 First published by Queen Mary University of London, 2016 The History of Modern Biomedicine Research Group is funded by the Wellcome Trust, which is a registered charity, no. 210183. ISBN 978 1 91019 5208 All volumes are freely available online at www.histmodbiomed.org Please cite as: Zarros A, Jones E M, Tansey E M. (eds) (2016) The Recent History of Tumour Necrosis Factor (TNF). Wellcome Witnesses to Contemporary Medicine, vol. 60. London: Queen Mary University of London. CONTENTS What is a Witness Seminar? v Acknowledgements E M Tansey and A Zarros vii Illustrations and credits ix Abbreviations xi Introduction Professor Jon Cohen xv Transcript Edited by A Zarros, E M Jones, and E M Tansey 1 Appendix 1 Timeline of important events in the history of TNF 73 Appendix 2 Simplified overview of the main biological actions of TNF in rheumatoid arthritis 75 Appendix 3 Overview of TNF inhibitors mentioned in the current Witness Seminar transcript 77 Glossary 79 Biographical notes 83 References 93 Index 105 Witness Seminars: Meetings and publications 111 WHAT IS A WITNESS SEMINAR? The Witness Seminar is a specialized form of oral history, where several individuals associated with a particular set of circumstances or events are invited to meet together to discuss, debate, and agree or disagree about their memories. -

WO 2016/176089 Al 3 November 2016 (03.11.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/176089 Al 3 November 2016 (03.11.2016) P O P C T (51) International Patent Classification: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, A01N 43/00 (2006.01) A61K 31/33 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, (21) International Application Number: KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, PCT/US2016/028383 MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (22) International Filing Date: PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, 20 April 2016 (20.04.2016) SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of regional protection available): ARIPO (BW, GH, (30) Priority Data: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, 62/154,426 29 April 2015 (29.04.2015) US TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, (71) Applicant: KARDIATONOS, INC. [US/US]; 4909 DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, Lapeer Road, Metamora, Michigan 48455 (US).