ABC of Prehospital Emergency Medicine / Edited by Tim Nutbeam, Matthew Boylan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Non-Incineration Medical Waste Treatment Technologies
Non-Incineration Medical Waste Treatment Technologies A Resource for Hospital Administrators, Facility Managers, Health Care Professionals, Environmental Advocates, and Community Members August 2001 Health Care Without Harm 1755 S Street, N.W. Unit 6B Washington, DC 20009 Phone: 202.234.0091 www.noharm.org Health Care Without Harm 1755 S Street, N.W. Suite 6B Washington, DC 20009 Phone: 202.234.0091 www.noharm.org Printed with soy-based inks on Rolland Evolution, a 100% processed chlorine-free paper. Non-Incineration Medical Waste Treatment Technologies A Resource for Hospital Administrators, Facility Managers, Health Care Professionals, Environmental Advocates, and Community Members August 2001 Health Care Without Harm www.noharm.org Preface THE FOUR LAWS OF ECOLOGY . Meanwhile, many hospital staff, such as Hollie Shaner, RN of Fletcher-Allen Health Care in Burlington, Ver- 1. Everything is connected to everything else, mont, were appalled by the sheer volumes of waste and 2. Everything must go somewhere, the lack of reduction and recycling efforts. These indi- viduals became champions within their facilities or 3. Nature knows best, systems to change the way that waste was being managed. 4. There is no such thing as a free lunch. Barry Commoner, The Closing Circle, 1971 In the spring of 1996, more than 600 people – most of them community activists – gathered in Baton Rouge, Up to now, there has been no single resource that pro- Louisiana to attend the Third Citizens Conference on vided a good frame of reference, objectively portrayed, of Dioxin and Other Hormone-Disrupting Chemicals. The non-incineration technologies for the treatment of health largest workshop at the conference was by far the one care wastes. -
Official Convention Guide
OFFICIAL CONVENTION GUIDE BALTIMORE CONVENTION CENTER • CONVENTION.NATA.ORG Client: Johnson & Johnson IMC job # JSM-16774 Project: NATA News Ad May 2016 Run: Inside Front Cover, June 2016 forward File Name: JJ_Tapes_May_2016.ai Contact Info: Julie Evans, IMC 732.837.3217 DOWNLOAD THE Fueled by NATA 2016 MOBILE APP! Navigate the 67th NATA Clinical Symposia & AT Expo effortlessly with the NATA 2016 mobile app. WITH THE NATA 2016 APP YOU CAN: • Stay organized with up-to-the-minute Exhibitor, Speaker, and Event information • Sync the app across all of your devices with Multi-Device Sync • Receive important real-time communications • Build a personalized schedule and bookmark exhibitors • Take notes during sessions that can be saved and emailed • Interactively locate sessions and exhibitors on the Baltimore Convention Center maps • Visit your bookmarked exhibitors with the Quick Route • Find attendees and connect with your colleagues • Stay in-the-know and join in on social media Downloading the App is Easy! SEARCH: The App Store or Google Play for “NATA2016” SCAN For All Other Device Types (including BlackBerry, Windows, and all other web browser-enabled devices): While on your smartphone, point your mobile browser to m.core-apps.com/nata2016 to be directed to the proper download version for your device. Platform Compatibility: Android v4x+ and iOS v7x+ Should you have any questions, please contact [email protected] 10-13_J&J-Day-Keynote_P3.indd 13 5/12/16 6:11 PM COME BY TO SEE OUR INNOVATION JOURNEY ANDCOME EXPERIENCE BY TO SEE THE OUR FUTURE INNOVATION OF SPORTS JOURNEY FUEL. AND PLUS,EXPERIENCE RECEIVE THE YOUR FUTURE FREE OF GIVEAWAY. -

Human Physiology an Integrated Approach
Gas Exchange and Transport Gas Exchange in the Lungs and Tissues 18 Lower Alveolar P Decreases Oxygen Uptake O2 Diff usion Problems Cause Hypoxia Gas Solubility Aff ects Diff usion Gas Transport in the Blood Hemoglobin Binds to Oxygen Oxygen Binding Obeys the Law of Mass Action Hemoglobin Transports Most Oxygen to the Tissues P Determines Oxygen-Hb Binding O2 Oxygen Binding Is Expressed As a Percentage Several Factors Aff ect Oxygen-Hb Binding Carbon Dioxide Is Transported in Three Ways Regulation of Ventilation Neurons in the Medulla Control Breathing Carbon Dioxide, Oxygen, and pH Infl uence Ventilation Protective Refl exes Guard the Lungs Higher Brain Centers Aff ect Patterns of Ventilation The successful ascent of Everest without supplementary oxygen is one of the great sagas of the 20th century. — John B. West, Climbing with O’s , NOVA Online (www.pbs.org) Background Basics Exchange epithelia pH and buff ers Law of mass action Cerebrospinal fl uid Simple diff usion Autonomic and somatic motor neurons Structure of the brain stem Red blood cells and Giant liposomes hemoglobin of pulmonary Blood-brain barrier surfactant (40X) From Chapter 18 of Human Physiology: An Integrated Approach, Sixth Edition. Dee Unglaub Silverthorn. Copyright © 2013 by Pearson Education, Inc. All rights reserved. 633 Gas Exchange and Transport he book Into Thin Air by Jon Krakauer chronicles an ill- RUNNING PROBLEM fated trek to the top of Mt. Everest. To reach the summit of Mt. Everest, climbers must pass through the “death zone” T High Altitude located at about 8000 meters (over 26,000 ft ). Of the thousands of people who have attempted the summit, only about 2000 have been In 1981 a group of 20 physiologists, physicians, and successful, and more than 185 have died. -

