Impact of Β-Galactomannan on Health Status and Immune Function in Rats Leeann Schalinske Iowa State University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Isolation, Characterization, and Medicinal Potential of Polysaccharides of Morchella Esculenta
molecules Article Isolation, Characterization, and Medicinal Potential of Polysaccharides of Morchella esculenta Syed Lal Badshah 1,* , Anila Riaz 1, Akhtar Muhammad 1, Gülsen Tel Çayan 2, Fatih Çayan 2, Mehmet Emin Duru 2, Nasir Ahmad 1, Abdul-Hamid Emwas 3 and Mariusz Jaremko 4,* 1 Department of Chemistry, Islamia College University Peshawar, Peshawar 25120, Pakistan; [email protected] (A.R.); [email protected] (A.M.); [email protected] (N.A.) 2 Department of Chemistry and Chemical Processing Technologies, Mu˘glaVocational School, Mu˘glaSıtkı Koçman University, 48000 Mu˘gla,Turkey; [email protected] (G.T.Ç.); [email protected] (F.Ç.); [email protected] (M.E.D.) 3 Core Labs, King Abdullah University of Science and Technology (KAUST), Thuwal 23955-6900, Saudi Arabia; [email protected] 4 Division of Biological and Environmental Sciences and Engineering (BESE), King Abdullah University of Science and Technology (KAUST), Thuwal 23955-6900, Saudi Arabia * Correspondence: [email protected] (S.L.B.); [email protected] (M.J.) Abstract: Mushroom polysaccharides are active medicinal compounds that possess immune-modulatory and anticancer properties. Currently, the mushroom polysaccharides krestin, lentinan, and polysac- Citation: Badshah, S.L.; Riaz, A.; charopeptides are used as anticancer drugs. They are an unexplored source of natural products with Muhammad, A.; Tel Çayan, G.; huge potential in both the medicinal and nutraceutical industries. The northern parts of Pakistan have Çayan, F.; Emin Duru, M.; Ahmad, N.; a rich biodiversity of mushrooms that grow during different seasons of the year. Here we selected an Emwas, A.-H.; Jaremko, M. Isolation, edible Morchella esculenta (true morels) of the Ascomycota group for polysaccharide isolation and Characterization, and Medicinal characterization. -

United States Patent (10) Patent No.: US 9,572,364 B2 Langan Et Al
USOO9572364B2 (12) United States Patent (10) Patent No.: US 9,572,364 B2 Langan et al. (45) Date of Patent: *Feb. 21, 2017 (54) METHODS FOR THE PRODUCTION AND 6,490,824 B1 12/2002 Intabon et al. USE OF MYCELIAL LIQUID TISSUE 6,558,943 B1 5/2003 Li et al. CULTURE 6,569.475 B2 5/2003 Song 9,068,171 B2 6/2015 Kelly et al. (71) Applicant: Mycotechnology, Inc., Aurora, CO 2002.01371.55 A1 9, 2002 Wasser et al. (US) 2003/0208796 Al 11/2003 Song et al. (72) Inventors: James Patrick Langan, Denver, CO 3988: A. 58: sistset al. (US); Brooks John Kelly, Denver, CO 2004f02.11721 A1 10, 2004 Stamets (US); Huntington Davis, Broomfield, 2005/0180989 A1 8/2005 Matsunaga CO (US); Bhupendra Kumar Soni, 2005/0255126 A1 11/2005 TSubaki et al. Denver, CO (US) 2005/0273875 A1 12, 2005 Elias s 2006/0014267 A1 1/2006 Cleaver et al. (73) Assignee: MYCOTECHNOLOGY, INC., Aurora, 2006/0134294 A1 6/2006 McKee et al. CO (US) 2006/0280753 A1 12, 2006 McNeary (*) Notice: Subject to any disclaimer, the term of this 2007/O160726 A1 T/2007 Fujii patent is extended or adjusted under 35 (Continued) U.S.C. 154(b) by 0 days. FOREIGN PATENT DOCUMENTS This patent is Subject to a terminal dis claimer. CN 102860541. A 1, 2013 DE 4341316 6, 1995 (21) Appl. No.: 15/144,164 (Continued) (22) Filed: May 2, 2016 OTHER PUBLICATIONS (65) Prior Publication Data Diekman "Sweeteners Facts and Fallacies: Learn the Truth About US 2016/0249660 A1 Sep. -
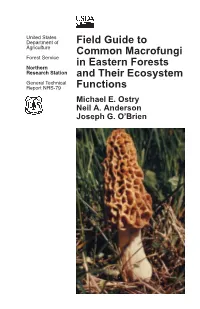
