Critical Issues in Head and Neck Oncology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MEDICAL Injectables & ONCOLOGY TREND REPORT™
MEDICAL INJECTABLEs & ONCOLOGY TREND REPORT™ 2010 firsT edition ICORE HEALTHCARE www.ICOREHealthcare.com/Trends.AsPx letter to OuR readers 1 Injectable Drugs: Giving You the Data You Need It is my pleasure to present you with the 2010 ICORE For this first edition, we surveyed 60 medical, pharmacy, and Healthcare Medical Injectables & Oncology Trend clinical directors representing 146 million lives to get an understanding ReportTM. It is the first of what will be an annual of what payors are doing today and planning to do in the future to publication. The purpose of our investment in this manage the quality and cost of care for medical benefit injectables. report is straightforward: Back in 2003 when ICORE We then evaluated health plan medical benefit injectable claims such Healthcare first began assisting payors in managing that benchmarks and trends could be determined. medical injectables, no reference or benchmark data ICORE Healthcare’s mission has not changed in the past seven existed. Frankly, this has continued to be the case years: We serve as the center of medical injectable drug management. until the release of this report, since few, if any, benefit To this end, we believe this report is one additional resource to assist managers are able to review and assess medical benefit our customers, colleagues, and partners. injectable claims. I want to give special thanks to the Assessing medical injectable use, costs, and trends payors who served on our advisory is more critical now than ever, since five of the top board of this publication and 16 drugs in 2009 (based upon sales dollars) were who provided invaluable input specialty drugs, whereas it is expected that 11 drugs of into the report’s overall objective, the top 16 will be injectable or specialty products by content, and design. -

Nimotuzumab, an Antitumor Antibody That Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding While Permitting the Active Receptor Conformation
Published OnlineFirst July 7, 2009; DOI: 10.1158/0008-5472.CAN-08-4518 Experimental Therapeutics, Molecular Targets, and Chemical Biology Nimotuzumab, an Antitumor Antibody that Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding while Permitting the Active Receptor Conformation Ariel Talavera,1,2 Rosmarie Friemann,2,3 Silvia Go´mez-Puerta,1 Carlos Martinez-Fleites,4 Greta Garrido,1 Ailem Rabasa,1 Alejandro Lo´pez-Requena,1 Amaury Pupo,1 Rune F. Johansen,3 Oliberto Sa´nchez,5 Ute Krengel,2 and Ernesto Moreno1 1Center of Molecular Immunology, Havana, Cuba; 2Department of Chemistry, University of Oslo, Oslo, Norway; and 3Center for Molecular and Behavioral Neuroscience, Institute of Medical Microbiology, University of Oslo, Rikshospitalet HF, Oslo, Norway; 4Department of Chemistry, University of York, Heslington, York, United Kingdom; and 5Center for Genetic Engineering and Biotechnology, Havana, Cuba Abstract region of the EGFR (eEGFR), leaving the dimerization ‘‘arm’’ in Overexpression of the epidermal growth factor (EGF) receptor domain II ready for binding a second monomer (4, 5). It has been (EGFR) in cancer cells correlates with tumor malignancy and shown that the eEGFR adopts a ‘‘tethered’’ or inactive conformation poor prognosis for cancer patients. For this reason, the EGFR in the absence of EGF (6). In this characteristic conformation, has become one of the main targets of anticancer therapies. the dimerization