Life Expectancy Mortality
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ALTCAR Training Camp
ALTCAR TraINING CAMP A unique wildlife habitat on the Sefton Coast I I I I I I I I I I I Cabin Hill I I I I Formby I I I Dry Training Area I I Alt Grange I I Altcar Training Camp I Altcar Training Camp North Lookout I I River Alt I I R i v I e I r A I l t I I I Pumping I Station I I Lookout I I Hightown I Range Control I I I I Ranges I I I Boat Yard Danger Area I I I I I I South Lookout I I I I I I I I I Crosby I I FOREWORD Altcar Training Camp is owned and managed by the unique habitats. As part of this coast Altcar is a genuine Reserve Forces and Cadets Association for the North sanctuary for nature, the foreshore danger area giving West of England and the Isle of Man as one of the UK’s protection to thousands of passage and over-wintering premier facilities for small arms marksmanship training. birds, the dunes a home to internationally protected species such as the Sand Lizard and Natterjack Toad and In any year over thirty five thousand soldiers learn their the more recent woodland plantations harbouring the rifle skills at Altcar before being deployed to military nationally rare Red Squirrel. activity throughout the world. Since 1977, a Conservation Advisory Group has Altcar Training Camp is also part of the Sefton Coast, supported the management of the Altcar estate, giving a wild stretch of beaches, dunes and woodlands lying advice to ensure that nature conservation sits alongside between Liverpool and Southport. -

68 Freshfield Road Formby, Liverpool, Merseyside, L37 7BQ
68 Freshfield Road £775,000 Formby, Liverpool, Merseyside, L37 7BQ Asking Price 18 CHAPEL LANE Opening Hours FORMBY, LIVERPOOL, L37 4DU Mon, Tue, Thur, Fri 09:00 to 17:00 [email protected] Wed 09:30 to 17:00 www.halifax.co.uk/estateagency Sat 09:00 to 16:00 Sun closed 01704 878545 Details A unique opportunity to acquire this 7 bedroom Victorian detached residence with grounds in a highly sought after location. With tall ceilings, spacious rooms and period character throughout the property comprises enclosed porch, entrance hall, lounge open to dining room, sitting room, downstairs bathroom suite, dining kitchen, family shower room and 7 bedrooms over 2 floors. The property benefits from central heating system, partial double glazing and double garage. Accommodation Enclosed Porch Spacious Entrance Hall Sitting Room 4.23(13' 11'') x 4.89(16' 1'') (max to bay) Front Lounge (open to Dining Room) 5.15(16' 11'') x 4.55(14' 11'') (max to recess) Dining Room 4.85(15' 11'') x 5.51(18' 1'') (max to bay) Ground Floor Bathroom Suite 1.70(5' 7'') x 2.29(7' 6'') Dining Kitchen 4.46(14' 8'') x 4.62(15' 2'') (max to bay) Turned Staircase to First Floor Landing Family Shower Room 2.85(9' 4'') x 1.65(5' 5'') Front Bedroom 1 5.11(16' 9'') x 4.55(14' 11'') Rear Bedroom 2 3.70(12' 2'') to recess x 5.52(18' 1'') to bay Front Bedroom 3 4.89(16' 1'') to bay x 3.69(12' 1'') to robes Rear Bedroom 4 4.20(13' 9'') x 4.28(14' 1'') Turned Staircase to Second Floor Landing Front Bedroom 5 4.76(15' 7'') x 2.26(7' 5'') Rear Bedroom 6 3.93(12' 11'') x 3.04(10' 0'') Side Bedroom 7 2.49(8' 2'') x 2.76(9' 1'') & 4.46(14' 8'') x 2.83(9' 3'') Gardens surrounding property Detached Double Garage 5.38(17' 8'') x 7.89(25' 11'') HIP AVAILABLE Directions Tenure From this office depart on Chapel Lane. -