Field Guide to Common Macrofungi in Eastern Forests and Their Ecosystem Functions
United States Department of Field Guide to Agriculture Common Macrofungi Forest Service in Eastern Forests Northern Research Station and Their Ecosystem General Technical Report NRS-79 Functions Michael E. Ostry Neil A. Anderson Joseph G. O’Brien Cover Photos Front: Morel, Morchella esculenta. Photo by Neil A. Anderson, University of Minnesota. Back: Bear’s Head Tooth, Hericium coralloides. Photo by Michael E. Ostry, U.S. Forest Service. The Authors MICHAEL E. OSTRY, research plant pathologist, U.S. Forest Service, Northern Research Station, St. Paul, MN NEIL A. ANDERSON, professor emeritus, University of Minnesota, Department of Plant Pathology, St. Paul, MN JOSEPH G. O’BRIEN, plant pathologist, U.S. Forest Service, Forest Health Protection, St. Paul, MN Manuscript received for publication 23 April 2010 Published by: For additional copies: U.S. FOREST SERVICE U.S. Forest Service 11 CAMPUS BLVD SUITE 200 Publications Distribution NEWTOWN SQUARE PA 19073 359 Main Road Delaware, OH 43015-8640 April 2011 Fax: (740)368-0152 Visit our homepage at: http://www.nrs.fs.fed.us/ CONTENTS Introduction: About this Guide 1 Mushroom Basics 2 Aspen-Birch Ecosystem Mycorrhizal On the ground associated with tree roots Fly Agaric Amanita muscaria 8 Destroying Angel Amanita virosa, A. verna, A. bisporigera 9 The Omnipresent Laccaria Laccaria bicolor 10 Aspen Bolete Leccinum aurantiacum, L. insigne 11 Birch Bolete Leccinum scabrum 12 Saprophytic Litter and Wood Decay On wood Oyster Mushroom Pleurotus populinus (P. ostreatus) 13 Artist’s Conk Ganoderma applanatum -

Fungal Diversity in the Mediterranean Area
Fungal Diversity in the Mediterranean Area • Giuseppe Venturella Fungal Diversity in the Mediterranean Area Edited by Giuseppe Venturella Printed Edition of the Special Issue Published in Diversity www.mdpi.com/journal/diversity Fungal Diversity in the Mediterranean Area Fungal Diversity in the Mediterranean Area Editor Giuseppe Venturella MDPI • Basel • Beijing • Wuhan • Barcelona • Belgrade • Manchester • Tokyo • Cluj • Tianjin Editor Giuseppe Venturella University of Palermo Italy Editorial Office MDPI St. Alban-Anlage 66 4052 Basel, Switzerland This is a reprint of articles from the Special Issue published online in the open access journal Diversity (ISSN 1424-2818) (available at: https://www.mdpi.com/journal/diversity/special issues/ fungal diversity). For citation purposes, cite each article independently as indicated on the article page online and as indicated below: LastName, A.A.; LastName, B.B.; LastName, C.C. Article Title. Journal Name Year, Article Number, Page Range. ISBN 978-3-03936-978-2 (Hbk) ISBN 978-3-03936-979-9 (PDF) c 2020 by the authors. Articles in this book are Open Access and distributed under the Creative Commons Attribution (CC BY) license, which allows users to download, copy and build upon published articles, as long as the author and publisher are properly credited, which ensures maximum dissemination and a wider impact of our publications. The book as a whole is distributed by MDPI under the terms and conditions of the Creative Commons license CC BY-NC-ND. Contents About the Editor .............................................. vii Giuseppe Venturella Fungal Diversity in the Mediterranean Area Reprinted from: Diversity 2020, 12, 253, doi:10.3390/d12060253 .................... 1 Elias Polemis, Vassiliki Fryssouli, Vassileios Daskalopoulos and Georgios I. -

Screening of Edible Mushrooms and Extraction by Pressurized Water
