Merseyside Mental Health Equity Audit
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ALTCAR Training Camp
ALTCAR TraINING CAMP A unique wildlife habitat on the Sefton Coast I I I I I I I I I I I Cabin Hill I I I I Formby I I I Dry Training Area I I Alt Grange I I Altcar Training Camp I Altcar Training Camp North Lookout I I River Alt I I R i v I e I r A I l t I I I Pumping I Station I I Lookout I I Hightown I Range Control I I I I Ranges I I I Boat Yard Danger Area I I I I I I South Lookout I I I I I I I I I Crosby I I FOREWORD Altcar Training Camp is owned and managed by the unique habitats. As part of this coast Altcar is a genuine Reserve Forces and Cadets Association for the North sanctuary for nature, the foreshore danger area giving West of England and the Isle of Man as one of the UK’s protection to thousands of passage and over-wintering premier facilities for small arms marksmanship training. birds, the dunes a home to internationally protected species such as the Sand Lizard and Natterjack Toad and In any year over thirty five thousand soldiers learn their the more recent woodland plantations harbouring the rifle skills at Altcar before being deployed to military nationally rare Red Squirrel. activity throughout the world. Since 1977, a Conservation Advisory Group has Altcar Training Camp is also part of the Sefton Coast, supported the management of the Altcar estate, giving a wild stretch of beaches, dunes and woodlands lying advice to ensure that nature conservation sits alongside between Liverpool and Southport. -

2005 No. 170 LOCAL GOVERNMENT, ENGLAND The
STATUTORY INSTRUMENTS 2005 No. 170 LOCAL GOVERNMENT, ENGLAND The County of Lancashire (Electoral Changes) Order 2005 Made - - - - 1st February 2005 Coming into force in accordance with article 1(2) Whereas the Boundary Committee for England(a), acting pursuant to section 15(4) of the Local Government Act 1992(b), has submitted to the Electoral Commission(c) recommendations dated October 2004 on its review of the county of Lancashire: And whereas the Electoral Commission have decided to give effect, with modifications, to those recommendations: And whereas a period of not less than six weeks has expired since the receipt of those recommendations: Now, therefore, the Electoral Commission, in exercise of the powers conferred on them by sections 17(d) and 26(e) of the Local Government Act 1992, and of all other powers enabling them in that behalf, hereby make the following Order: Citation and commencement 1.—(1) This Order may be cited as the County of Lancashire (Electoral Changes) Order 2005. (2) This Order shall come into force – (a) for the purpose of proceedings preliminary or relating to any election to be held on the ordinary day of election of councillors in 2005, on the day after that on which it is made; (b) for all other purposes, on the ordinary day of election of councillors in 2005. Interpretation 2. In this Order – (a) The Boundary Committee for England is a committee of the Electoral Commission, established by the Electoral Commission in accordance with section 14 of the Political Parties, Elections and Referendums Act 2000 (c.41). The Local Government Commission for England (Transfer of Functions) Order 2001 (S.I. -

Data Myout Ward Codes Contents Section One
CONTENTS DATA MYOUT SECTION ONE WARD CODES SECTION lWO vS4 ON TM? ICL 2900 Fonrat lqi3q S&m I Title: IAuthor: Irate: Isheet: 1 I ‘lLmm VS4 I OFWUSEC I SKP 1988 I oNMuNEI’Ic TAm I I I CcmwrER TAPE FILE sPEcrFIcATTm ***** ***************************** This pap de9mibee the intent ad fozmatof the megnetictape verelon of table VS4. I All erquiriescOnzermng the contentof the tebleeor arrerqeuents dietrilution”shcmldbe,a~ to: VlTf3L ST/W5TICS cu~I=Q C+L ICES Officeof Fqulation Cenewes an5 Sumeye Tltd.field Hante m15 5RR Tel: TiHield (0329)42511X305J3 ~lf ic emquuaee omcernwg -W ~ my be altermtiwly addresed to: cDstete Grulpu MR5 S ~EwJANE Tel: Titd_field(0329)42511 x342I Accpyof thewholetapewilllx providedbmstcmws. ‘13u6eonly ted in W will receivethe whole tape, ani ehmld mke their mm ~ for extractingthe :zequheddata. The magnetictepe will k in a formatsuitablefor ~ixJ on ICL (1900or 2900 s-e-rise)or H mahfram madbee. Title: IAuthor: Imte: Imeet: 2 { TAmE VS4 I oKs/aslK SEP 1988 I oNMAaa3rIc TAPE / / / ! KGICAL m SIFUCNJRE I The magnetictape v-ion of the tape will be set cat ae if the tables hadhenprapared using the OFCS tahlaticm utilityTAUerdtheta~ had / been writtenueiru the W utiliiwALCZNSAVEwhi~ savesteblee h a format I suitablefor data-intercimge. - This mans that the ffle is @ysically a file of fhed kqth 80 &aracter remzd.emth a logicalhierarchyof: Fm.E !mBL-5 ARE?+ Textuallabelswill be proviW &m to the ame lwel (naxrative daacriptim of the file,table identi~, area mme.s)hz tstubardmlmn labelseni explanatcq w will rxJtbe imll.kid. If ~ hevethe TAUeoftwareamiwiah tiuseit tiperfozm further analyeesof thedata, than they may baabletousethe~ utilitytoreadths dataintotha TAUsys&n. -

