Working Group DE Report, and the Working Group DE Report Resulting from the Fraser Health Authority Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
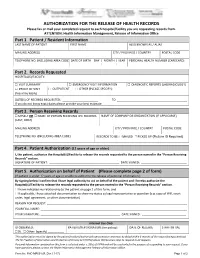
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -
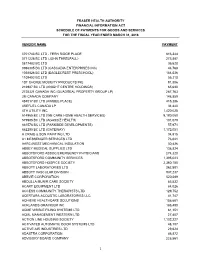
2018 Schedule of Vendor Payments.Xlsx
FRASER HEALTH AUTHORITY FINANCIAL INFORMATION ACT SCHEDULE OF PAYMENTS FOR GOODS AND SERVICES FOR THE FISCAL YEAR ENDED MARCH 31, 2018 VENDOR NAME PAYMENT 0701743 BC LTD - FERN RIDGE PLACE 816,344 0771226 BC LTD (JOHN THRELFALL) 273,887 0817482 BC LTD 36,628 0986305 BC LTD (CASCADIA ENTERPRISES INC) 44,768 1038826 BC LTD (EAGLECREST PRESCHOOL) 184,036 1109402 BC LTD 56,210 1ST CHOICE MOBILITY PRODUCTS INC 91,806 216987 BC LTD (KNIGHT CENTRE HOLDINGS) 65,630 2725321 CANADA INC (QUADREAL PROPERTY GROUP LP) 287,763 3M CANADA COMPANY 148,859 484017 BC LTD (KIMBEE PLACE) 415,386 4REFUEL CANADA LP 34,440 4TH UTILITY INC 1,420,028 514965 BC LTD (WE CARE HOME HEALTH SERVICES) 9,180,060 579985 BC LTD (AGASSIZ HEALTH) 101,079 661576 BC LTD (PARKSIDE DEVELOPMENTS) 57,971 662290 BC LTD (GATEWAY) 1,172,051 A CRAIG & SON PAINTING LTD 34,915 A1 MESSENGER SERVICES LTD 76,041 AARC-WEST MECHANICAL INSULATION 30,426 ABBEY MEDICAL SUPPLIES LTD 138,824 ABBOTSFORD ASSOC EMERGENCY PHYSICIANS 274,320 ABBOTSFORD COMMUNITY SERVICES 1,395,023 ABBOTSFORD HOSPICE SOCIETY 2,360,180 ABBOTT LABORATORIES LTD 262,801 ABBOTT VASCULAR DIVISION 937,237 ABBVIE CORPORATION 520,589 ABDULLA MUNIR CARE SOCIETY 85,532 ACART EQUIPMENT LTD 84,026 ACCESS COMMUNITY THERAPISTS LTD 129,752 ACERTARA ACOUSTIC LABORATORIES LLC 41,747 ACHIEVE HEALTHCARE SOLUTIONS 158,681 ACKLANDS-GRAINGER INC 185,490 ACME VISIBLE FILING SYSTEMS LTD 81,151 ACML MANAGEMENT WESTERN LTD 27,457 ACTION LINE HOUSING SOCIETY 1,102,227 ACTIVATED AUTOMATIC DOOR SYSTEMS LTD 48,107 ACTIVE AIR INDUSTRIES LTD 29,624 -

Residential Care in Fraser Health
RESIDENTIAL CARE i n FRASER HEALTH Choices for adults who need 24-hour nursing care, personal care assistance and support TABLE OF CONTENTS About residential care 1 Options for residential care Subsidized 2 Private Pay 3 The first step toward moving to subsidized residential care Moving from home 4 Moving from hospital or temporary care 5 Preparing for the move to a residential care facility Before the move 6 Settling into the residential care setting 7 Moving to another residential care facility or to more independent living 8 Typical living costs in residential care 8 Some commonly used terms 9 Notes 11 Further Information inside back cover RESIDENTIAL CARE i n FRASER HEALTH About residential care IS RESIDENTIAL CARE THE RIGHT CHOICE? When a person’s ongoing health care needs become more complex, When the amount of daily a residential care facility may become the best health care choice. care needed is more than Residential care is sometimes also referred to as intermediate care, can be safely managed at extended care, special care or a nursing home. home, or in a supportive Residential care provides: or assisted living setting, a safe and secure living environment residential care may be 24-hour nursing care, personal care the most appropriate assistance and support nutritious meals care option. basic linen and personal laundry services recreational and activity programs Fraser Health operates and funds many residential care facilities, which together accommodate more than 7,500 adults throughout Fraser Health communities. All residential facilities in British Columbia operate within and provide care that meets established standards. -

