Intimate Partner Violence and Communication of HIV Diagnosis in Rakai, Uganda
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations from the AIDS Support Organization (TASO) in the Teso Region Emma Smith SIT Study Abroad
SIT Graduate Institute/SIT Study Abroad SIT Digital Collections Independent Study Project (ISP) Collection SIT Study Abroad Spring 2008 HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations From The AIDS Support Organization (TASO) in the Teso Region Emma Smith SIT Study Abroad Follow this and additional works at: https://digitalcollections.sit.edu/isp_collection Recommended Citation Smith, Emma, "HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations From The AIDS Support Organization (TASO) in the Teso Region" (2008). Independent Study Project (ISP) Collection. 99. https://digitalcollections.sit.edu/isp_collection/99 This Unpublished Paper is brought to you for free and open access by the SIT Study Abroad at SIT Digital Collections. It has been accepted for inclusion in Independent Study Project (ISP) Collection by an authorized administrator of SIT Digital Collections. For more information, please contact [email protected]. HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations from The AIDS Support Organization (TASO) in the Teso Region Emma Smith Advisor: Alutia Samuel Academic Directors: Charlotte Mafumbo and Martha Wandera Location: TASO Soroti SIT Uganda Spring 2008 Dedication To all the people living with HIV/AIDS in Teso, who continue to live strongly despite decades of suffering from continuous war, displacement and neglect. May the world come to recognize the struggles that you live with. Acknowledgements There are so many people to whom thanks is owed, it would not be possible to acknowledge them all even if time and space allowed. Primarily, I would like to thank the clients of TASO Soroti, who so willingly welcomed a stranger into their communities and allowed so many questions to be asked of them. -

Intimate Partner Violence As a Predictor of Marital Disruption in Rural Rakai, Uganda: a Longitudinal Study
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by eScholarship - University of California UCLA UCLA Previously Published Works Title Intimate partner violence as a predictor of marital disruption in rural Rakai, Uganda: a longitudinal study. Permalink https://escholarship.org/uc/item/2kz5x57n Journal International journal of public health, 61(8) ISSN 1661-8556 Authors Wagman, Jennifer A Charvat, Blake Thoma, Marie E et al. Publication Date 2016-11-01 DOI 10.1007/s00038-016-0891-z Peer reviewed eScholarship.org Powered by the California Digital Library University of California See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/308047420 Intimate partner violence as a predictor of marital disruption in rural Rakai, Uganda: a longitudinal study Article in International Journal of Public Health · September 2016 DOI: 10.1007/s00038-016-0891-z CITATIONS READS 7 161 11 authors, including: Jennifer Wagman Marie Thoma University of California Los Angeles Fielding School of Public Health University of Maryland, College Park 51 PUBLICATIONS 1,343 CITATIONS 49 PUBLICATIONS 1,094 CITATIONS SEE PROFILE SEE PROFILE Anthony Ndyanabo Fredrick Nalugoda Rakai Health Sciences Program Rakai Health Sciences Program 41 PUBLICATIONS 877 CITATIONS 265 PUBLICATIONS 11,819 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: Mucosal HIV Susceptibility View project ALPHA Network View project All content following this page was uploaded by Jennifer Wagman on 31 March 2018. The user has requested enhancement of the downloaded file. Int J Public Health DOI 10.1007/s00038-016-0891-z ORIGINAL ARTICLE Intimate partner violence as a predictor of marital disruption in rural Rakai, Uganda: a longitudinal study Jennifer A. -

Program of the 4Th Scientific Conference
