2ND Common Review Mission
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accepted .Pdf
Accepted List of Accepted Application Form of Candidates for Interview for Class-IV Vacancies for Advertisement No. 01/15 dated 29.12.2015 Sl. Registration Name of Applicant Father's Name Qualificat Correspondence Address Date of Interview Time of Interview Post Sex Date of Birth Category No. No/ Roll No. applied for ion PUNAM KUMARI SHISHANKAR RAJAWAR HINU,C/5,PO-HINU,PS- 31-08-2016 08:00:00 AM DORANDA,DIST-RANCHI, 1 000002 PEON F 02/01/1990 SC MATRIC JHARKHAND,- 834002 KUNTI KUMARI KHAITA RAJAWAR HINU,C/59,PO-HINU,PS- 31-08-2016 08:00:00 AM DORANDA,DIST-RANCHI,JHARKHAND 2 000003 PEON F 02/10/1993 SC MATRIC PIN-834002 SANJAY KUMAR KINDO LATE BUDHRAM KINDO VILL-KATHAR GONDA,INDRAPURI 31-08-2016 08:00:00 AM ROAD NO-06,PO-HEHAL,DIST- 3 000004 PEON M 11/12/1976 ST BA RANCHI,JHARKHAND,PIN-834005 SANJAY KUMAR VERMA NAKUL MAHATO VILL-DHURGADGI,PO-TARA,PS- 31-08-2016 08:00:00 AM JAMUA,DIST- 4 000006 PEON M 03/01/1985 BC-2 BA GIRIDIH,JHARKHAND,PIN-815318 WAKIL FAJILAT HUSSAIN DORANDA BAILDAR 31-08-2016 08:00:00 AM MUHALLA,DORANDA,,PO- 5 000007 PEON M 05/06/1987 OBC MATRIC DORANDA,PS-DORANDA,RANCHI, JHARKHAND VIKASH KUMAR ARJUN SAW VILL-CHOTKI BARHI,PO-RASOIA 31-08-2016 08:00:00 AM DHAMNA,PS-BARHI,DIST- 6 000009 PEON M 20-10-1987 BC-1 MA HAZARIBAGH,JHARKHAND,PIN- 825405 KUMAR LAW KUSH RAMDHANI PRASAD BHATTIMUHALLA,DEVI MANDIR, 31-08-2016 08:00:00 AM DALTONGANJ,PALAMAU,JHARKHAND 7 000011 PEON M 01/06/1984 OBC MATRIC ,PIN-822101 AMRESH YADAV ALAKHDEV YADAV PO-KUNDA,PS-KUNDA,DIST- 31-08-2016 08:00:00 AM 8 000013 PEON M 09/03/1990 OBC-2 INTER CHATRA,JHARKHAND -
Scheme N Volume 2) (Transmission Lines Associated with GSS at Chhatarpur
Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Environment and Social Impact Assessment Report (Scheme N Volume 2) (Transmission Lines Public Disclosure Authorized Associated with GSS at Chhatarpur) Jharkhand Urja Sancharan Nigam Limited Final Report January 2019 www.erm.com The Business of Sustainability FINAL REPORT Jharkhand Urja Sancharan Nigam Limited Environment and Social Impact Assessment Report (Scheme N Volume 2) (Transmission Lines Associated with GSS at Chhatarpur) 10 January 2019 Reference # 0402882 Suvankar Das Consultant Prepared by Abhishek Roy Goswami Senior Consultant Reviewed & Debanjan Approved by: Bandyapodhyay Partner This report has been prepared by ERM India Private Limited a member of Environmental Resources Management Group of companies, with all reasonable skill, care and diligence within the terms of the Contract with the client, incorporating our General Terms and Conditions of Business and taking account of the resources devoted to it by agreement with the client. We disclaim any responsibility to the client and others in respect