arm is hidden by interactions with domain IV, Structural data obtained in the last few years have revealed whereas domains I and III remain separated. Thus, to adopt the the molecular mechanism for ligand-induced EGFR dimeriza- ‘‘extended’’ or active conformation observed in the crystal structure tion and subsequent signal transduction, and also how this of the complex with EGF (4), the receptor must undergo a major signal is blocked by either monoclonal antibodies or small conformational change that brings together domains I and III (6). -

Targeted and Novel Therapy in Advanced Gastric Cancer Julie H
Selim et al. Exp Hematol Oncol (2019) 8:25 https://doi.org/10.1186/s40164-019-0149-6 Experimental Hematology & Oncology REVIEW Open Access Targeted and novel therapy in advanced gastric cancer Julie H. Selim1 , Shagufta Shaheen2 , Wei‑Chun Sheu3 and Chung‑Tsen Hsueh4* Abstract The systemic treatment options for advanced gastric cancer (GC) have evolved rapidly in recent years. We have reviewed the recent data of clinical trial incorporating targeted agents, including inhibitors of angiogenesis, human epidermal growth factor receptor 2 (HER2), mesenchymal–epithelial transition, epidermal growth factor receptor, mammalian target of rapamycin, claudin‑18.2, programmed death‑1 and DNA. Addition of trastuzumab to platinum‑ based chemotherapy has become standard of care as front‑line therapy in advanced GC overexpressing HER2. In the second‑line setting, ramucirumab with paclitaxel signifcantly improves overall survival compared to paclitaxel alone. For patients with refractory disease, apatinib, nivolumab, ramucirumab and TAS‑102 have demonstrated single‑agent activity with improved overall survival compared to placebo alone. Pembrolizumab has demonstrated more than 50% response rate in microsatellite instability‑high tumors, 15% response rate in tumors expressing programmed death ligand 1, and non‑inferior outcome in frst‑line treatment compared to chemotherapy. This review summarizes the current state and progress of research on targeted therapy for advanced GC. Keywords: Gastric cancer, Targeted therapy, Human epidermal growth factor receptor 2, Programmed death‑1, Vascular endothelial growth factor receptor 2 Background GC mortality which is consistent with overall decrease in Gastric cancer (GC), including adenocarcinoma of the GC-related deaths [4]. gastroesophageal junction (GEJ) and stomach, is the ffth Tere have been several eforts to perform large-scale most common cancer and the third leading cause of can- molecular profling and classifcation of GC. -

The Antibody Zalutumumab Inhibits Epidermal Growth Factor Receptor Signaling by Limiting Intra- and Intermolecular Flexibility
The antibody zalutumumab inhibits epidermal growth factor receptor signaling by limiting intra- and intermolecular flexibility Jeroen J. Lammerts van Bueren*, Wim K. Bleeker*, Annika Bra¨ nnstro¨ m†, Anne von Euler†, Magnus Jansson†, Matthias Peipp‡, Tanja Schneider-Merck‡, Thomas Valerius‡, Jan G. J. van de Winkel*§, and Paul W. H. I. Parren*¶ *Genmab, 3508 AD, Utrecht, The Netherlands; †Sidec, SE-164 40 Kista, Sweden; ‡Division of Nephrology and Hypertension, Christian-Albrecht-University, 24105 Kiel, Germany; and §Immunotherapy Laboratory, Department of Immunology, University Medical Centre Utrecht, 3584 EA, Utrecht, The Netherlands Edited by Michael Sela, Weizmann Institute of Science, Rehovot, Israel, and approved February 7, 2008 (received for review October 8, 2007) The epidermal growth factor receptor (EGFR) activates