Fraser Health Together
Fraser Health Together Fraser Health’s online booking tool is going through important maintenance to ensure there is a comprehensive transition to the provincial online booking and registration system set to launch on April 6th. This information is for your convenience please click on the link to be directed to the Fraser Health website for the most current updates: https://www.fraserhealth.ca/vaccine#.YGS-6a9KiUn Booking your immunization appointment if you live in the Fraser Health region Effective immediately, and until 7:00 a.m. on April 6, eligible people in the Fraser Health region* who would like to book their COVID-19 immunization appointment can do so one of two ways: • Between 7:00 am and 7:00 p.m. (Daytime): Call our immunization booking phone line at 1-855-755-2455. The phone line will operate from 9:00 a.m. to 5:00 p.m. on Friday, April 2 and Monday, April 5 to align with the statutory holidays. • Between 7:00 pm and 7:00 a.m. (Nighttime): Access Fraser Health’s self-serve online booking tool. The online tool will operate from 5:00 p.m. to 9:00 a.m. on Friday, April 2 and Monday, April 5. On Saturday, April 3 and Sunday, April 4 it will run from 7:00 pm to 7:00 am. To date we have booked just over 222,070 immunization appointments and we acknowledge that people in our communities want to book appointments as quickly as they become eligible. We appreciate everyone’s patience as we schedule very sizable populations into immunization appointments. -

COVID-19 School Cluster and Transmission Analysis
COVID-19 school cluster and transmission analysis May 7, 2021 1 Purpose Retrospective analysis of COVID-19 cases in K-12 school settings to determine clusters and transmission dynamics 2 Inclusion criteria COVID-19 cases reported to Public Health between January 1 and March 7, 2021 in students and staff who attended school (K- 12 public/independent) 3 Methods . Identified all schools with >1 case within a 14-day period (excluding cases from the same household) . Determined whether in-school transmission occurred based on standardized transmission/acquisition definitions . Cases reviewed by team of epidemiologists, analysts and MHO over 6 week period . MHO consulted for complex and ambiguous cases 4 Definitions . Suspect in-school acquisition/transmission defined as: . Case attended school during acquisition period . Case has no known exposure to a household or community case with symptom onset two or more days earlier . Possible in-school acquisition/transmission event defined as: . Suspect definition above AND . When 2 or more cases within the same classroom/admin areas/school bus/other school supervised venue or activity or with confirmed contact between cases in school based setting with similar symptom onset within 2 calendar day window without any other known acquisition . Likely in-school acquisition/transmission defined as: . Suspect definition above AND . Acquisition period of case overlaps with infectious period of another case in the same classroom/admin areas/school bus/other school supervised venue or activity or with confirmed contact between cases in school based setting *Does not include cases who were en route to school together (e.g. car-pooled or walking – excludes school bus use) as these are considered as community transmission and not issues with school based safety measures. -