St Faith`S Church, Great Crosby Confirmation Registers 1901 – 2000
1 St Faith`s Church, Great Crosby Confirmation Registers 1901 – 2000 There are two volumes covering the church`s first century, volume 1 covering the period 1901 to 1958 and volume 2 the period 1959 to 2000; volume 2 is not yet full. The registers have entries for a particular confirmation event detailing the names, ages and addresses of those being confirmed (the addresses are not always included for the most recent confirmation candidates). The location of the confirmation service, its date and the Bishop confirming the candidates are given. A number of early male candidates for confirmation came from Merchant Taylors` School which then took boarding pupils. The first volume, for some individuals, mentions when they moved from the district, joined the forces or joined the merchant navy. During the first decade some adults were confirmed privately at the Bishop`s Palace in Liverpool. Services for adults were often held during the latter part of the year and the main confirmation service during March or April. Candidates before WWII would often travel some distance for a confirmation service, in some cases as far as Wigan, Warrington and Rock Ferry. Although most confirmations were conducted by the Bishop of Liverpool or the Bishop of Warrington there have been times when other bishops have conducted the confirmations. Most notable was Lord Runcie of Cuddesdon but in March 1945 the Bishop of the Argentine presided. An interesting feature of the period up to about 1930 is the number of parents who were confirmed shortly before their children were confirmed. In these transcripts some early confirmations are show as having taken place at the Cathedral. -
Walking and Cycling Guide to Sefton’S Natural Coast
Walking and Cycling Guide to Sefton’s Natural Coast www.seftonsnaturalcoast.com Altcar Dunes introduction This FREE guide has been published to encourage you to get out and about in Southport and Sefton. It has been compiled to help you to discover Sefton’s fascinating history and wonderful flora and fauna. Walking or cycling through Sefton will also help to improve your health and fitness. With its wide range of accommodation to suit all budgets, Southport makes a very convenient base. So make the most of your visit; stay over one or two nights and take in some of the easy, family-friendly walks, detailed in this guide. Why not ‘warm-up’ by walking along Lord Street with its shops and cafés and then head for the promenade and gardens alongside the Marine Lake. Or take in the sea air with a stroll along the boardwalk of Southport Pier before walking along the sea wall of Marine Drive to the Queen’s Jubilee Nature Trail or the new Eco Centre nearby. All the trails and walks are clearly signposted and suitable for all ages and abilities. However, as with all outdoor activities, please take sensible precautions against our unpredictable weather and pack waterproof clothing and wear suitable shoes. Don’t forget your sun cream during the Summer months. If cycling, make sure that your bike is properly maintained and wear a protective helmet at all times. It's also a good idea to include some food and drink in a small day-pack, as although re-fuelling stops are suggested on the listed routes, there is no guarantee that they will be open when you need them. -
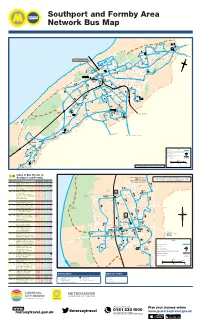
To Bus Routes in Southport and Formby
Southport and Formby Area Network Bus Map E M I V R A D R I N M E E A E N U I R N R E Harrogate Way A S V 40 M H A S Y O 40 A R D I W TRU S X2 to Preston D G R K H L I E I P E V A T M N R E O D 40 A R O C N 44 I R N L O O LSWI OAD O L A C R G K T Y E A V N A A E R . S D A E E RO ’ T K X2 G S N N R TA 40 E S 40 h RS t GA 44 A a W p O D B t A o P A R Fo I Y A 47.49 D V 40 l E ta C as 44 E Co n 44 fto 40 44 F Y L D E F e D S 15 40 R O A A I G R L Crossens W H E AT R O A D 40 A N ER V P X2 D M ROAD A D O THA E L NE H 15 Y R A O L N K A D E 347 W D O A S T R R 2 E ROA R O 347 K E D O . L A 47 E F Marshside R R D T LD 2 Y FIE 2 to Preston S H A ELL 49 A 15 SH o D D 347 to Chorley u W E N t V E I R 40 W R h R I N O M D A E p A L O o R F A r N F R t 15 R N E F N Golf O P I E S T O R A D X2 U A U H L ie 44 E N R M D N I F E R r Course E S LARK Golf V 347 T E D I C Southport Town Centre Marine D A E D N S H P U R A N E O E D A B Lake A Course I R R O A E 47 calls - N S V T R C 15.15 .40.44.46.46 .47.49.315(some)X2 R K V A E A E T N S HM E K R Ocean D I 2 E O M A L O O R A R L R R R IL O P Plaza P L H H B D A D O OO D E C AD A A R D 40 O A W 40 A S U 40 O N R T K 40 EE O 40 H R Y Y D L R E C LE F T L E S E E H U V W W L 15 O N I 49 KN Y R A R R G O D E R M O A L L S A R A A D M O E L M T E M I D B A Southport C R IDG E A E B Hesketh R S M I A N T C R S Hospital O E E E A Princes E 2 D E D R .1 P A A 5. -