Everest and Oxygen—Ruminations by a Climber Anesthesiologist by David Larson, M.D
Everest and Oxygen—Ruminations by a Climber Anesthesiologist By David Larson, M.D. Gaining Altitude and Losing Partial Pressure with Dave and Samantha Larson Dr. Dave Larson is an obstetric anesthesiologist who practices at Long Beach Memorial Medical Center, and his daughter Samantha is a freshman at Stanford University. Together they have successfully ascended the Seven Summits, the tallest peaks on each of the seven continents, a feat of mountaineering postulated in the 1980s by Richard Bass, owner of the Snowbird Ski Resort in Utah. Bass accomplished it first in 1985. Samantha Larson, who scaled Everest in May 2007 (the youngest non-Sherpa to do so) and the Carstensz Pyramid in August 2007, is at age 18 the youngest ever to have achieved this feat. Because of varying definitions of continental borders based upon geography, geology, and geopolitics, there are nine potential summits, but the Seven Summits is based upon the American and Western European model. Reinhold Messner, an Italian mountaineer known for ascending without supplemental oxygen, postulated a list of Seven Summits that replaced a mountain on the Australian mainland (Mount Kosciuszko—2,228 m) with a higher peak in Oceania on New Guinea (the Carstensz Pyramid—4,884 m). The other variation in defining summits is whether you define Mount Blanc (4,808 m) as the highest European peak, or use Mount Elbrus (5,642 m) in the Caucasus. Other summits include Mount Kilimanjaro in Kenya, Africa (5,895 m), Vinson Massif in Antarctica (4,892 m), Mount Everest in Asia (8,848 m), Mount McKinley in Alaska, North America (6,194 m), and Mount Aconcagua in Argentina, South America (6,962 m). -

Enhancing Care Across the Continuum
2017 CAREHOLDERS’ REPORT MedStar: enhancing care across the continuum © 2017 MedStar Mobile Healthcare. All Rights Reserved. MISSION STATEMENT To Provide World Class Mobile Healthcare with the Highest-Quality Customer Service and Clinical Excellence in a Fiscally Responsible Manner. 2 Haslet • Saginaw • Blue • Mound 2017 Careholders’ Report Lakeside • CEO’s Message ..............................................1 Lake Worth • Haltom MedStar at a Glance .......................................2 • Sansom Park City • Making the Difference - MedStar People .........3 Naval Air Station • • River Oaks Community Commitment ................................5 • Westworth Village Higher Standards: Service ..............................7 • White Settlement The Medicine - Fort Medical Direction and Oversight .................11 Worth Leadership ...................................................15 Forest Hill • Edgecliff Village • MedStar's service area encompasses 15 cities, 434 square miles and a population of Burleson • nearly 1 million residents. CEO’S MESSAGE MedStar’s had an amazing year in 2016! April 1, 2016 was a significant milestone for MedStar substantial transition this year toward the concept of “EMS 3.0”. Most no- as we celebrated our 30th Anniversary with the theme tably, we were approached by insurers with an idea to completely change ‘30 Years of Caring and Innovation’. The outpouring of how they pay for EMS services—moving away from a fee-for-transport support from our community was humbling, with more model toward a population-based model. As we continue to operation- than 300 community members, current and previ- alize that paradigm shift, we are encouraged by the trust and value that ous employees, and area dignitaries joining us for our our payers have come to place in MedStar and our team members to test anniversary open house event. -