West Midlands European Regional Development Fund Operational Programme
Regional Competitiveness and Employment Objective 2007 – 2013 West Midlands European Regional Development Fund Operational Programme Version 3 July 2012 CONTENTS 1 EXECUTIVE SUMMARY 1 – 5 2a SOCIO-ECONOMIC ANALYSIS - ORIGINAL 2.1 Summary of Eligible Area - Strengths and Challenges 6 – 14 2.2 Employment 15 – 19 2.3 Competition 20 – 27 2.4 Enterprise 28 – 32 2.5 Innovation 33 – 37 2.6 Investment 38 – 42 2.7 Skills 43 – 47 2.8 Environment and Attractiveness 48 – 50 2.9 Rural 51 – 54 2.10 Urban 55 – 58 2.11 Lessons Learnt 59 – 64 2.12 SWOT Analysis 65 – 70 2b SOCIO-ECONOMIC ANALYSIS – UPDATED 2010 2.1 Summary of Eligible Area - Strengths and Challenges 71 – 83 2.2 Employment 83 – 87 2.3 Competition 88 – 95 2.4 Enterprise 96 – 100 2.5 Innovation 101 – 105 2.6 Investment 106 – 111 2.7 Skills 112 – 119 2.8 Environment and Attractiveness 120 – 122 2.9 Rural 123 – 126 2.10 Urban 127 – 130 2.11 Lessons Learnt 131 – 136 2.12 SWOT Analysis 137 - 142 3 STRATEGY 3.1 Challenges 143 - 145 3.2 Policy Context 145 - 149 3.3 Priorities for Action 150 - 164 3.4 Process for Chosen Strategy 165 3.5 Alignment with the Main Strategies of the West 165 - 166 Midlands 3.6 Development of the West Midlands Economic 166 Strategy 3.7 Strategic Environmental Assessment 166 - 167 3.8 Lisbon Earmarking 167 3.9 Lisbon Agenda and the Lisbon National Reform 167 Programme 3.10 Partnership Involvement 167 3.11 Additionality 167 - 168 4 PRIORITY AXES Priority 1 – Promoting Innovation and Research and Development 4.1 Rationale and Objective 169 - 170 4.2 Description of Activities -

Hunting and Social Change in Late Saxon England
Eastern Illinois University The Keep Masters Theses Student Theses & Publications 2016 Butchered Bones, Carved Stones: Hunting and Social Change in Late Saxon England Shawn Hale Eastern Illinois University This research is a product of the graduate program in History at Eastern Illinois University. Find out more about the program. Recommended Citation Hale, Shawn, "Butchered Bones, Carved Stones: Hunting and Social Change in Late Saxon England" (2016). Masters Theses. 2418. https://thekeep.eiu.edu/theses/2418 This is brought to you for free and open access by the Student Theses & Publications at The Keep. It has been accepted for inclusion in Masters Theses by an authorized administrator of The Keep. For more information, please contact [email protected]. The Graduate School� EASTERNILLINOIS UNIVERSITY " Thesis Maintenance and Reproduction Certificate FOR: Graduate Candidates Completing Theses in Partial Fulfillment of the Degree Graduate Faculty Advisors Directing the Theses RE: Preservation, Reproduction, and Distribution of Thesis Research Preserving, reproducing, and distributing thesis research is an important part of Booth Library's responsibility to provide access to scholarship. In order to further this goal, Booth Library makes all graduate theses completed as part of a degree program at Eastern Illinois University available for personal study, research, and other not-for-profit educational purposes. Under 17 U.S.C. § 108, the library may reproduce and distribute a copy without infringing on copyright; however, professional courtesy dictates that permission be requested from the author before doing so. Your signatures affirm the following: • The graduate candidate is the author of this thesis. • The graduate candidate retains the copyright and intellectual property rights associated with the original research, creative activity, and intellectual or artistic content of the thesis. -