of any matters outside the scope of the above. This report is confidential to the client and we accept no responsibility of whatsoever nature to third parties to whom this report, or any part thereof, is made known. Any such party relies on the report at their own risk. TABLE OF CONTENTS EXECUTIVE SUMMARY I 1 INTRODUCTION 1 1.1 BACKGROUND 1 1.2 PROJECT OVERVIEW 1 1.3 PURPOSE AND SCOPE OF THIS ESIA 2 1.4 STRUCTURE OF THE REPORT 2 1.5 LIMITATION -

Government of Jharkhand Office of the Accountant General (Audit)
Annual Technical Inspection Report on Local Bodies for the year ended 31 March 2016 Government of Jharkhand Office of the Accountant General (Audit), Jharkhand, Ranchi TABLE OF CONTENTS Reference to Paragraph Page Preface v Overview vii PART – A CHAPTER – I AN OVERVIEW OF THE FUNCTIONING, ACCOUNTABILITY MECHANISM AND FINANCIAL REPORTING ISSUES OF PANCHAYATI RAJ INSTITUTIONS Introduction 1.1 1 Organisational setup of Panchayati Raj Institutions 1.2 2 Functioning of Panchayati Raj Institutions 1.3 3 Formation of various committees 1.4 4 Audit arrangement 1.5 5 Response to Audit Observations 1.6 6 Ombudsman 1.7 7 Social Audit 1.8 7 Submission of Utilisation Certificates 1.9 8 Internal Audit and Internal Control System of Panchayati Raj 1.10 8 Institutions Financial Reporting Issues 1.11 8 CHAPTER – II COMPLIANCE AUDIT – PANCHAYATI RAJ INSTITUTIONS RURAL DEVELOPMENT DEPARTMENT (PANCHAYATI RAJ) Audit on Construction activities by the Panchayati Raj Institutions in 2.1 15 the State of Jharkhand PART – B CHAPTER – III AN OVERVIEW OF THE FUNCTIONING, ACCOUNTABILITY MECHANISM AND FINANCIAL REPORTING ISSUES OF URBAN LOCAL BODIES Introduction 3.1 37 Orgnisational setup of Urban Local Bodies 3.2 37 Functioning of Urban Local Bodies 3.3 39 Formation of various committees 3.4 41 Audit arrangement 3.5 42 Response to Audit Observations 3.6 43 Ombudsman 3.7 44 Social Audit 3.8 44 Submission of Utilisation Certificates 3.12 45 Internal Audit and Internal Control System of Urban Local Bodies 3.13 45 Financial Reporting Issues 3.14 46 CHAPTER – IV PERFORMANCE -
(Scheme I Volume 2) (Transmission Lines Associated with GSS at Panki) Public Disclosure Authorized
Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Environment and Social Impact Assessment Report (Scheme I Volume 2) (Transmission Lines Associated with GSS at Panki) Public Disclosure Authorized Jharkhand Urja Sancharan Nigam Limited Final Report November 2018 www.erm.com The Business of Sustainability FINAL REPORT Jharkhand Urja Sancharan Nigam Limited Environment and Social Impact Assessment Report (Scheme I Volume 2) (Transmission Lines Associated with GSS at Panki) 09 November 2018 Reference # 0402882 Prepared by Suvankar Das Consultant Prepared by Abhishek Roy Goswami Senior Consultant Reviewed & Debanjan Approved by: Bandyapodhyay Partner This report has been prepared by ERM India Private Limited a member of Environmental Resources Management Group of companies, with all reasonable skill, care and diligence within the terms of the Contract with the client, incorporating our General Terms and Conditions of Business and taking account of the resources devoted to it by agreement with the client. We disclaim any responsibility to the client and others in respect of any matters outside the scope of the above. This report is confidential to the client and we accept no responsibility of whatsoever nature to third parties to whom this report, or any part thereof, is made known. Any such party relies on the report at their own risk. TABLE OF CONTENTS EXECUTIVE SUMMARY I 1 INTRODUCTION 1 1.1 BACKGROUND 1 1.2 PROJECT OVERVIEW 1 1.3 PURPOSE AND SCOPE OF THIS ESIA 2 1.4 STRUCTURE OF THE REPORT 2 1.5 LIMITATION -

Chhatarpur (Sc)
ASSEMBLY CONSTITUENCY MAP C H H A T A R P U R ( S C ) - ( 7 8 ) © K 0 2.25 4.5 9 13.5 (79) - Hussainabad Patra Khurd Gamharia Pathra Sandha Assembly Constituency Kailkha Mangara Jhargara Km ThekahiRangnia Ê Dalpatpur Gontha Deogan Pipra Kalan Mahugain Bamhandih Hathgara Kui Urf Shashiganj TilharhwaBhitiha Mahuari Dhobni Erajikita Ê Bergain Dumaria 18 2 1 Lowadag Chatar Chati Ê K Patsara Bansdiha Alias Latea Marar 17 3 Ê KEY MAP Piprahat BhainsraMaheshra Kalapahar Lamba Chunautwa Dhobidih 16 Tendudih 4 5 28 Chuchru Pachmo Bhalubar Bhadwa Kokro 79 15 Pachmo 19 Maradag 30 6 Tardih Pokhraha Bhojua 12 11 Birwadohar Bogna Alias Ahri Karupa Majhganwan KundilKulhia 81 31 Baijna Gosaindih 77 78 27 21 13 10 K BIHAR 14 7 Dinadag 29 Solanga Mednipur Jhardag 75 26 20 Khendhora Khurd Gulabjhari 80 24 32 Chauchhia Lachhmipur 25 33 9 8 Jamalpur Jamua Alias Bishunpur 76 42 Keswahi Alias Tenwahi K Larmi Khendhra Kalan Ê 74 22 Lahanga NawadihÊ Kathautia 34 40 39 Pindrahi Naso Mayapur 43 38 Kushmaha K 23 35 41 Kauwal Ê 73 36 Dundur Kachanpur Ê 65 37 Phatia Kodwaria Ê 72 Bandhudih Rajha Ê Ê Ê Bara Salaiya Bhandardih Jolahkhap 64 63 62 Pahari Ê Ê 69 66 61 Obra Hisag Jobna Alias Ramgarh Ê Ê Harna Pakha Gopalpur Arjundih Guruain K Manandohar 60 Ê Ê 68 Ê Ê Baghamara Ê 67 58 Naudiha Nima Majurahi 50 Obra Shivdayaldih Madanpur Marhipta 59 Kharwardih Marwa Pichhulia Ê 47 Rud Nawdiha Bara 49 Ê K Bagaiya K Madheya 57 48 Ê Ê 8 Ê Chorar Alias Udaigarh a Kauwal 56 K 9 ÊNawatacnr 70 Ê H Ê Ê N Nawadih Risyapa 51 45 Ê Ê Amwa Thekha 46 Belwanr Ê 71 55 Obra Ê Lohrai Ê 52 -
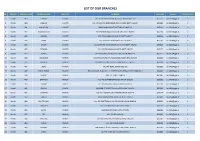
List of Our Branches