1 Screening of edible mushrooms and extraction by pressurized 2 water (PWE) of 3-hydroxy-3-methyl-glutaryl CoA reductase 3 inhibitors 4 5 Alicia Gil-Ramíreza*, Cristina Clavijob, Marimuthu Palanisamya, Alejandro Ruíz-Rodrígueza, 6 María Navarro-Rubioa, Margarita Pérezb, Francisco R. Marína, Guillermo Regleroa, Cristina 7 Soler-Rivasa 8 9 aDepartment of Production and Characterization of New Foods. CIAL -Research Institute in Food Science 10 (UAM+CSIC). Madrid. Spain. 11 bCentro Tecnológico de Investigación del Champiñón de La Rioja (CTICH). Autol. Spain 12 13 * corresponding author: Alicia Gil-Ramírez. Department of Production and Characterization of New Foods. 14 CIAL -Research Institute in Food Science (UAM+CSIC). 28049 Madrid (Spain). E-mail address: 15 [email protected]. Tel: +34 910017900 16 17 18 19 20 21 22 23 24 25 1 1 ABSTRACT 2 3 The methanol/water and particularly the water extracts obtained from 26 mushroom species 4 were able to inhibit the 3-hydroxy-3-methyl-glutaryl CoA reductase (HMGCR) activity to 5 different extent (10 to 76%). Cultivated mushrooms such as Pleurotus sp. and Lentinula 6 edodes were among the strains which showed higher HMGCR inhibitory capacities. Their 7 inhibitory properties were not largely influenced by cultivation parameters, mushroom 8 developmental stage or flush number. The HMGCR inhibitory activity of L. edodes was 9 concentrated in the cap excluding the gills while in P. ostreatus it was distributed through all 10 the different tissues. A method to obtain aqueous fractions with high HMGCR inhibitory 11 activity was optimized using an accelerated solvent extractor (ASE) by selecting 10.7 MPa 12 and 25ºC as common extraction conditions and 5 cycles of 5 min each for P. -

Mushroom Highlights Newsletter
April 2016 - Mushroom Highlights Newsletter for Wild Mushrooms PNW ❖ www.wildmushroomspnw.com Can Fungi Survive on Mars? An experiment conducted on the international space station found that even after 18 months on board, more than 60% of the fungi’s cells remained intact. The samples used were from the genus Cryomyces and came from remote and hostile areas on the Earth to see if they could also survive extreme environments beyond our planet, and they did. (from earthsky.org) Fungi Create Raindrops Mushroom spores are released into the atmosphere every day by the billions. This amounts to 50 million tons each year. Together with pollen, bacteria, and other biological particles, they serve as nuclei for cloud formation, and therefore rain. (extracted from NAMA March/April 2016 – Elio Schaechter) How Fast and How Far Can a Spore Fly? On the underside of some mushroom caps there are gills or pores. Because of internal pressure from maturing spores and humidity, the contents of asci (tubes where spores are formed) can simultaneously eject spores into the air with an initial velocity of close to 7 feet/second. This is sustained only for a brief time or the spores would hit the opposite gills. Since they cannot overcome the viscosity of air, they drop vertically to be caught by air current and may be carried a long distance. Sphaerobolus stellatus (Cannonball Fungus) can travel over a 20 foot horizontal and a 7 foot vertical distance. (extracted from NAMA March/April 2016 – Elio Schaechter) When is a Mushroom Important? You found a mushroom and just can’t identify it. -

Morchella Esculenta</Em>