68 Freshfield Road Formby, Liverpool, Merseyside, L37 7BQ
68 Freshfield Road £775,000 Formby, Liverpool, Merseyside, L37 7BQ Asking Price 18 CHAPEL LANE Opening Hours FORMBY, LIVERPOOL, L37 4DU Mon, Tue, Thur, Fri 09:00 to 17:00 [email protected] Wed 09:30 to 17:00 www.halifax.co.uk/estateagency Sat 09:00 to 16:00 Sun closed 01704 878545 Details A unique opportunity to acquire this 7 bedroom Victorian detached residence with grounds in a highly sought after location. With tall ceilings, spacious rooms and period character throughout the property comprises enclosed porch, entrance hall, lounge open to dining room, sitting room, downstairs bathroom suite, dining kitchen, family shower room and 7 bedrooms over 2 floors. The property benefits from central heating system, partial double glazing and double garage. Accommodation Enclosed Porch Spacious Entrance Hall Sitting Room 4.23(13' 11'') x 4.89(16' 1'') (max to bay) Front Lounge (open to Dining Room) 5.15(16' 11'') x 4.55(14' 11'') (max to recess) Dining Room 4.85(15' 11'') x 5.51(18' 1'') (max to bay) Ground Floor Bathroom Suite 1.70(5' 7'') x 2.29(7' 6'') Dining Kitchen 4.46(14' 8'') x 4.62(15' 2'') (max to bay) Turned Staircase to First Floor Landing Family Shower Room 2.85(9' 4'') x 1.65(5' 5'') Front Bedroom 1 5.11(16' 9'') x 4.55(14' 11'') Rear Bedroom 2 3.70(12' 2'') to recess x 5.52(18' 1'') to bay Front Bedroom 3 4.89(16' 1'') to bay x 3.69(12' 1'') to robes Rear Bedroom 4 4.20(13' 9'') x 4.28(14' 1'') Turned Staircase to Second Floor Landing Front Bedroom 5 4.76(15' 7'') x 2.26(7' 5'') Rear Bedroom 6 3.93(12' 11'') x 3.04(10' 0'') Side Bedroom 7 2.49(8' 2'') x 2.76(9' 1'') & 4.46(14' 8'') x 2.83(9' 3'') Gardens surrounding property Detached Double Garage 5.38(17' 8'') x 7.89(25' 11'') HIP AVAILABLE Directions Tenure From this office depart on Chapel Lane. -