University Hospital Aintree and Southport & Ormskirk NHS Trust
The successful merger of DAWN AC between University Hospital Aintree and Southport & Ormskirk NHS Trust Hannah Williams MSc BSc FIBMS Senior Biomedical Scientist Why are we doing this? • Community Anticoagulation Services for Southport and Formby CCG and South Sefton CCG were put out to tender ………..and Aintree was awarded the contract Brief history…… • Both hospital (UHA) and community clinics use Thrombotrak analysers and DAWN • Both are BMS led • UHA has 1 Specialist Nurse Practicioner (NMP) and a Consultant Haematologist lead UHA Comprised of patients from Liverpool ~ 2500 patients CCG, South Sefton CCG, Southport & 11 clinic sessions pw (500 pts) Formby CCG, Knowsley CCG 2 new patient sessions pw (20pts) DAWN v7 Southport & Ormskirk Comprised of patients from South Sefton ~1900 patients CCG, Southport & Formby CCG, 2 sessions pw at ODGH West Lancashire CCG 3sessions pw at SDGH ~ 4500 community patients 19 sessions pw (1000 patients) Domicillary visits (100 – 150 pw) AF only initiated in community DAWN v7 Tender specification included • Time to first appointment – less than 14 days for new patients, five working days for patients discharged from hospital • INR should be made available to GP within 1 working day and done as part of computerised support software. • Quality indicators – TTR, etc Aim • To meet the tender spec and create one DAWN system for UHA and the community service. ~ 7000 patients 11 sessions pw at UHA 23 sessions pw at 9 locations across the community Domicillary visits (100 – 150 pw) * Only South Sefton CCG and Southport & Formby CCG patients will be transferred from Southport & Ormskirk Already in place Require • GP read only access to • DAWN interface to hospital DAWN (community only) PAS system • DAWN mailer (AHT only) • Remote access to DAWN from clinic premises • A test system needs to be available on both the Aintree and the Southport sites. -

Translocating Isle of Man Cabbage Coincya Monensis Ssp
Conservation Evidence (2012) 9, 67-71 www.conservationevidence.com Translocating Isle of Man cabbage Coincya monensis ssp. monensis in the sand-dunes of the Sefton coast, Merseyside, UK Philip H. Smith1* & Patricia A. Lockwood2 19 Hayward Court, Watchyard Lane, Formby, Liverpool L37 3QP 213 Stanley Road, Formby, Liverpool L37 7AN *Corresponding author e-mail: [email protected] SUMMARY This paper describes the results of a translocation rescue of the British endemic Isle of Man cabbage Coincya monensis ssp. monensis from a sand-dune ridge at Crosby, Merseyside, which was about to be excavated as a source of sand for a coastal protection scheme at nearby Hightown. Using methods developed during a 1992 translocation, over eight hundred 1st year plants, together with seed-pods, were moved by volunteers to two protected receptor sites at Crosby and Birkdale in August 2011. Monitoring the following summer located small surviving populations at the receptor sites but mortality of transplants appeared to be over 90%, seed germination and establishment contributing most individuals. Low success at Crosby seemed partly attributable to winter sand-blow and heavy public pressure, while vegetation overgrowth may have been an adverse factor at Birkdale. An unexpected finding was that the original Crosby colony survived the removal of most of its habitat, about 1300 plants being counted in 2012 on the levelled dune area. More than half were small seedlings, presumably derived from buried seed. Also, 234 Isle of Man cabbage plants were discovered on the new coastal defence bund at Hightown, having arisen from propagules transported from Crosby. Other known Sefton duneland colonies at Southport Marine Lake and Blundellsands were also monitored, the former having apparently declined to extinction. -