cellular intervene in EGFR signaling, as reflected by two classes of pathways controlling cell proliferation, differentiation, migration, anti-EGFR drugs that are currently used clinically: tyrosine and survival. It thus represents a valid therapeutic target for kinase inhibitors (TKIs) and monoclonal antibodies (mAbs). treating solid cancers. Here, we used an electron microscopy-based TKIs represent small-molecule inhibitors that block EGFR- technique (Protein Tomography) to study the structural rearrange- kinase activity by binding to the ATP-binding pocket, thereby ment accompanying activation and inhibition of native, individual, abrogating downstream EGFR signaling. The effects of TKI EGFR molecules. Reconstructed tomograms (3D density maps) seem to be primarily related to enzyme inhibition. showed a level of detail that allowed individual domains to be For mAbs, the mechanisms of action are more diverse and discerned. Monomeric, resting EGFR ectodomains demonstrated their relative contribution to antitumor activity is still being large flexibility, and a number of distinct conformations were investigated. -

WV Graded Music List 2011
2011 WV Graded Music List, p. 1 2011 West Virginia Graded Music List Grade 1 Grade 2 Grade 3 Grade 4 Grade 5 Grade 6 Grade Artist Arranger Title Publisher 1 - Higgins, John Suo Gan HL 1 - McGinty Japanese Folk Trilogy QU 1 - McGinty, Anne Elizabethan Songbook, An KJ 1 - Navarre, Randy Ngiele, Ngiele NMP 1 - Ployhar Along the Western Trail BE 1 - Ployhar Minka BE 1 - Ployhar Volga Boat Song BE 1 - Smith, R.W. Appalachian Overture BE Variant on an Old English 1 - Smith, R.W. BE Carol 1 - Story A Jubilant Carol BE 1 - Story Classic Bits and Pieces BE 1 - Story Patriotic Bits and Pieces BE 1 - Swearingen Three Chorales for Band BE 1 - Sweeney Shenandoah HL 1 Adams Valse Petite SP 1 Akers Berkshire Hills BO 1 Akers Little Classic Suite CF 1 Aleicheim Schaffer Israeli Folk Songs PO 1 Anderson Ford Forgotten Dreams BE 1 Anderson Ford Sandpaper Ballet BE 1 Arcadelt Whiting Ave Maria EM 1 Arensky Powell The Cuckoo PO 1 Bach Gardner Little Bach Suite ST Grand Finale from Cantata 1 Bach Gordon BO #207 1 Bach Walters Celebrated Air RU 1 Bain, James L. M Wagner Brother James' Air BE 1 Balent Bold Adventure WB Drummin' With Reuben And 1 Balent BE Rachel 1 Balent Lonesome Tune WB 1 Balmages Gettysburg FJ 2011 WV Graded Music List, p. 2 1 Balmages Majestica FJ 1 Barnes Ivory Towers of Xanadu SP 1 Bartok Castle Hungarian Folk Suite AL 1 Beethoven Clark Theme From Fifth Symphony HL 1 Beethoven Foulkes Creation's Hymn PO 1 Beethoven Henderson Hymn to Joy PO 1 Beethoven Mitchell Ode To Joy CF 1 Beethoven Sebesky Three Beethoven Miniatures Al 1 Beethoven Tolmage -

The Two Tontti Tudiul Lui Hi Ha Unit
THETWO TONTTI USTUDIUL 20170267753A1 LUI HI HA UNIT ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2017 /0267753 A1 Ehrenpreis (43 ) Pub . Date : Sep . 21 , 2017 ( 54 ) COMBINATION THERAPY FOR (52 ) U .S . CI. CO - ADMINISTRATION OF MONOCLONAL CPC .. .. CO7K 16 / 241 ( 2013 .01 ) ; A61K 39 / 3955 ANTIBODIES ( 2013 .01 ) ; A61K 31 /4706 ( 2013 .01 ) ; A61K 31 / 165 ( 2013 .01 ) ; CO7K 2317 /21 (2013 . 01 ) ; (71 ) Applicant: Eli D Ehrenpreis , Skokie , IL (US ) CO7K 2317/ 24 ( 2013. 