LIST OF OUR BRANCHES SR REGION BRANCH CODE BRANCH NAME DISTRICT ADDRESS PIN CODE E-MAIL CONTACT NO 1 Ranchi 419 DORMA KHUNTI VILL+PO-DORMA,VIA-KHUNTI,DISTT-KHUNTI-835 227 835227 [email protected] 0 2 Ranchi 420 JAMHAR KHUNTI VILL-JAMHAR,PO-GOBINDPUR RD,VIA-KARRA DISTT-KHUNTI. 835209 [email protected] 0 3 Ranchi 421 KHUNTI (R) KHUNTI MAIN ROAD,KHUNTI,DISTT-KHUNTI-835 210 835210 [email protected] 0 4 Ranchi 422 MARANGHADA KHUNTI VILL+PO-MARANGHADA,VIA-KHUNTI,DISTT-KHUNTI 835210 [email protected] 0 5 Ranchi 423 MURHU KHUNTI VILL+PO-MURHU,VIA-KHUNTI, DISTT-KHUNTI 835216 [email protected] 0 6 Ranchi 424 SAIKO KHUNTI VILL+PO-SAIKO,VIA-KHUNTI,DISTT-KHUNTI 835210 [email protected] 0 7 Ranchi 425 SINDRI KHUNTI VILL-SINDRI,PO-KOCHASINDRI,VIA-TAMAR,DISTT-KHUNTI 835225 [email protected] 0 8 Ranchi 426 TAPKARA KHUNTI VILL+PO-TAPKARA,VIA-KHUNTI, DISTT-KHUNTI 835227 [email protected] 0 9 Ranchi 427 TORPA KHUNTI VILL+PO-TORPA,VIA-KHUNTI, DISTT-KHUNTI-835 227 835227 [email protected] 0 10 Ranchi 444 BALALONG RANCHI VILL+PO-DAHUTOLI PO-BALALONG,VIA-DHURWA RANCHI 834004 [email protected] 0 11 Ranchi 445 BARIATU RANCHI HOUSING COLONY, BARIATU, RANCHI P.O. - R.M.C.H., 834009 [email protected] 0 12 Ranchi 446 BERO RANCHI VILL+PO-BERO, RANCHI-825 202 825202 [email protected] 0 13 Ranchi 447 BIRSA CHOWK RANCHI HAWAI NAGAR, ROAD NO. - 1, KHUNTI ROAD, BIRSA CHOWK, RANCHI - 3 834003 [email protected] 0 14 Ranchi 448 BOREYA RANCHI BOREYA, KANKE, RANCHI 834006 [email protected] 0 15 Ranchi 449 BRAMBEY RANCHI VILL+PO-BRAMBEY(MANDER),RANCHI-835205 835205 [email protected] 0 16 Ranchi 450 BUNDU -

Jharkhand Annex.H2.Xlsx
Notice for appointment of Regular / Rural Retail Outlet Dealerships Bharat Petroleum Corporation Limited proposes to appoint Retail Outlet dealers in Jharkhand, as per following details: Sl. No Name of location Revenue District Type of RO Estimated Category Type of Site* Minimum Dimension (in M.)/Area of the site (in Finance to be arranged by the Mode of Fixed Fee / Security Deposit monthly Sales Sq. M.). * applicant Selection Minimum Bid (Rs. Lakhs) Potential # (Rs. Lakhs) amount. (Rs. Lakhs) 1 2 3 4 5 6 7 8 9a 9b 10 11 12 Regular / Rural MS+HSD in Kls SC CC / DC / CFS Frontage Depth Area Estimated Estimated fund Draw of Lots / working capital required for Bidding SC CC-1 requirement for development of SC CC-2 operation of RO infrastructure at RO SC PH ST ST CC-1 ST CC-2 ST PH OBC OBC CC-1 OBC CC-2 OBC PH OPEN OPEN CC-1 OPEN CC-2 OPEN PH Between Kargali gate to Chalkari Draw of 1 Basti BOKARO RURAL 113 ST CFS 30 25 750 0 0 Lots 0 2 Between Phusro to Dumri on Dumri- Draw of 2 Bermo Jaina Marg BOKARO RURAL 149 SC CFS 30 25 750 0 0 Lots 0 2 Between Gomoh Railway Crossing to Khario Railway Crossing on Draw of 3 Topchanchi- Nawagarh Road DHANBAD RURAL 148 ST CFS 30 25 750 0 0 Lots 0 2 Draw of 4 Mouza-TANDWA Not ON SH CHATRA RURAL 178 ST CFS 30 25 750 0 0 Lots 0 2 Within 2 km of Kanvatia Chowk on Kothiya more to Dumma Chowk Draw of 5 road DEOGHAR RURAL 90 ST CFS 30 25 750 0 0 Lots 0 2 Between Govt. -

A Regional Assessment of the Potential for Co2 Storage in the Indian Subcontinent