Cycle Sefton!
G E ' S L A N E t anspor Tr ac Tr cling Cy ing lk Wa ublic ublic P Southport CH A RN In association with LE A Y'S LA NE MARINE DRIVE Cycling is great because it’s… Fresh Air RALPH'S WIFE'S LANE NE LA 'S Fitness FE I W H'S Banks LP RA S M6 KI PT Fun ON H AV A EN R U R E O G A58 A T D For the whole family E C E A U W R A OAD Sefton CouncilN E Y RO N R N O E I Sefton Council S T O TA T S R S V S C G K U A IN E E N B5204 V K N F I F O T A R O R B R Low cost travel D RU E E Y T D N A N I W G A D R L LE R A N E I O E N U T M T CN V V D S Crossens E A C N E E A I R IV S O E E C A S 5 L R Y S N 65 ANCA R D O V O W STE N R Y A M T T Door to door L A S ER E E R G LA I N T R L D M K IN E E M L R N A S A IV O F R L R E M Y S A A A ' E EW H I S S S D U ID A B P C Pollution free E U A T E Y S R R C CN H O A N E E S A A CR T C D W C FT R RO E AUSEWAY N SC C E E E N TH O T D V G T A H I O I N A A R D O E AD S R E D R A O R S S YL D O POOL STREET R N K T F K I A K R IC D B P R This map shows cycle lanes and suggested routes W A Y N LS O R E R G G A W NG R O L P E TA O A R E E N BROOK STREET S D A D O N R AR A D A P E N G O F A around Sefton avoiding busy roads and junctions. -

Cabinet Member Decision Briefing PSPO Alcohol Final FD-LD PDF 468 KB
Report to Cabinet Communities Date of Issue: 20 April 2018 Member for: and Housing Date of Decision: 27 April 2018 Subject: Public Spaces Protection Order (PSPO) - restriction of the drinking of alcohol Report of: Head of Wards Affected: Southport, Communities Crosby/Waterloo, Bootle Town Centre, Formby Is this a Key No Included in No Decision: Forward Plan: Exempt / No Confidential Report: Summary To Inform Cabinet Member – Communities and Housing of the final proposals for the establishment of a Public Spaces Protection Order to restrict drinking alcohol in public in the following areas: Southport Town Centre, Bootle Town Centre, Formby, Crosby/Waterloo Recommendations: To ask Cabinet Member to agree the following: (1) That the content, proposals and restrictions within the PSPO’s are acceptable. (2) That amendments made as a result of the Consultation process are agreeable. (3) For the final version of the PSPO to be presented to the Legal Department to prepare and execute the Order. Reason for the Recommendations: To formally approve the Public Spaces Protection Order (PSPO) Alternative Options Considered and Rejected: (including any Risk Implications) N/A What will it cost and how will it be financed? (A) Revenue Costs N/A (B) Capital Costs N/A Implications of the Proposals: Resource Implications (Financial, IT, Staffing and Assets): N/A Legal Implications: N/A Equality Implications: There are no equality implications. Contribution to the Council’s Core Purpose: Protect the most vulnerable: Implementing the PSPO will help to identify -