St Faith`S Church, Great Crosby Confirmation Registers 1901 – 2000
1 St Faith`s Church, Great Crosby Confirmation Registers 1901 – 2000 There are two volumes covering the church`s first century, volume 1 covering the period 1901 to 1958 and volume 2 the period 1959 to 2000; volume 2 is not yet full. The registers have entries for a particular confirmation event detailing the names, ages and addresses of those being confirmed (the addresses are not always included for the most recent confirmation candidates). The location of the confirmation service, its date and the Bishop confirming the candidates are given. A number of early male candidates for confirmation came from Merchant Taylors` School which then took boarding pupils. The first volume, for some individuals, mentions when they moved from the district, joined the forces or joined the merchant navy. During the first decade some adults were confirmed privately at the Bishop`s Palace in Liverpool. Services for adults were often held during the latter part of the year and the main confirmation service during March or April. Candidates before WWII would often travel some distance for a confirmation service, in some cases as far as Wigan, Warrington and Rock Ferry. Although most confirmations were conducted by the Bishop of Liverpool or the Bishop of Warrington there have been times when other bishops have conducted the confirmations. Most notable was Lord Runcie of Cuddesdon but in March 1945 the Bishop of the Argentine presided. An interesting feature of the period up to about 1930 is the number of parents who were confirmed shortly before their children were confirmed. In these transcripts some early confirmations are show as having taken place at the Cathedral. -
Walking and Cycling Guide to Sefton’S Natural Coast
Walking and Cycling Guide to Sefton’s Natural Coast www.seftonsnaturalcoast.com Altcar Dunes introduction This FREE guide has been published to encourage you to get out and about in Southport and Sefton. It has been compiled to help you to discover Sefton’s fascinating history and wonderful flora and fauna. Walking or cycling through Sefton will also help to improve your health and fitness. With its wide range of accommodation to suit all budgets, Southport makes a very convenient base. So make the most of your visit; stay over one or two nights and take in some of the easy, family-friendly walks, detailed in this guide. Why not ‘warm-up’ by walking along Lord Street with its shops and cafés and then head for the promenade and gardens alongside the Marine Lake. Or take in the sea air with a stroll along the boardwalk of Southport Pier before walking along the sea wall of Marine Drive to the Queen’s Jubilee Nature Trail or the new Eco Centre nearby. All the trails and walks are clearly signposted and suitable for all ages and abilities. However, as with all outdoor activities, please take sensible precautions against our unpredictable weather and pack waterproof clothing and wear suitable shoes. Don’t forget your sun cream during the Summer months. If cycling, make sure that your bike is properly maintained and wear a protective helmet at all times. It's also a good idea to include some food and drink in a small day-pack, as although re-fuelling stops are suggested on the listed routes, there is no guarantee that they will be open when you need them. -
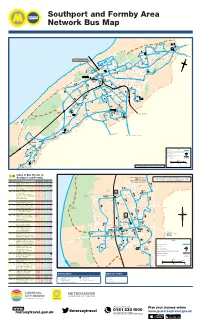
To Bus Routes in Southport and Formby
Southport and Formby Area Network Bus Map E M I V R A D R I N M E E A E N U I R N R E Harrogate Way A S V 40 M H A S Y O 40 A R D I W TRU S X2 to Preston D G R K H L I E I P E V A T M N R E O D 40 A R O C N 44 I R N L O O LSWI OAD O L A C R G K T Y E A V N A A E R . S D A E E RO ’ T K X2 G S N N R TA 40 E S 40 h RS t GA 44 A a W p O D B t A o P A R Fo I Y A 47.49 D V 40 l E ta C as 44 E Co n 44 fto 40 44 F Y L D E F e D S 15 40 R O A A I G R L Crossens W H E AT R O A D 40 A N ER V P X2 D M ROAD A D O THA E L NE H 15 Y R A O L N K A D E 347 W D O A S T R R 2 E ROA R O 347 K E D O . L A 47 E F Marshside R R D T LD 2 Y FIE 2 to Preston S H A ELL 49 A 15 SH o D D 347 to Chorley u W E N t V E I R 40 W R h R I N O M D A E p A L O o R F A r N F R t 15 R N E F N Golf O P I E S T O R A D X2 U A U H L ie 44 E N R M D N I F E R r Course E S LARK Golf V 347 T E D I C Southport Town Centre Marine D A E D N S H P U R A N E O E D A B Lake A Course I R R O A E 47 calls - N S V T R C 15.15 .40.44.46.46 .47.49.315(some)X2 R K V A E A E T N S HM E K R Ocean D I 2 E O M A L O O R A R L R R R IL O P Plaza P L H H B D A D O OO D E C AD A A R D 40 O A W 40 A S U 40 O N R T K 40 EE O 40 H R Y Y D L R E C LE F T L E S E E H U V W W L 15 O N I 49 KN Y R A R R G O D E R M O A L L S A R A A D M O E L M T E M I D B A Southport C R IDG E A E B Hesketh R S M I A N T C R S Hospital O E E E A Princes E 2 D E D R .1 P A A 5. -