A REGIONAL ASSESSMENT OF THE POTENTIAL FOR CO2 STORAGE IN THE INDIAN SUBCONTINENT Technical Study Report No. 2008/2 May 2008 This document has been prepared for the Executive Committee of the IEA GHG Programme. It is not a publication of the Operating Agent, International Energy Agency or its Secretariat. INTERNATIONAL ENERGY AGENCY The International Energy Agency (IEA) was established in 1974 within the framework of the Organisation for Economic Co-operation and Development (OECD) to implement an international energy programme. The IEA fosters co-operation amongst its 26 member countries and the European Commission, and with the other countries, in order to increase energy security by improved efficiency of energy use, development of alternative energy sources and research, development and demonstration on matters of energy supply and use. This is achieved through a series of collaborative activities, organised under more than 40 Implementing Agreements. These agreements cover more than 200 individual items of research, development and demonstration. The IEA Greenhouse Gas R&D Programme is one of these Implementing Agreements. ACKNOWLEDGEMENTS AND CITATIONS This report was prepared as an account of the work sponsored by the IEA Greenhouse Gas R&D Programme. The views and opinions of the authors expressed herein do not necessarily reflect those of the IEA Greenhouse Gas R&D Programme, its members, the International Energy Agency, the organisations listed below, nor any employee or persons acting on behalf of any of them. In addition, none of these make any warranty, express or implied, assumes any liability or responsibility for the accuracy, completeness or usefulness of any information, apparatus, product of process disclosed or represents that its use would not infringe privately owned rights, including any parties intellectual property rights. -

MANISH Final
DISTRICT SUPERINTENDENT OF EDUCATION, PALAMU foHkkxh; ladYi la[;k 1145 fnukad 18-07-2019 ds vkyksd esa vizf'kf{kr f'k{kdksa dks mudh fu;qfDr frfFk ls ,oa yksd lsok vk;ksx }kjk fu;qDr f'k{kdksa dk e/s kk lwph ls xzsM&1 dh vkilh ojh;rk lwphA Social Sl# Name School Block Gender DOB DOJ in Service Grade 1 Designation Sl.No. In Merit List Address Remarks Category MOHAMMAD MADRASATUL ISLAM KUDAGA Unreserv 1 CHAINPUR (200210) Male 12/05/1962 25/09/1980 25/09/1980 INTER TRAINED PATRATU,SARJU,GARU, LATEHAR JAMALUDIN KALAN ed NEZMUDDIN AHAMAD MADRASATUL ISLAM KUDAGA Unreserv 2 CHAINPUR (200210) Male 03/02/1962 01/10/1980 01/10/1980 INTER TRAINED SHAHPUR, CHAINPUR, PALAMU ANSARI KALAN ed MADRASATUL ISLAM KUDAGA Unreserv 3 MD FASIHUDDIN CHAINPUR (200210) Male 04/04/1964 01/06/1982 01/06/1982 INTER TRAINED SHAHPUR, CHAINPUR, PALAMU KALAN ed PRAMOD KUMAR BISHRAMPUR Unreserv 4 UPG RAJKIYEKRIT MS TONA Male 