01 ) ; A61K 2039/ 505 ( 2013 .01 ) (72 ) Inventor : Eli D Ehrenpreis, Skokie , IL (US ) (57 ) ABSTRACT Disclosed are methods for enhancing the efficacy of mono (21 ) Appl. No. : 15 /605 ,212 clonal antibody therapy , which entails co - administering a therapeutic monoclonal antibody , or a functional fragment (22 ) Filed : May 25 , 2017 thereof, and an effective amount of colchicine or hydroxy chloroquine , or a combination thereof, to a patient in need Related U . S . Application Data thereof . Also disclosed are methods of prolonging or increasing the time a monoclonal antibody remains in the (63 ) Continuation - in - part of application No . 14 / 947 , 193 , circulation of a patient, which entails co - administering a filed on Nov. 20 , 2015 . therapeutic monoclonal antibody , or a functional fragment ( 60 ) Provisional application No . 62/ 082, 682 , filed on Nov . of the monoclonal antibody , and an effective amount of 21 , 2014 . colchicine or hydroxychloroquine , or a combination thereof, to a patient in need thereof, wherein the time themonoclonal antibody remains in the circulation ( e . g . , blood serum ) of the Publication Classification patient is increased relative to the same regimen of admin (51 ) Int . -

Portland Daily Press: April 23, 1898
PORTLAND DAILY JUNE 1832-VOL.35. SATURDAY ESTABLISHED 23, PORTLAND, MAINE, MORNING, APRIL 2'. 1898. IHHfSaaTiKSSK PRICE THREE CENTS. JliY BE LOST. BEST SPRING REMEDY TOFEKi S CY. SHERMAN TO REM ttWiLB LEAD A S^UAD. Rumor That She Was Sunk by a Gen. Lee Ready to Serve in Any Merchantman. Position. FOB TRE London, April £3.— It is rumored here CHILDREN. 23.—It is under, Present of State Richmond, Va., April the Will that United States cruiser Topeka Secretary stood here that General Lee will unqnes- formerly the Diogenes foundered Tues- sionably be made a Major General in the day night in collision with the hark Al- His United States volunteer army and will The Perfect Haaitii of a Is Due to the Use of batross. Abdicate Post Soon. Large Family lead a division or corps m Cuba. He wiil Falmouth, April 22.—Captain Port-son leave for Washington Sunday if not or. of the Swedish bark Albatross from Mo- iered there sooner and immediately apon bile for Dundee, towed in here yesterday receiving his commission will select his Paine’s damaged from collision at midnight of Celery Compound. staff of nine men. the 19th about sixty miles southwest of When asked if the Virginia troops Scilly iclands, with an unknown vessel, SAILED FOR MANILA. would be attached to his command ha says that he believes that the vessel collid- stated unhesitatingly that they would he, with him was a steamer she f^k JiRk ing and that and 1) April 23. Xlie American at it has leaked out that he wired to London, Squadron Hong Kong, according to a special had foundered, for after she had flashed despatch from Shanghai has sailed for Manila, which it will attack. -

The Republican Journal: Vol. 71, No. 23
The Republican Journal. Mi 7K___ BELFAST, MAINE. THURSDAY, JUNE 8, 1890. > NUMBER 23. years old and there are but few of The girls Waldo Co. Veteran Association. OBITUARY. News of the that age who can boast of earning their Oranges. PERSONAL. PERSONAL. new wheel.The track at the State fair The Waldo Plain, Mass., County Veteran Association Died, in Jamaica May 31st, Union Harvest Centre Mrs. Rose grounds at Lewiston has been to the met Grange, Montville, Fahy went to Boston last E. L. Smith of is K\ Tlil RSPAV J«ORM.NO BY THE open with the at formerly of Chelsea, Mass., visiting people East Thorndike Frank Fletcher, Belmont, aged initiated three new members at trainers, and the indications are that June the last Thursday. in Belfast. 