University Hospital Aintree and Southport & Ormskirk NHS Trust
The successful merger of DAWN AC between University Hospital Aintree and Southport & Ormskirk NHS Trust Hannah Williams MSc BSc FIBMS Senior Biomedical Scientist Why are we doing this? • Community Anticoagulation Services for Southport and Formby CCG and South Sefton CCG were put out to tender ………..and Aintree was awarded the contract Brief history…… • Both hospital (UHA) and community clinics use Thrombotrak analysers and DAWN • Both are BMS led • UHA has 1 Specialist Nurse Practicioner (NMP) and a Consultant Haematologist lead UHA Comprised of patients from Liverpool ~ 2500 patients CCG, South Sefton CCG, Southport & 11 clinic sessions pw (500 pts) Formby CCG, Knowsley CCG 2 new patient sessions pw (20pts) DAWN v7 Southport & Ormskirk Comprised of patients from South Sefton ~1900 patients CCG, Southport & Formby CCG, 2 sessions pw at ODGH West Lancashire CCG 3sessions pw at SDGH ~ 4500 community patients 19 sessions pw (1000 patients) Domicillary visits (100 – 150 pw) AF only initiated in community DAWN v7 Tender specification included • Time to first appointment – less than 14 days for new patients, five working days for patients discharged from hospital • INR should be made available to GP within 1 working day and done as part of computerised support software. • Quality indicators – TTR, etc Aim • To meet the tender spec and create one DAWN system for UHA and the community service. ~ 7000 patients 11 sessions pw at UHA 23 sessions pw at 9 locations across the community Domicillary visits (100 – 150 pw) * Only South Sefton CCG and Southport & Formby CCG patients will be transferred from Southport & Ormskirk Already in place Require • GP read only access to • DAWN interface to hospital DAWN (community only) PAS system • DAWN mailer (AHT only) • Remote access to DAWN from clinic premises • A test system needs to be available on both the Aintree and the Southport sites. -

Translocating Isle of Man Cabbage Coincya Monensis Ssp
Conservation Evidence (2012) 9, 67-71 www.conservationevidence.com Translocating Isle of Man cabbage Coincya monensis ssp. monensis in the sand-dunes of the Sefton coast, Merseyside, UK Philip H. Smith1* & Patricia A. Lockwood2 19 Hayward Court, Watchyard Lane, Formby, Liverpool L37 3QP 213 Stanley Road, Formby, Liverpool L37 7AN *Corresponding author e-mail: [email protected] SUMMARY This paper describes the results of a translocation rescue of the British endemic Isle of Man cabbage Coincya monensis ssp. monensis from a sand-dune ridge at Crosby, Merseyside, which was about to be excavated as a source of sand for a coastal protection scheme at nearby Hightown. Using methods developed during a 1992 translocation, over eight hundred 1st year plants, together with seed-pods, were moved by volunteers to two protected receptor sites at Crosby and Birkdale in August 2011. Monitoring the following summer located small surviving populations at the receptor sites but mortality of transplants appeared to be over 90%, seed germination and establishment contributing most individuals. Low success at Crosby seemed partly attributable to winter sand-blow and heavy public pressure, while vegetation overgrowth may have been an adverse factor at Birkdale. An unexpected finding was that the original Crosby colony survived the removal of most of its habitat, about 1300 plants being counted in 2012 on the levelled dune area. More than half were small seedlings, presumably derived from buried seed. Also, 234 Isle of Man cabbage plants were discovered on the new coastal defence bund at Hightown, having arisen from propagules transported from Crosby. Other known Sefton duneland colonies at Southport Marine Lake and Blundellsands were also monitored, the former having apparently declined to extinction. -

View PDF of Article
© The Authors 2021 International Practice Development Journal 11 (1) [5] fons.org/library/journal-ipdj-home International Practice PcP-ICoP Development Journal Working together to develop practice Online journal of FoNS in association with the IPDC and PcP-ICoP (ISSN 2046-9292) ORIGINAL PRACTICE DEVELOPMENT AND RESEARCH Implementing the PIE (Person, Interaction and Environment) programme to improve person-centred care for people with dementia admitted to hospital wards: a qualitative evaluation Ann Skingley*, Mary Godfrey, Rosemary Henderson, Kim Manley, Rosie Shannon and John Young *Corresponding author: Canterbury Christ Church University , Canterbury, England Email: [email protected] Submitted for publication: 8th January 2021 Accepted for publication: 4th May 2021 Published: 19th May 2021 https://doi.org/10.19043/ipdj.111.005 Abstract Background: In the UK, improving person-centred care for people with dementia in hospitals is a policy priority. The PIE (Person, Interaction, Environment) programme comprises cycles of observation of care by staff, identification of areas for improvement and plans for practice change and evaluation. Aim: To describe and evaluate PIE implementation in three UK NHS regions. Methods: A qualitative design was adopted at 10 case study sites (wards), selected on the basis of readiness for change criteria. Following a training workshop, PIE cycles were introduced into each ward. Data collection comprised observation, interviews, documentary analysis and an events log. Normalisation process theory provided a guiding framework for analysis. Results: PIE was fully adopted in two study wards over 18 months, which resulted in sustained practice change and increased awareness of person-centredness. Partial implementation of PIE took place in a further two wards but progress stalled before significant action.