Makerere University College of Health Sciences Program for the 7th Annual Scientific Conference 20th – 22nd September 2011; Speke Resort Munyonyo Kampala, Uganda 20th SEPTEMBER 2011 Abstract No. Time Presentation 8.00-8.30 Arrival and registration PLENARY Chair: Dr Rhoda Wanyenze; Co-Chair: Dr. Freddie Bwanga 8.30 - 9.00 Key note address – All for Health – One Health: Dr. Jane Aceng Director General MOH PLENARY Health Systems, Health Policy & Healthcare Chair: Prof Fredrick Wabwire-Mangen; Co-Chair: Prof. David Guwatudde PP1001_20 9.00-9.10 Health Systems, Governance and Health Outcome: Dr. Freddie Ssengoba PP1002_20 9.10-9.20 Challenges and Future Systems in Uganda to Ensure Delivery of Quality Care: Dr. Robert Basaza PP1003_20 9.20-9.30 Transforming Education to Strengthen Health Systems in an Inter-department World: Prof. David Serwadda 9.30-9:40 DISCUSSION PP1004_20 9:40-9:50 Role of Cultural Institutions in Healthcare Delivery, Disease Prevention and Health Promotion: Dr. Nelson Kawalya PP1005_20 9:50-10:00 Impact of Private for Profit Institutions in Healthcare Delivery and Health Systems Strengthening: Dr. Ian Clarke PP1006_20 10:00-10:10 HIV/AIDS programming through District based technical assistance programme: Experience from STAR-EC: Dr. Samson Kironde 10:10-10:20 DISCUSSION 10:20-10:50 TEA BREAK OFFICIAL OPENING CEREMONY: MC – Prof. Harriet Mayanja; Co-MC: Mr. Gerald Makumbi 10:50-10.55 Welcome remarks by Chair, 7ASC Organising Committee MakCHS: Dr. Freddie Bwanga 10.55-11.10 Announcement of the Bill & Melinda Gates Research Grant for Africa: Dr. Wong 11.10-11.10 Remarks on Translating Research into Policy and Healthcare Delivery by Chair, Research College of Health Sciences Makerere University: Prof. -
Annual Report 2010
ANNUAL REPORT 2010 * Listening * Telling true stories * Addressing adolescent and adult sexuality In 2010 STF sadly said farewell to Charlotte Kanstrup when she returned to Copenhagen. Seen above with clients at Gulu Youth Centre, Charlotte was Counsellor of Development at Danida in Kampala from 2005 to 2010. She was an ardent supporter of STF’s model, and STF is immensely grateful for the guidance she provided. ABBREVIAtions Straight Talk radio shows capture deeply private moments. STF Board of DIRECTORS AMYC Amuru Youth center Interviews are conducted in huts, AJYC Ajumani Youth Center classsrooms, clinics and small ARVs Anti Retrovirals living rooms and under trees. BCC Behaviour Change Communication They are assembled into shows CCTs Centre Coordinating Tutors in STF’s Kampala studio. CSF Civil Society Fund DATIC District Agricultural Training and Information Center DEOs District Education Officers Straight Talk Foundation (STF) is a Ugandan NGO, DHOs District Health Officers set up in 1997. It grew out of a teen newspaper, Chair: Aggrey Charles Odere, Rev Gideon GYC Gulu Youth Center Straight Talk, started in 1993. Today it practises Kibenge, Under Advocate, Lex Uganda Byamugisha, FGD Focus Group Discussion COMMunicAtion foR SociAL CHAngE. Secretary, MoES Christian Aid HCT HIV Counseling and Testing IPPF International Planned Parenthood Federation Its main focus is PREVEnting HIV in KYC Kitgum Youth Center ADOLEscEnts. MoES Ministry of Education and Sports MOU Memorandum of Understanding STF also supports PAREnts and TEACHERS NUREP Northern Uganda Rehabilitation Program to have safer and healthier sexual lives and to help PACE Programs for Accessible Health , Communication and Education PIASCY Presidential Initiative on AIDS Strategy for Communication to Youth adolescent have safer transitions to adulthood. -

Serena Hotel and Conference Centre Kampala, Uganda May 26–27, 2011 Table of Contents
Program Serena Hotel and Conference Centre Kampala, Uganda MAY 26–27, 2011 Table of Contents Welcome Letter . 3 Acknowledgements . 4 General Information . 5 Agenda . 9 u Wednesday, May 25, 2011 . 9 u Thursday, May 26, 2011 . 9 u Friday, May 27, 2011 . .11 Conference Centre Floor Plan . 13 Abstracts . 14 Attendee List . 38 Attendee Collaboration Information . 47 SUB-SAHARAN AFRICA CFAR CONFERENCE 2011 1 Dear CFAR Colleagues and Partners! On behalf of the U .S . National Institutes of Health-sponsored Centers for AIDS Research, and Makerere University’s Infectious Diseases Institute, welcome to Kampala! It is our pleasure and honor to have you join us for the 2011 Sub-Saharan Africa CFAR Conference as we gather to feature some of the important research being conducted by African investigators collaborating with the 21 Centers for AIDS Research (CFARs) . Our Conference Steering Committee is planning an exciting program focusing on three priority themes: u Integrating Treatment and Prevention in HIV Care u HIV Comorbidities u HIV and Women Through a combination of plenary and poster presentations, panel discussions, and networking sessions, this meeting will present