Journal of Bioresource Management Volume 3 Issue 1 Article 6 In Vitro Propagation of Morchella esculenta and Study of its Life Cycle Nazish Kanwal Institute of Natural and Management Sciences, Rawalpindi, Pakistan Kainaat William Bioresource Research Centre, Islamabad, Pakistan Kishwar Sultana Institute of Natural and Management Sciences, Rawalpindi, Pakistan Follow this and additional works at: https://corescholar.libraries.wright.edu/jbm Part of the Biodiversity Commons, and the Biology Commons Recommended Citation Kanwal, N., William, K., & Sultana, K. (2016). In Vitro Propagation of Morchella esculenta and Study of its Life Cycle, Journal of Bioresource Management, 3 (1). DOI: https://doi.org/10.35691/JBM.6102.0044 ISSN: 2309-3854 online This Article is brought to you for free and open access by CORE Scholar. It has been accepted for inclusion in Journal of Bioresource Management by an authorized editor of CORE Scholar. For more information, please contact [email protected]. In Vitro Propagation of Morchella esculenta and Study of its Life Cycle © Copyrights of all the papers published in Journal of Bioresource Management are with its publisher, Center for Bioresource Research (CBR) Islamabad, Pakistan. This permits anyone to copy, redistribute, remix, transmit and adapt the work for non-commercial purposes provided the original work and source is appropriately cited. Journal of Bioresource Management does not grant you any other rights in relation to this website or the material on this website. In other words, all other rights are reserved. For the avoidance of doubt, you must not adapt, edit, change, transform, publish, republish, distribute, redistribute, broadcast, rebroadcast or show or play in public this website or the material on this website (in any form or media) without appropriately and conspicuously citing the original work and source or Journal of Bioresource Management’s prior written permission. -

Characterization of Lipoxygenase Activity from a Partially Purified
Process Biochemistry 36 (2000) 1–7 www.elsevier.com/locate/procbio Characterization of lipoxygenase activity from a partially purified enzymic extract from Morchella esculenta Barbara Bisakowski a, Avtar S. Atwal a,*, Selim Kermasha b a Food Research and De6elopment Center, Agriculture and Agri-Food Canada, 3600, Bl6d. Casa6ant West, St-Hyacinth, Que´bec, Canada J2S 8E3 b Department of Food Science and Agricultural Chemistry, McGill Uni6ersity, 21 111 Lakeshore, Ste Anne de Belle6ue, Que´bec, Canada H9X 3V9 Received 22 November 1999; received in revised form 29 February 2000; accepted 3 March 2000 Abstract A crude extract (FI) from Morchella esculenta was partially purified using ammonium sulphate precipitation at 0–60, 60–80 and 80–100% of saturation to obtain fractions (FIIa), (FIIb) and (FIIc), respectively. The highest specific lipoxygenase (LOX) activity was obtained in fraction (FIIa) which showed a recovery of 12.8% and a 2.5-fold increase in purification. Partially purified LOX extract exhibited optimal activity at the acidic pH of 3.0 and showed 62.5% of the maximal activity in the pH range of 4.0–6.0 and less than 12.5% activity in the pH range of 7.0–10.0. Kinetic studies indicated that the LOX activity of fraction (FIIa) m −1 −1 −4 had a Vmax of 0.314 mol hydroperoxide mg protein min and a corresponding Km value of 1.59×10 M. The enzymic activity exhibited a strong specificity towards linoleic acid as substrate while only 29% activity was observed using linolenic acid and approximately 11% was obtained with mono-, di- and trilinolein; however, LOX activity showed a relatively strong affinity (83%) towards arachidonic acid as substrate. -

Mushrooms in Your Garden