Freshfield Station Interchange Information
Freshfield Station Interchange Information Formby Circulars Freshfield Interchange Map Monday to Saturday off-peak (0900-1600) Minutes past Travelling to Via Route Departure each hour Number Stop 00 Formby Village Halsall Lane 161 B 04 Formby Village Harington Road 160 A 30 Formby Village Freshfield Road 160 B 34 Formby Village Harington Road 161 A 49 Formby Village Ryeground Lane 162 D Monday to Saturday peak (0700-0900 and 1600-1900) Minutes past Travelling to Via Route Departure each hour Number Stop 00 Formby Village Halsall Lane 164 B 04 Alt Road Harington Road 164 A 30 Formby Village Halsall Lane 164 B 34 Alt Road Harington Road 164 A 49 Formby Village Ryeground Lane 162 D Sundays Minutes past Travelling to Via Route Departure each hour Number Stop 08 Formby Village Harington Road/ 165 A (1008 - 1708) Duke Street 31 Formby Village Ryeground Lane/ 165 D (1031 - 1731) Watchyard Lane Monday to Saturday 164 164 164 164 160 161 160 161 160 161 164 164 164 164 164 164 Freshfield Station stop A 0704 0734 0804 0834 0904 0934 04 34 1504 1534 1604 1634 1704 1734 1804 1834 Birch Green (for Nature Reserve) 0705 0735 0805 0835 0906 0936 06 36 1506 1536 1605 1635 1705 1735 1805 1835 Woodlands Primary School 0707 0737 0807 0837 0908 0938 08 38 1508 1538 1607 1637 1707 1737 1807 1837 Formby Station stop A 0709 0739 0809 0839 0910 0940 10 40 1510 1540 1609 1639 1709 1739 1809 1839 then at Formby Village Chapel Lane - - - - 0913 0943 13 43 1513 1543 - - - - - - these Alt Road, Romsey Avenue 0716 0746 0816 0846 0919 0949 19 49 1519 1549 1616 1646 -

Road Safety Concerns Outside Schools
Formby High School ‘Determined to Achieve’ Headteacher: DMA/LFO Mr D A Mackenzie BA (Hons) NPQH Freshfield Road Formby 28 February 2020 Liverpool L37 3HW 01704 873100 For the attention of parents of all FHS students enquiries@ formbyhighschool.com www. formbyhighschool.com Dear Parent @FormbyHigh Road Safety You may be aware that Formby High School is participating in a Formby wide initiative led by Andrew Drewary of Road Safety Smart to improve the safe use of all roads in our community and we will continue to support this initiative in whatever way possible. Thank you to those parents who engaged with the recent workshop delivered by Andrew Drewary and who have committed to be involved with Road Safety Smart as this project develops. Through the project, Andrew Drewary will be delivering a road safety awareness session to our Sixth Form students who are either learning to drive or have passed their driving test. This will take place on Wednesday 11 March. As part of our commitment to road safety, I would like to emphasise that we continue to experience considerable safety concerns around the school entrance due to congestion caused by vehicles dropping off and collecting students at the start / end of the school day. I would like to repeat my appeal to all parents to support us in promoting the safety of all our students and school community in the following ways: Encouraging your child to walk or cycle to school (particularly as the weather begins to improve). Dropping off / picking up further away from the school campus (ideally beyond Rosemary Lane / Old Town Lane) to avoid this dangerous congestion. -

Formby and Little Altcar Neighbourhood Development Plan
Formby and Little Altcar Neighbourhood Development Plan 2012 to 2030 Page| Page|02 FOREWORD Formby is a great town with a unique heritage and a dynamic future. Its uniqueness is due in part to its open areas of natural beauty, unrivalled coastal dunes and its local heritage. Investment and change in the years ahead will only be worthwhile if it makes a real difference to the lives of local people and the future of its community. The Formby and Little Altcar Neighbourhood Development Plan, [NDP] has been produced jointly by the Parish Councils of Formby and Little Altcar, starting back in September 2013. The Parish Councils wanted the people of Formby and Little Altcar to have a say in all aspects of the future of the town; addressing the issues surrounding housing, infrastructure, health and wellbeing, the environment, and natural/heritage assets. However, most importantly, it wanted local people to decide what they wanted in their community. The NDP sets out a vision for the area that reflects the thoughts and feelings of local people with a real interest in their community. It sets out objectives on key themes such as housing, employment, green space, moving around and community facilities and builds on current and future planned activities. The Parish Councils are committed to developing and strengthening contacts with the groups that have evolved because of the NDP process. We believe that by working together to implement the NDP it will make Formby an even better place to live, work and enjoy. We have had to ensure that our NDP is consistent, where appropriate, with the Sefton Local Plan, the February 2019 National Planning Policy Framework, subsequent updates, and guidance notes.