a unique opportunity for both scientific and information exchange . A special effort will be made to provide a platform for sharing information on existing scientific resources and infrastructure at leading African institutions that support AIDS research and training – a critical prerequisite for the exchange of scientific resources, capacity building, and the fostering of new collaborations among African institutions . The conference has already generated much energy and interest . We envision this momentum leading to the emergence of an African-led network that will build on existing collaborations and begin to explore potential synergies with new partners – including other CFARs, other complementary networks active in Africa, and in particular, South-South partnerships among African institutions – to strengthen the community of science on the continent . -

Chapter 1: Background to the Study: Decentralisation and Urban Governance
Decentralisation and Urban Governance in Uganda By Sabiti Makara Supervisor: Prof. Tom Lodge Thesis submitted to the University of the Witwatersrand, Johannesburg For the award of a Ph.D in the Faculty of Humanities 2009 i Declaration I declare that this is my own work which, to the best of my knowledge, has not been submitted to any university for any academic award. ii Dedication This work is dedicated to the memory of my late father, Eliab Makara who taught me that life and work have the same meaning, and to my late grandmother Egransi Baroza, under whose care and guidance I grew to realise my childhood dream. iii Acknowledgement I am indebted to many people for their contribution to this work. I thank my supervisor Professor Tom Lodge, who despite the challenge of transferring from Wits to Limerick University retained and guided me to the end. It is a privilege accorded to very few students and I am lucky to have associated with him in this regard. To the members of my family, especially my wife Beatrice Kabahinda, children: Janet Kukundakwe, Jessica Namara, Joy Asiimwe and Joseph Ruteikara and to my dear mother, Medias, I owe you a pat on the back for all kinds of support to me. It was never a bed of roses, it was a struggle throughout. I am grateful to Makerere University for a grant that enabled me to pursue this degree. Last but not least, I thank my colleagues who contributed in various capacities to the process of writing this work: William Muhumuza, Paul Omach, Andrew Ellias State, R. -
Croi 2021 Program Committee
General Information CONTENTS WELCOME . 2 General Information General Information OVERVIEW . 2 CONTINUING MEDICAL EDUCATION . 3 CONFERENCE SUPPORT . 4 VIRTUAL PLATFORM . 5 ON-DEMAND CONTENT AND WEBCASTS . 5 CONFERENCE SCHEDULE AT A GLANCE . 6 PRECONFERENCE SESSIONS . 9 LIVE PLENARY, ORAL, AND INTERACTIVE SESSIONS, AND ON-DEMAND SYMPOSIA BY DAY . 11 SCIENCE SPOTLIGHTS™ . 47 SCIENCE SPOTLIGHT™ SESSIONS BY CATEGORY . 109 CROI FOUNDATION . 112 IAS–USA . 112 CROI 2021 PROGRAM COMMITTEE . 113 Scientific Program Committee . 113 Community Liaison Subcommittee . 113 Former Members . 113 EXTERNAL REVIEWERS . .114 SCHOLARSHIP AWARDEES . 114 AFFILIATED OR PROXIMATE ACTIVITIES . 114 EMBARGO POLICIES AND SOCIAL MEDIA . 115 CONFERENCE ETIQUETTE . 115 ABSTRACT PROCESS Scientific Categories . 116 Abstract Content . 117 Presenter Responsibilities . 117 Abstract Review Process . 117 Statistics for Abstracts . 117 Abstracts Related to SARS-CoV-2 and Special Study Populations . 117. INDEX OF SPECIAL STUDY POPULATIONS . 118 INDEX OF PRESENTING AUTHORS . .122 . Version 9 .0 | Last Update on March 8, 2021 Printed in the United States of America . © Copyright 2021 CROI Foundation/IAS–USA . All rights reserved . ISBN #978-1-7320053-4-1 vCROI 2021 1 General Information WELCOME TO vCROI 2021 Welcome to vCROI 2021! The COVID-19 pandemic has changed the world for all of us in so many ways . Over the past year, we have had to put some of our HIV research on hold, learned to do our research in different ways using different tools, to communicate with each other in virtual formats, and to apply the many lessons in HIV research, care, and community advocacy to addressing the COVID-19 pandemic . Scientists and community stakeholders who have long been engaged in the endeavor to end the epidemic of HIV have pivoted to support and inform the unprecedented progress made in battle against SARS-CoV-2 . -