1st. The weather 4 The deceased was a number of fast horses will h# was all that could 54 years and mouths. meeting. large »e Mrs. Allen Orcutt is friends jiican Journal Pub. Co, desired aud noon two 27, the son of the visiting in Mrs. Ann M. returned to q,, trained there the sea- by fully hundred born in Belmont, Jan. 1845, The National has Cbenery Boston during coming j Grange sent out to the Rockland. sou. veterans and their families had last Saturday. assembled. late Samuel and Hannah (Bicknell) Fletcher. subordinate granges a number of petitions ! HI: PAPER for Maine Seafar- The following towns were : Ban- In he married Kezia Knowles of Bel- to Dr. G. W. Stoddard spent with represented 1865 Congress for the signatures of the mem- Sunday Miss Daisy Taylor of New York is gor, visiting ing People.” In Bkikf. -

Blssii Great Lakes Maritime Institute
TELESCOPE May, 1966 Volume 15, Number 5 B lS S Ii Great Lakes Maritime Institute Dossin Great Lakes Museum, Belle Isle, Detroit 7, Michigan May May Cover: £ G e z in a B r ov i g Below, left: TELESCOPE Seaway Salties 4: Gosforth Below, right: Marg it Brovig Lists compiled by Donald Baut and George Ayoub - -Ma s sman with photographs by Emory Massman and others photographs LIST ONE: Compiled by FLAGS represented Be Belgium Gh Ghana No Norway Br Great Britain Gr Greece Pa Panama Donald Baut Ca Canada In India Sp Spain Da Denmark Ir Ireland Ss Switzerland Du Netherlands Is Israel Sw Sweden Fi Finland It Italy BAR United Arab Republic Fr France Ja Japan US United States Ge West Germany De Lebanon Yu Yugoslavia 1964 Li Liberia N U M B E R OF Atheltemplar (Br) Athel Line Ltd. 496x64 1951 0-1-0-2-2-1 PASSAGES Atlantic Duke (Li) Atlantic Tankers Ltd. 529x70 1952 0-0-0-0-0-3 Augvald (No) Skibs A/S Corona 467x61 1958 0-0-0-1-0-1 cO CO cO cO cO cO en O) oi O' O' O' iO O K to U Jk Baltic Sea (Sw) Wm. Thozen, Mgr. 444x56 1960 0-0-2-2-2-1 a Bambi (No) D/S A/S Bananfart 293x45 1957 1-2-3-1-0-1 A & J Faith (US) Pacific Seafarers Inc. 459x63 194 6 0-0-0-0-3-1 Bannercliff (Br) Bond Shipping Co. Ltd. 455x58 1948 0-0-0-0-1-1 A & J Mercury (US) Pacific Steamers Inc. -
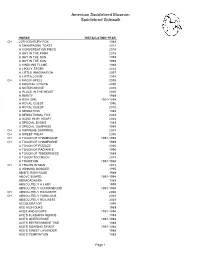
Saddlebred Sidewalk List 1989-2018
American Saddlebred Museum Saddlebred Sidewalk HORSE INSTALLATION YEAR CH 20TH CENTURY FOX 1989 A CHAMPAGNE TOAST 2011 A CONVERSATION PIECE 2014 A DAY IN THE PARK 2018 A DAY IN THE SUN 1999 A DAY IN THE SUN 1998 A KINDLING FLAME 1989 A LIKELY STORY 2014 A LITTLE IMAGINATION 2007 A LOTTA LOVIN' 1998 CH A MAGIC SPELL 2005 A MAGICAL CHOICE 2000 A NOTCH ABOVE 2016 A PLACE IN THE HEART 2000 A RARITY 1989 A RICH GIRL 1991-1994 A ROYAL QUEST 1996 A ROYAL QUEST 2010 A SENSATION 1989 A SENSATIONAL FOX 2002 A SONG IN MY HEART 2004 A SPECIAL EVENT 1989 A SPECIAL SURPRISE 1998 CH A SUPREME SURPRISE 2001 CH A SWEET TREAT 2000 CH A TOUCH OF CHAMPAGNE 1991-1994 CH A TOUCH OF CHAMPAGNE 1989 A TOUCH OF PIZZAZZ 2006 A TOUCH OF RADIANCE 1995 A TOUCH OF TENDERNESS 1989 A TOUCH TOO MUCH 2018 A TRADITION 1991-1994 CH A TRAVELIN' MAN 2012 A WINNING WONDER 1995 ABIE'S IRISH ROSE 1989 ABOVE BOARD 1991-1994 ABRACADABRA 1989 ABSOLUTELY A LADY 1999 ABSOLUTELY COURAGEOUS 1991-1994 CH ABSOLUTELY EXQUISITE 2005 CH ABSOLUTELY FABULOUS 2001 ABSOLUTELY NO LIMITS 2001 ACCELERATOR 1998 ACE HIGH DUKE 1989 ACES AND EIGHTS 1991-1994 ACE'S FLASHING GENIUS 1989 ACE'S QUEEN ROSE 1991-1994 ACE'S REFRESHMENT TIME 1989 ACE'S SOARING SPIRIIT 1991-1994 ACE'S SWEET LAVENDER 1989 ACE'S TEMPTATION 1989 Page 1 American Saddlebred Museum Saddlebred Sidewalk HORSE INSTALLATION YEAR ACTIVE SERVICE 1996 ADF STRICTLY CLASS 1989 ADMIRAL FOX 1996 ADMIRAL'S AVENGER 1991-1994 ADMIRAL'S BLACK FEATHER 1991-1994 ADMIRAL'S COMMAND 1989 CH ADMIRAL'S FLEET 1998 CH ADMIRAL'S MARK 1989 CH ADMIRAL'S MARK -