DEATH ZONE FREERIDE About the Project
DEATH ZONE FREERIDE About the project We are 3 of Snow Leopards, who commit the hardest anoxic high altitude ascents and perform freeride from the tops of the highest mountains on Earth (8000+). We do professional one of a kind filming on the utmost altitude. THE TRICKIEST MOUNTAINS ON EARTH NO BOTTLED OXYGEN CHALLENGES TO HUMAN AND NATURE NO EXTERIOR SUPPORT 8000ERS FREERIDE FROM THE TOPS MOVIES ALONE WITH NATURE FREERIDE DESCENTS 5 3 SNOW LEOS Why the project is so unique? PROFESSIONAL FILMING IN THE HARDEST CONDITIONS ❖ Higher than 8000+ m ❖ Under challenging efforts ❖ Without bottled oxygen & exterior support ❖ Severe weather conditions OUTDOOR PROJECT-OF-THE-YEAR “CRYSTAL PEAK 2017” AWARD “Death zone freeride” project got the “Crystal Peak 2017” award in “Outdoor project-of-the-year” nomination. It is comparable with “Oscar” award for Russian outdoor sphere. Team ANTON VITALY CARLALBERTO PUGOVKIN LAZO CIMENTI Snow Leopard. Snow Leopard. Leader The first Italian Snow Leopard. MC in mountaineering. Manaslu of “Mountain territory” club. Specializes in a ski mountaineering. freeride 8163m. High altitude Ski-mountaineer. Participant cameraman. of more than 20 high altitude expeditions. Mountains of the project Manaslu Annapurna Nanga–Parbat Everest K2 8163m 8091m 8125m 8848m 8611m The highest mountains on Earth ❖ 8027 m Shishapangma ❖ 8167 m Dhaulagiri I ❖ 8035 m Gasherbrum II (K4) ❖ 8201 m Cho Oyu ❖ 8051 m Broad Peak (K3) ❖ 8485 m Makalu ❖ 8080 m Gasherbrum I (Hidden Peak, K5) ❖ 8516 m Lhotse ❖ 8091 m Annapurna ❖ 8586 m Kangchenjunga ❖ 8126 m Nanga–Parbat ❖ 8614 m Chogo Ri (K2) ❖ 8156 m Manaslu ❖ 8848 m Chomolungma (Everest) Mountains that we climbed on MANASLU September 2017 The first and unique freeride descent from the altitude 8000+ meters among Russian sportsmen. -

Emergency Medical Services Program Policies – Procedures – Protocols
Emergency Medical Services Program Policies – Procedures – Protocols Protocols Table of Contents GENERAL PROVISIONS ................................................................................................ 3 DESTINATION DECISION SUMMARY-METRO BAKERSFIELD AREA ........................ 5 DETERMINATION OF DEATH ..................................................................................... 12 101 AIRWAY OBSTRUCTION ...................................................................................... 16 102 ALTERED LEVEL OF CONSCIOUSNESS ............................................................ 18 103 ALLERGIC REACTION/ANAPHYLAXIS ................................................................ 20 104 ASYSTOLE/ PULSELESS ELECTRICAL ACTIVITY ............................................. 22 105 BITES STINGS ENVENOMATION ......................................................................... 24 106 BRADYCARDIA ..................................................................................................... 26 107 BRIEF RESOLVED UNEXPLAINED EVENT ......................................................... 29 108 BURNS ................................................................................................................... 32 109 CHEMPACK ........................................................................................................... 35 110 CHEST PAIN OR ACUTE CORONARY SYNDROME ........................................... 37 111 CHEST TRAUMA .................................................................................................. -