Harm Reduction Supply Distribution Sites
Harm Reduction Supply Distribution Sites Below are possible points to access and dispose of harm reduction supplies in Fraser Health. These agencies may be able to refer to additional places to get supplies including health care providers as part of their confidential clinical practice. Provincial policy mandates provision of harm reduction supplies and services and they are an integral component of prevention, treatment, and health care for people dependent on and/or who use substances. FRASER EAST ORGANIZATION CONTACT INFO HOURS OF OPERATION Abbotsford 5 and 2 Ministries 604-798-7332 Various Hours Monday- Saturday Mobile Outreach call for access and look for van with logo Abbotsford Community Services 604-850-5106 Monday - Friday: 8:30am - 4:30pm #202 31943 South Fraser Way Abbotsford Public Health Unit 604-864-3400 Monday - Friday: 8:30am - 4:30pm #104 34194 Marshall Road Positive Living Fraser Valley 604-854-1101 (office) Mobile Outreach: 604-556-6228 (mobile) Monday, Wednesday, Friday: 9:30am - 12:00pm #108 32883 South Fraser Way PARC Drop-in Supplies Monday, Tuesday, Thursday, Friday: 12:00pm - 4:00pm Wednesday: 9:30am - 4:00pm Women’s Resource Society of the Fraser Valley, 604-746-3301 Monday - Friday Warm Zone 33264 Old Yale Road 12:00pm - 7:00pm Drop-in 9:00am - 12:00pm Call 604-217-3033 for supplies *Note: increased hours coming soon Mission Mission Friendship Centre Society 604-826-1281 ext. 112 Monday - Friday: 8:30am - 4:30pm. 33150A First Avenue Please check with receptionist first Mission Public Health Unit 604-814-5500 -

Induction of Labour When Labour Needs to Be Started
Induction of labour When labour needs to be started For most women labour starts on its own. For some Why would labour be induced? women, labour needs help to get started. Times when we consider inducing labour: ‘Induction’ is when we start or ‘induce’ labour for Your pregnancy is 7 days or more past your you. This is usually done when your doctor or due date. midwife (care provider) feels the risks to you or The bag of water around the baby breaks your baby are greater than the risk of carrying on before labour starts. with the pregnancy. Your baby is growing too slowly. Induction of labour is generally safe. However, as The fluid around the baby is low. with any medical procedure or medicine, there are possible risks. Your care provider will explain You have a medical illness (such as high blood these to you. pressure, or diabetes) that might affect you or your baby’s health. How is labour induced? . Prostaglandin Gel . Oxytocin This medicated gel is put into your vagina. It We give this medication into a vein in your arm. softens the cervix and helps start contractions. This is called an intravenous (or IV). You stay in We observe you and your baby for at least 1 the hospital until your baby is born. We check hour. You stay in bed for the hour to make sure you and your baby often during this time. the gel has time to absorb. You will not be able to . Breaking the water sac (rupturing the membranes) eat or drink during this time. -

Inflammatory Arthritis Clinic
Other Arthritis Rehab Services CONTACT US in the Lower Mainland Inflammatory Arthritis Clinic Surrey Memorial Hospital Publicly funded arthritis clinics with Rehabilitation Department Inflammatory physiotherapy and occupational B building basement level 13750 96 Avenue Surrey B.C. V3V 1Z2 therapy include: Arthritis Clinic Mary Pack Arthritis Program Ph. 604 585 5666 ext 778778 (Vancouver) Richmond Hospital Arthritis Clinic Lions Gate Hospital Arthritis Surrey Memorial Clinic (North Vancouver) Hospital OASIS clinics for osteoarthritis (Richmond, Vancouver, North Vancouver) Burnaby Hospital Arthritis Program A doctor referral is required. Arthritis Resources The Arthritis Society: www.arthritis.ca Mary Pack Arthritis Centre: www.mpap.vch.ca www.fraserhealth.ca www.rheuminfo.com © August 2017 Rehabilitation Subtitle Subtitle Sed tellus lorem, semper id felis non, Mauris condimentum pharetra tempor dolor. Aliquam condimentum ligula, a maximus feugiat venenatis leo, at hendrerit mauris fringilla eget. Mauris nec Title of massa posuere sed. posuere nulla. In hac habitasse Sed ut sollicitudin ex. Donec fringilla platea dictumst. ante nec lectus laoreet facilisis. Ut Brochure eleifend gravida nulla, viverra laoreet Curabitur feugiat justo eget leo lectus eleifend ac. hendrerit tristique. Maecenas venenatis sollicitudin ornare. Nam Proin ut faucibus urna. at nisi a quam ornare mollis eu Subtitle nec eros. Ut ac enim vel odio Fusce at leo vulputate, finibus leo tristique pulvinar vel sed sem. quis, eleifend urna. Additional info Morbi ac purus a libero ornare Etiam magna nulla, rhoncus sed facilisis. posuere ut, tempus sed libero. Nullam id leo aliquet, tristique Nunc sit amet fringilla odio. nibh vel, sodales mi. Quisque luctus facilisis dolor, id aliquam ligula posuere quis. Quisque eu arcu rutrum, semper dui ut, egestas tellus. -