10Th Anniversary Report Leslie Engel, Editor Kerstin Vogdes, Designer
Doris Duke Charitable Foundation Medical Research Program 10th Anniversary Report Leslie Engel, editor Kerstin Vogdes, designer On cover from top to bottom: Friedhelm Hildebrandt, 2006 Distinguished Clinical Scientist, Harmony Reynolds, 2006 Clinical Scientist Development Awardee, and Brian Somoano, 2003-2004 Clinical Research Fellow. Doris Duke Charitable Foundation Medical Research Program 10th Anniversary Report :: Table of Contents :: I. Message from the President . 3 II. Message from the Program Director . 4 III. Message from the Chairman of the Scientific Advisory Council . .5 IV. Acknowledgments . .6 V. Doris Duke Charitable Foundation . 7 About the Foundation . 8 About the Medical Research Program . 10 Staff . 13 Scientific Advisory Council . 14 VI. Anniversary Highlights . 15 Impacting Patient Care and Treatment Through Clinical Research . 16 Screening for Stroke in Sickle Cell Disease: Michael DeBaun, MD, MPH . 16 Molecular Signatures Reveal Rational Treatment Targets in Diffuse Large B-cell Lymphoma: Margaret Shipp, MD . .17 Translating Laboratory Advances to New Therapies for Atherosclerosis: Daniel Rader, MD . 18 Developing the Career Ladder for Physician-Scientists . .19 Supporting the Clinical Research Career Ladder from Medical Students to Senior Faculty: Philip Rosenthal, MD, Grant Dorsey, MD, PhD, MPH, Lisa Bebell, MD . 19 Stimulating Innovation in Clinical Research . .20 Tackling the Lack of Inexpensive Point-of-Care HIV Diagnostics: David Anderson, PhD . 21 Identifying New Viral Pathogens Using Genomics-Based Approaches: Don Ganem, MD . 22 Identifying Smokers with an Increased Risk of Developing Lung Cancer: Avrum Spira, MD, MSc . 23 Supporting Clinical Research in Africa . 24 African Health Research . .24 Tackling Tuberculosis and HIV Co-Infection in Rural South Africa: Gerald Friedland, MD . -

Durban Declaration Dishonor Roll
Hall of Shame (2000) The Durban Declaration. Nature 406: 15-16. THE DURBAN Simon Agwale, PhD Françoise Barré-Sinoussi, PhD DECLARATION Institute of Human Virology Research Director, INSERM ORGANIZING Baltimore, MD Professor, Institut Pasteur COMMITTEE USA Retroviral Biology Unit Updated July 3, 2000 Paris, France Arthur J. Ammann, MD Quarraisha Abdool Karim, PhD President Avertino Barreto, MD, MSc, Southern African Fogarty AIDS Global Strategies for HIV CHDC Training Program Co-ordinator Prevention National Director of Nell and Shapiro cc San Rafael, CA STD/HIV/AIDS Programme Durban USA Deputy National Health South Africa Director Birgitta Åsjö, MD, PhD Ministry of Health Salim S. Abdool Karim, Professor of Virology Maputo MBChB, PhD University of Bergen Mozambique Director, HIV Prevention and Norway Vaccine Research Jorge Barreto, MD Medical Research Council Laura Astarloa, MD, PhD Head, Department of Durban Professor Immunology South Africa University of Buenos Aires National Institute of Health School of Medicine Maputo Alash’le Abimiku, PhD Buenos Aires Mozambique Assistant Professor Argentina Institute of Human Virology John G. Bartlett, MD Baltimore, MD Brigitte Autran, MD, PhD Chief, Division of Infectious Professor Diseases Nadine Abiola Hôpital La Pitié-Salpêtrière Johns Hopkins University Assistant Chief, Clinical Paris, France Baltimore, Maryland Biological Laboratory USA Project RETRO-CI Abidjan Mary Bassett, MD, MPH Ivory Coast Department of Community Medicine Georgette Adjorlolo-Johnson, Roberto Badaró, MD, PhD University -

CURRICULUM VITAE the Johns Hopkins University School of Medicine
CURRICULUM VITAE The Johns Hopkins University School of Medicine _____________________________ Robert C. Bollinger, M.D., M.P.H. March 16, 2012 DEMOGRAPHIC INFORMATION Current Appointments: Primary Appointment Professor, Division of Infectious Diseases, Department of Medicine The Johns Hopkins University School of Medicine Secondary Appointment Professor, Department of International Health The Johns Hopkins Bloomberg School of Public Health Professor, Department of Community – Public Health The Johns Hopkins University School of Nursing Personal Data: Business Address The Johns Hopkins University School of Medicine Center for Clinical Global Health Education 600 N. Wolfe Street, Phipps 540 Baltimore, Maryland 21287 Telephone: (410) 614-0936 Fax: (443) 287-6440 