Lights and Siren Use by Emergency Medical Services (EMS): Above All Do No Harm
U. S. Department of Transportation National Highway Traffic Safety Administration Office of Emergency Medical Services (EMS) Lights and Siren Use by Emergency Medical Services (EMS): Above All Do No Harm Author: Douglas F. Kupas, MD, EMT-P, FAEMS, FACEP Submitted by Maryn Consulting, Inc. For NHTSA Contract DTNH22-14-F-00579 About the Author Dr. Douglas Kupas is an EMS physician and emergency physician, practicing at a tertiary care medical center that is a Level I adult trauma center and Level II pediatric trauma center. He has been an EMS provider for over 35 years, providing medical care as a paramedic with both volunteer and paid third service EMS agencies. His career academic interests include EMS patient and provider safety, emergency airway management, and cardiac arrest care. He is active with the National Association of EMS Physicians (former chair of Rural EMS, Standards and Practice, and Mobile Integrated Healthcare committees) and with the National Association of State EMS Officials (former chair of the Medical Directors Council). He is a professor of emergency medicine and is the Commonwealth EMS Medical Director for the Pennsylvania Department of Health. Disclosures The author has no financial conflict of interest with any company or organization related to the topics within this report. The author serves as an unpaid member of the Institutional Research Review Committee of the International Academy of Emergency Dispatch, Salt Lake City, UT. The author is employed as an emergency physician and EMS physician by Geisinger Health System, Danville, PA. The author is employed part-time as the Commonwealth EMS Medical Director by the Pennsylvania Department of Health, Bureau of EMS, Harrisburg, PA. -
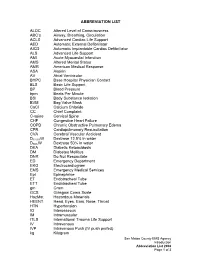
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Ventricular Rhythms Originate Below the Branching Portion of The
Northwest Community Healthcare Paramedic Program VENTRICULAR DYSRHYTHMIAS Pacemakers Connie J. Mattera, M.S., R.N., EMT-P Reading assignments: Bledsoe Vol 3; pp. 96-109 SOPs: VT with pulse; Ventricular fibrillation/PVT; Asystole/PEA Drugs: Amiodarone, magnesium, epinephrine 1mg/10mL Procedure manual: Defibrillation; Mechanical Circulatory Support (MCS) using a Ventricular Assist Device KNOWLEDGE OBJECTIVES: Upon completion of the reading assignments, class and homework questions, reviewing the SOPs, and working with their small group, each participant will independently do the following with at least an 80% degree of accuracy and no critical errors: 1. Identify the intrinsic rates, morphology, conduction pathways, and common ECG features of ventricular beats/rhythms. 2. Identify on a 6-second strip the following: a) Idioventricular rhythm b) Accelerated idioventricular rhythm c) Ventricular tachycardia: monomorphic & polymorphic d) Ventricular escape beats e) Premature Ventricular Contractions (PVCs) f) Ventricular fibrillation g) Asystole h) Paced rhythms i) Intraventricular conduction defects (Bundle branch blocks) 3. Systematically evaluate each complex/rhythm for the following: a) Rate (atrial and ventricular) b) Rhythm: Regular/irregular - R-R Interval, P-P Interval c) Presence/absence/morphology of P waves d) Presence/absence/morphology of QRS complexes d) P-QRS relationships f) QRS duration 4. Correlate the cardiac rhythm with patient assessment findings to determine the emergency treatment for each rhythm according to NWC EMSS SOPs. 5. Discuss the action, prehospital indications, side effects, dose and contraindications of the following during VT a) Amiodarone b) Magnesium 6. Describe the indications, equipment needed, critical steps, and patient monitoring parameters for cardioversion and defibrillation. 7. Identify the management of a patient with an implanted defibrillator and/or pacemaker. -
Burn Model System Summary Report
Burn Model System Summary Report 1994–2017 This report contains information, tables, and figures about the data contained in the Burn Model System National Database, collected from 1993 to 2017. The Burn Model System is funded by the National Institute for Disability, Independent Living, and Rehabilitation Research. This report was produced by the BMS National Data and Statistical Center. 2018 Table of Contents Introduction ............................................................................................................................................................................................ 1 Burn Model System Centers ............................................................................................................................................................. 3 Boston-Harvard Burn Injury Model System (BHBIMS) ...................................................................................................... 3 North Texas Burn Rehabilitation Model System (NTBRMS) ........................................................................................... 3 Pediatric Burn Injury Rehabilitation Model System ........................................................................................................... 4 Northwest Regional Burn Model System (NWRBMS) ....................................................................................................... 4 Burn Model System National Data and Statistical Center (BMS NDSC) .................................................................... 5 Summary -

EMS Spinal Precautions and the Use of the Long Backboard
EMS SPINAL PRECAUTIONS AND THE USE OF THE LONG BACKBOARD – RESOURCE DOCUMENT TO THE POSITION STATEMENT OF THE NATIONAL ASSOCIATION OF EMS PHYSICIANS AND THE AMERICAN COLLEGE OF SURGEONS COMMITTEE ON TRAUMA Chelsea C. White IV, MD, EMT-P, Robert M. Domeier, MD, Michael G. Millin, MD, MPH, and the Standards and Clinical Practice Committee, National Association of EMS Physicians ABSTRACT designed to guide practitioners in understanding of the new position statement. Each item in the position Field spinal immobilization using a backboard and cervical is quoted and followed by a discussion and a review collar has been standard practice for patients with suspected spine injury since the 1960s. The backboard has been a com- of the literature. ponent of field spinal immobilization despite lack of effi- cacy evidence. While the backboard is a useful spinal protec- • “Long backboards are commonly used to attempt tion tool during extrication, use of backboards is not without to provide rigid spinal immobilization among EMS risk, as they have been shown to cause respiratory compro- trauma patients. However, the benefit of long back- mise, pain, and pressure sores. Backboards also alter a pa- boards is largely unproven.” tient’s physical exam, resulting in unnecessary radiographs. Because backboards present known risks, and their value in protecting the spinal cord of an injured patient remains HISTORY OF THE BACKBOARD unsubstantiated, they should only be used judiciously. The following provides a discussion of the elements of the Na- Field spinal immobilization using a cervical collar and tional Association of EMS Physicians (NAEMSP) and Amer- a backboard has been standard practice for patients ican College of Surgeons Committee on Trauma (ACS-COT) with suspected spine injury since the 1960s.