Bulletinfrom Environmental Health Services
BULLETINFrom Environmental Health Services How to Complete Your Application for Health Approval ¾ Who needs to complete an application? Anyone who operates one of the following types of businesses in Fraser Health must complete an “Application for Health Approval”. Food (restaurant, food store, food processing, mobile vehicle, mobile cart) All mobile outdoor food service equipment, that is either propane or gas fired, must bear the approval decal from the BC Safety Authority or certified by an organization recognized by the “Standards Council of Canada.” Pool (swimming pool, hot tub, spray pool) Personal Service Establishment (hair salon, esthetics, body piercing, tattooing) Note: If you are applying for an Approval for Water Supply System you must complete a “Drinking Water Operating Permit Application” form, which is available at: www.fraserhealth.ca/drinkingwater. ¾ Why do I need to complete an application? A completed application is required before the Environmental Health Officer will approve your business to operate or issue a “Health Operating Permit”. ¾ What information do I need to provide on the application form? Follow the “4 Steps” for completing the application for health approval 1. Complete the following: form inside this bulletin. Owner information Site, billing and mailing addresses Type of Application for Health Approval Type of Service 2. Contact your local Environmental Health Officer if you have questions. 3. In the signature section, print and sign your name and write the date. 4. Submit the completed form to your Environmental Health Officer or forward to the local Health Protection office. Health Protection | Ensuring Healthy People and Healthy Environments Printshop #256167 July 2019 How to complete your Application for Health Approval Step 1: Complete Owner Information ¾ Type of Ownership Check the box next to the type of ownership that describes your business. -

Annual Report 2015 | 2016 TABLE of CONTENTS OVERVIEW of the DEPARTMENT of MEDICINE Heads and Directors
UNIVERSITY OF BRITISH COLUMBIA DEPARTMENT OF MEDICINE Annual Report 2015 | 2016 TABLE OF CONTENTS OVERVIEW OF THE DEPARTMENT OF MEDICINE Heads and Directors.................................................................... 2 Committees................................................................................... 3 Administration.............................................................................. 11 RESEARCH Activities....................................................................................... 12 Research Metrics and Highlights............................................ 12 EDUCATION UNIVERSITY OF BRITISH COLUMBIA Accomplishments and Highlights........................................... 13 DEPARTMENT OF MEDICINE Undergraduate Medical Education Program (UGME)....... 13 Annual Report 2015 | 2016 Postgraduate Medical Education Program (PGME)........... 13 Experimental Medicine.............................................................. 16 Dr. Graydon S. Meneilly, MD, FRCPC, MACP DIVISION REPORTS Professor and Eric W. Hamber Chair AIDS................................................................................................ 17 Head, UBC Department of Medicine Allergy and Immunology.......................................................... 20 Physician-in-Chief & Head, Cardiology.................................................................................... 22 Community Internal Medicine................................................ 25 Department of Medicine Critical Care Medicine.............................................................. -