Janel K. Baran, 6000 Portr Rd NE Blue Owl Holow Newark, OH 43055 740-345-4689 htp://www.blueowlgarden.com/ Resources for Growing Mushrooms in the Garden Species readily available on-line: Name Preferred substrates Fruiting season Sources Almond Agaricus manure or rich compost, prefers a companion 70-95°F (not hardy) F&F Agaricus subrufescens crop, e.g., tomato, squash, melon, potato summer Blewit hardwood & pine duff mixed with organic matter 40-65°F F&F Clitocybe nuda aka Lepista nuda fall Shaggy Mane lawns, meadows, wood chips, barnyards, manure- 40-60°F FP Coprinus comatus enriched soils, manure/sawdust beddding spring & fall Reishi/Ling Chi hardwood stumps and partially-buried logs; esp. 60-95°F, FP, F&F, Ganoderma lucidum oak, elm, maple; pony logs summer & early fall MP Maitake/Hen of the Woods hardwood stumps or buried logs; esp. oak, honey 45-70°F FP, F&F, Grifola frondosa locust, elm, black gum, beech, maple fall MP Lion's Mane thick-barked hardwood stumps or partially buried 60-75°F FP, F&F, Hericium erinaceus logs; esp. oak, elm, hard maple, walnut, sycamore summer MP Elm Oyster Stumps or partially-buried logs of elm, beech, 50-70°F FP Hypsizygus ulmarius maple, willow, oak; woodchip/sawdust beds summer & fall Shiitake thick-barked hardwood logs and stumps, e.g., oak, 50-80°F FP, F&F, Lentinula edodes ash, beech, hickory, hard maple spring, summer, fall MP Morel, Black burn sites; sand-wood ash-gypsum-gravel-wood 45-65°F FP, F&F, Morchella angusticeps charcoal beds, over-seed w/native grasses spring MP Morel, White wood-based mulch beds in old orchards or woods; 45-65°F FP, F&F Morchella esculenta among perennial veggies in a mix of partially spring decomposed organic matter, wood chips & soil Oyster hardwood and softwood stumps and logs,esp. -

Diversity, Characterization and Nutritional Status of Wild Edible and Medicinal Mushrooms of Sikkim
Wangdi Int. J. Pure App. Biosci. 7 (2): 327-334 (2019) ISSN: 2320 – 7051 Available online at www.ijpab.com DOI: http://dx.doi.org/10.18782/2320-7051.7421 ISSN: 2320 – 7051 Int. J. Pure App. Biosci. 7 (2): 327-334 (2019) Research Article Diversity, Characterization and Nutritional Status of Wild Edible and Medicinal Mushrooms of Sikkim Lhanjey P. Wangdi* Deptartment of Botany, Sikkim Government College, Tadong (Renamed: NBBDC, Tadong) Gangtok, Sikkim-737102 *Corresponding Author E-mail: [email protected] Received: 5.03.2019 | Revised: 10.04.2019 | Accepted: 17.04.2019 ABSTRACT Wild edible mushroom species are used since ancient time for their unique taste and extraordinary health enhancing bioactive compounds. Mushrooms are also a class of superfoods created from the actual fruiting body as well as the mycelium biomass. With the aim to study the diversity, nutritional content and identification of some wild edible mushrooms of Sikkim, the fungal cultures were isolated from the tissue taken from their basidiocarps, using moist chamber method. On the basis of available literature the fungi were identified by matching their characteristics like external morphology and anatomical features. Eleven different species of wild edible mushrooms namely; Laetiporus sulphurous, Polyporus guianensis, Pseudohydnum gelatinosum, Grifola frondosa, Pholiota nameko, Morchella crasspes, Auriculariacornea, Lentinula edodes, Pholiota sp., Schizophyllum commune and Trametes sanguinea were selected for detailed study. The nutritional contents of the mushrooms were analysed in terms of moisture, protein and carbohydrate (sugar) contents. The present study describes the existing situation of the wild mushrooms of Sikkim and putting emphasis on ecological effects of harvest. The results could be a valuable documentation for scientific community in domestication or cultivation of wild mushroom for nutritional and medicinal purpose. -