The Erbb/HER Family of Protein-Tyrosine Kinases and Cancer
Pharmacological Research 79 (2014) 34–74 Contents lists available at ScienceDirect Pharmacological Research jo urnal homepage: www.elsevier.com/locate/yphrs Invited Review The ErbB/HER family of protein-tyrosine kinases and cancer ∗ Robert Roskoski Jr. Blue Ridge Institute for Medical Research, 3754 Brevard Road, Suite 116, Box 19, Horse Shoe, NC 28742, USA a r t i c l e i n f o a b s t r a c t Article history: The human epidermal growth factor receptor (EGFR) family consists of four members that belong to the Received 7 November 2013 ErbB lineage of proteins (ErbB1–4). These receptors consist of a glycosylated extracellular domain, a sin- Accepted 8 November 2013 gle hydrophobic transmembrane segment, and an intracellular portion with a juxtamembrane segment, a protein kinase domain, and a carboxyterminal tail. Seven ligands bind to EGFR including epidermal This paper is dedicated to the memory of growth factor and transforming growth factor ␣, none bind to ErbB2, two bind to ErbB3, and seven lig- Dr. John W. Haycock (1949–2012) who ands bind to ErbB4. The ErbB proteins function as homo and heterodimers. The heterodimer consisting of prompted the author to write a review on the treatment of malignant diseases with ErbB2, which lacks a ligand, and ErbB3, which is kinase impaired, is surprisingly the most robust signaling targeted protein kinase inhibitors. complex of the ErbB family. Growth factor binding to EGFR induces a large conformational change in the extracellular domain, which leads to the exposure of a dimerization arm in domain II of the extracellular Chemical compounds studied in this article: segment. -

High Turnover of Tissue Factor Enables Efficient Intracellular Delivery of Antibody-Drug Conjugates Bart ECG De Goeij1, David Sa
Author Manuscript Published OnlineFirst on February 27, 2015; DOI: 10.1158/1535-7163.MCT-14-0798 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. High turnover of Tissue Factor enables efficient intracellular delivery of antibody-drug conjugates Bart ECG de Goeij1, David Satijn1, Claudia M Freitag1, Richard Wubbolts2, Wim K Bleeker1, Alisher Khasanov3, Tong Zhu3, Gary Chen3, David Miao3, Patrick HC van Berkel1 and Paul WHI Parren1,4 1 Genmab, Yalelaan 60, 3584 CM, Utrecht, The Netherlands 2 Department of Biochemistry and Cell Biology, Faculty of Veterinary Medicine, Utrecht University, Yalelaan 2, 3584 CM, Utrecht, The Netherlands 3 Concortis Biosystems Corp., San Diego, 11760 Sorrento Valley, CA 92121, USA 4 Dept. of Cancer and Inflammation Research, Institute of Molecular Medicine, University of Southern Denmark, Odense, Denmark Running title: Tissue Factor antibody-drug conjugate Key words: Tissue Factor, antibody-drug conjugate, internalization Corresponding author: Bart ECG de Goeij Genmab B.V. Yalelaan 60 3584CM Utrecht The Netherlands [email protected] +31 (0) 302123181 Conflict of interest statement: BECGG, DS, CMF, WKB, PHCB and PWHI are Genmab employees and own Genmab warrants and/or stock. 1 Downloaded from mct.aacrjournals.org on September 23, 2021. © 2015 American Association for Cancer Research. Author Manuscript Published OnlineFirst on February 27, 2015; DOI: 10.1158/1535-7163.MCT-14-0798 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract Antibody drug conjugates (ADC) are emerging as powerful cancer treatments that combine antibody-mediated tumor targeting with the potent cytotoxic activity of toxins.