email: [email protected] Education and Training: 1979 B.A., Philosophy/Chemistry Haverford College Haverford, Pennsylvania 1984 M.D., Dartmouth Medical School Hanover, New Hampshire 1984-1987 Internal Medicine/Internship/Residency Department of Medicine, University of Maryland Baltimore VA Hospitals Baltimore, Maryland 1988 Master’s in Public Health Department of International Health Johns Hopkins Bloomberg School of Public Health Baltimore, Maryland 1989-1992 Post Doctoral Fellowship, Infectious Diseases The Johns Hopkins University School of Medicine Baltimore, Maryland In the laboratory of Robert Siliciano, M.D., Ph.D. Research area: The Cytolytic T lymphocyte (CTL) response to HIV-1 Professional Experience: 10/79-1/80 Leprosy Control, Damien Social Welfare Centre Bihar, India 1/80-9/80 -

JULIET NABBUYE SEKANDI ______Global Health Institute, College of Public Health Wright Hall, Room 102B 100 Foster Road, Athens, GA 30602
JULIET NABBUYE SEKANDI ______________________________________________________________________________ Global Health Institute, College of Public Health Wright Hall, Room 102B 100 Foster Road, Athens, GA 30602 EDUCATION University of Georgia Athens, GA- Dec, 2013 Doctor of Public Health, DrPH Concentration: Epidemiology Case Western Reserve University, Cleveland, OH- May, 2006 Masters of Science, MS Concentration: Health Services Research & Epidemiology Mbarara University of Science and Technology, Uganda Mbarara, Uganda- Feb 1996 Degree in Human Medicine & Surgery, MBChB University of Georgia, Athens, GA- 2014-2016 Post-doctoral Fellowship Focus: TB patients’ diagnostic pathways and mHealth Harvard University, T Chan School of Public Health Boston, MA -2016 Certificate in Global Health NIH Fogarty mHealth Institute, Bethesda, MD- 2016 Certificate in mHealth Research Harvard University Boston, MA -2007 Fellowship in Health Services Research Methods EMPLOYMENT HISTORY 08/2016- Present Assistant Professor, Global Health Institute & Dept. of Epidemiology, College of Public Health, University of Georgia 01/ 2014- 07/ 2015 Post-doctoral research and teaching fellow, Dept. of Epidemiology, College of Public Health, University of Georgia 01/2014-07/2015 Senior Lecturer, Makerere University School of Public Health, Kampala, Uganda [on study leave] 02/2011– 12/2013 Assistant Lecturer, Makerere University School of Public Health, Kampala, Uganda Page 1 of 10 01/2008 – 12/2009 Academic Coordinator, Masters of Health Services Research Program, Makerere -
Conference Programme
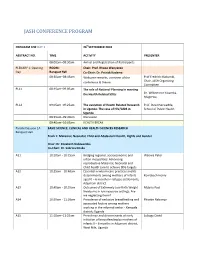
JASH CONFERENCE PROGRAM PROGRAM FOR DAY 1 26thSEPTEMBER 2018 ABSTRACT NO. TIME ACTIVITY PRESENTER 08:00am–08:30am Arrival and Registration of Participants PLENARY 1: Opening ROOM: Chair: Prof. Rhoda Wanyenze Day Banquet Hall Co-Chair: Dr. Patrick Kadama 08:30am–08:45am Welcome remarks, overview of the Prof Fredrick Makumbi, conference & theme Chair, JASH Organizing Committee PL11 08:45am–09:05am The role of National Planning in meeting the Health Related SDGs Dr. Wilberforce Kisamba- Mugerwa, PL12 09:05am–09:25am The evolution of Health Related Research Prof. David Serwadda, in Uganda: The case of HIV/AIDS in School of Public Health Uganda 09:25am–09:40am Discussion 09:40am–10:05am HEALTH BREAK Parallel Session 1A BASIC SCIENCE, CLINICAL AND HEALTH SCIENCES RESEARCH Banquet Hall Track 1: Maternal, Neonatal, Child and Adolescent Health, Rights and Gender Chair: Dr. Elizabeth Nabiwemba Co-Chair: Dr. Sabrina Kitaka A11 10:10am - 10:25am Bridging regional, socioeconomic and Waiswa Peter urban inequalities: Advancing reproductive Maternal, Neonatal and Child health care to achieve SDG targets. A12 10:25am - 10:40am Essential newborn care practices and its determinants among mothers of infants Komakech Henry aged 0 – 6 months in refugee settlements, Adjumani district A13 10:40am - 10:55am Outcomes of Extremely Low Birth Weight Mubiru Paul Newborns in low resource settings: Are we neglecting them? A14 10:55am - 11:10am Prevalence of exclusive breastfeeding and Phoebe Nabunya associated factors among mothers working in the informal sector - Kampala district; Uganda A15 11:10am–11:25am Prevalence and determinants of early Lubogo David initiation of breastfeeding by mothers of infants 0 – 6 months in Adjumani district, West Nile, Uganda PROGRAM FOR DAY 1 26thSEPTEMBER 2018 ABSTRACT NO.