Burnaby, Belcarra, Anmore, Port Moody, Maple Ridge Areas Abbotsford, Mission, Chilliwack, Hope Areas
Date Results Posted: July 5, 2019 Single Sample (<400 Geometric Mean Unsatisfactory Based on Name of Beach E.coli/100mls) (<200 E.coli/100mls) Another Condition: Abbotsford, Mission, Chilliwack, Hope Areas Albert Dyck Lake - Public Beach West End 15 14 Albert Dyck Lake - Public Beach East End 5 11 Camp Luther (Hatzic Lake) 5 5 Cultus Lake - Entrance Bay Beach 5 Cultus Lake - Main Beach 5 5 Cultus Lake- Maple Bay Beach 5 Cultus Lake - Spring Bay Beach 20 Harrison Bay Beach - Cabin Dock 5 Harrison Lake Beach - Left Of The Lagoon 5 Harrison Lake Lagoon - Centre 20 Harrison Lake Lagoon - East 60 Harrison Lake Lagoon - West 10 Hope Public Beach - Kawkawa Lake 10 7 Lake Errock Beaches 5 7 Lake Of The Woods Beach - Highway Stop 5 5 Rolley Lake Provincial Park Beach 5 6 Sasquatch Provincial Park - Deer Lake - Lakeside Dock 5 Sasquatch Provincial Park - Green Point - Picnic Area - Harrison Lake 10 Sasquatch Provincial Park - Hicks Lake Day Use Beach 5 Burnaby, Belcarra, Anmore, Port Moody, Maple Ridge Areas Barnet Marine Park Beach 1835 36 Bedwell Bay 31 12 Belcarra Park 231 31 Buntzen Lake - North Beach - End Of Dock 5 Buntzen Lake - South Beach - Centre 20 Buntzen Lake - South Beach - Dog Area 5 Buntzen Lake - South Beach - East End 5 Buntzen Lake - South Beach - Floating Bridge 25 Buntzen Lake - South Beach - West 14 Davidson Pool Beach 70 Golden Ears Provincial Park - Campground Beach North 5 5 Golden Ears Provincial Park - Campground Beach South 5 5 Golden Ears Provincial Park - Day Beach North 5 5 Golden Ears Provincial Park - Day Beach South 10 5 Old Orchard Park Beach 97 34 White Pine Beach - Main Beach North 20 12 White Pine Beach - Family Beach South 31 16 White Pine Beach - Swim Dock 10 10 White Pine Beach - Sasamat Outdoor Centre 20 13 Whonnock Lake Beach - West Beach 1050 146 Whonnock Lake Beach 285 86 Centennial Beach 10 10 Crescent Beach 10 12 Crescent Beach-North 10 15 White Rock Beach-East Of Pier 20 12 White Rock Beach-West Of Pier 10 20. -

Fraser Health Authority
Consolidated Financial Statements of FRASER HEALTH AUTHORITY Year ended March 31, 2011 ABCD KPMG Enterprise™ Telephone (604) 527-3600 Metrotower II Fax (604) 527-3636 Suite 2400 - 4720 Kingsway Internet www.kpmg.ca/enterprise Burnaby BC V5H 4N2 Canada INDEPENDENT AUDITORS' REPORT To the Board of Fraser Health Authority We have audited the accompanying consolidated financial statements of the Fraser Health Authority ("the Entity"), which comprise the consolidated statement of financial position as at March 31, 2011 the consolidated statements of operations, changes in net assets (deficiency) and cash flows for the year then ended, and notes, comprising a summary of significant accounting policies and other explanatory information. Management's Responsibility for the Financial Statements Management is responsible for the preparation and fair presentation of these consolidated financial statements in accordance with Canadian generally accepted accounting principles, and for such internal control as management determines is necessary to enable the preparation of financial statements that are free from material misstatement, whether due to fraud or error. Auditor's Responsibility Our responsibility is to express an opinion on these consolidated financial statements based on our audit. We conducted our audit in accordance with Canadian generally accepted auditing standards. Those standards require that we comply with ethical requirements and plan and perform an audit to obtain reasonable assurance about whether the consolidated financial statements are free from material misstatement. An audit involves performing procedures to obtain audit evidence about the amounts and disclosures in the financial statements. The procedures selected depend on the auditor's judgment, including the assessment of the risks of material misstatement of the financial statements, whether due to fraud or error.