Wild Edible Mushrooms from High Elevations in the Garhwal Himalaya-I
Current Research in Environmental & Applied Mycology 6 (2): 118–131(2016) ISSN 2229-2225 www.creamjournal.org Article CREAM Copyright © 2016 Online Edition Doi 10.5943/cream/6/2/6 Wild edible mushrooms from high elevations in the Garhwal Himalaya-I Bhatt RP1, Singh U1* and Stephenson SL2 1Department of Botany & Microbiology, H.N.B. Garhwal University (A Central University), Srinagar, Garhwal, 246174, Uttarakhand, India 2Department of Biological Sciences, University of Arkansas, Fayetteville, Arkansas, 7270, USA Bhatt RP, Singh U, Stephenson SL. 2016 – Wild edible mushrooms from high elevations in the Garhwal Himalaya-I. Current Research in Environmental & Applied Mycology 6(1), 118–131, Doi 10.5943/cream/6/2/6 Abstract Information is provided on 15 species of wild edible mushrooms collected at elevations of 2000−3500 masl in the Garhwal Himalaya of Northern India. Except for Morchella esculenta (‗Guchhi‘), which is a member of the ascomycetes, all of the other macrofungi considered herein are basidiomycetes. The 15 species belong to 12 genera and 08 families and were collected from 08 different study sites in the Garhwal Himalaya. Key words – Ascomycetes – Basidiomycetes – macrofungi − Northern India Introduction Wild mushrooms have been eaten by mankind since time immemorial. Their use in Indian literature dates back to 3000 B.C. They were highly prized by the Greeks, and the consumption of mushrooms in European nations has deep traditional roots. Edible mushrooms are considered one of the world‘s greatest natural resources since they have the ability to transform nutritionally valueless substances into high protein foods. Mushrooms are highly valued for their rich characteristic flavour, delicate taste and potent nutritional properties. -

Auricularia Auricula Pg
© Symbiosis The newsletter of the Prairie States Mushroom Club Volume 26:1 Spring 2009 http://www.geocities.com/iowamushroom Mushrooms and Anti-Semitism Information compiled by Dean Abel Dean Abel noticed the anti-Semitic “Propaganda and Children during the tract Der Giftpilz for sale on eBay Hitler Years”. <www.nizkor.org/hweb/ and he sought out more information. people/m/mills-mary/mills-00.html>. However, he was scooped by David W. Rose in the article “Auricularia She writes: “Der Giftpilz (The auricula, Anti-Semitism, and Political Poisonous Mushroom) appeared in Mushrooms” in the new magazine Germany in 1938 and leaves little Fungi. Rose’s article examines Der question regarding the intended Nazi Giftpilz and other Nazi propaganda solution to the “Jewish problem.” The employing mushroom metaphors as book begins innocently enough by well as discussing the history of the describing a favorite German pastime, “Jew’s Ear” mushroom. Visit the picking wild mushrooms in the woods. homepage of Fungi at A young boy, Franz, accompanies his www.fungimag.com. Some current mother on a walk in a beautiful, articles may be downloaded. wooded area and helps her gather mushrooms. After carefully describing In any case, here is what Dean and showing Franz several varieties of gleaned from the website both edible and poisonous www.calvin.edu/academic/cas/gpa/ mushrooms, his mother compares the thumb.htm. good mushrooms to good people and the harmful mushrooms to bad Der Giftpilz, the German word for people. The most dangerous people toadstool, was a publication of Julius are, of course, the Jews.