01/01/1963 21/08/1982 21/08/1982 INTER TRAINED DUBEY (200209) ed Unreserv 5 AMAR NATH JHA KALI SANSKRIT MS KISHUNPUR PATAN (200212) Male 05/06/1964 29/08/1982 29/08/1982 INTER TRAINED ed DALTONGANJ Unreserv 6 AHMAD HUSSAIN MADARSA AHSANUL ULOOM Male 23/04/1964 01/04/1983 01/04/1983 INTER TRAINED kund mohallah near millat masjid (200201) ed MD REYAZUDDIN MADRASATUL ISLAM KUDAGA Unreserv 7 CHAINPUR (200210) Male 12/11/1963 02/01/1984 02/01/1984 INTER TRAINED SUNTHA, PANDEYPURA, PATAN, PALAMU ANSARI KALAN ed UPG RAJKIYEKRIT MS MANJHI Unreserv VILL- MAJHIGAWAN, P. -

PALAMAU Name of the Lead Bank: STATE BANK of INDIA
List of villages with population below 2000 alloted to banks for FI Name of the District :: PALAMAU Name of the Lead Bank: STATE BANK OF INDIA Population of the village as Sl. Name of village with population Name of Bank , allotted per (2001 no Name of Block Name of Panchayat below 2000 the village census) 1 2 7 5 1 HARIHARGANJ KULHIYA KULHIYA VGB DHAB 920 HARIHARGANJ KULHIYA SHIKAR PUR VGB DHAB 558 HARIHARGANJ KULHIYA KARI LEBDA VGB DHAB 40 HARIHARGANJ KULHIYA LADI BADI VGB DHAB 592 HARIHARGANJ KULHIYA KOTHILA VGB DHAB 735 HARIHARGANJ KULHIYA NAUDIHA KALA VGB DHAB 126 HARIHARGANJ KULHIYA JAGDISHPUR VGB DHAB 635 HARIHARGANJ KULHIYA DIGLA VGB DHAB 9 HARIHARGANJ KULHIYA KOLHUWADA VGB DHAB 585 HARIHARGANJ KULHIYA JAHANA VGB DHAB 354 HARIHARGANJ KULHIYA NATHA VGB DHAB 50 HARIHARGANJ KULHIYA HARNIYA KHURD VGB DHAB 4 HARIHARGANJ SEMERWAR SEMERWAR VGB DHAB 1515 HARIHARGANJ SEMERWAR BHANDAR VGB DHAB 21 HARIHARGANJ SEMERWAR BIJWAR VGB DHAB 314 HARIHARGANJ SEMERWAR RAJWAR VGB DHAB 153 HARIHARGANJ SEMERWAR THARGHAT VGB DHAB 9 HARIHARGANJ SEMERWAR DHABKALA VGB DHAB 1398 HARIHARGANJ SEMERWAR DHABA KHURD VGB DHAB 168 HARIHARGANJ SEMERWAR MAMERKHA VGB DHAB 195 HARIHARGANJ SEMERWAR KAUWAKHOH VGB DHAB 478 HARIHARGANJ SEMERWAR PIRAUJEE VGB DHAB 448 HARIHARGANJ SEMERWAR TARACHAK VGB DHAB 110 HARIHARGANJ SEMERWAR CHANDA VGB DHAB 151 HARIHARGANJ SEMERWAR BIJNIWAR URF LAKHNI VGB DHAB 526 HARIHARGANJ KATAIYA KUSHDIH VGB DHAB 546 HARIHARGANJ KATAIYA TENUWA KALA VGB HARIHARGANJ 819 HARIHARGANJ KATAIYA JAGDISHPUR/ RAMPUR VGB HARIHARGANJ 389 HARIHARGANJ KATAIYA -

Draft Esia Scheme N Vol 2 Chhatarpur Tl
Environment and Social Impact Assessment Report (Scheme N Volume 2) (Transmission Lines Associated with GSS at Chhatarpur) Jharkhand Urja Sancharan Nigam Limited Final Report January 2019 www.erm.com The Business of Sustainability FINAL REPORT Jharkhand Urja Sancharan Nigam Limited Environment and Social Impact Assessment Report (Scheme N Volume 2) (Transmission Lines Associated with GSS at Chhatarpur) 10 January 2019 Reference # 0402882 Suvankar Das Consultant Prepared by Abhishek Roy Goswami Senior Consultant Reviewed & Debanjan Approved by: Bandyapodhyay Partner This report has been prepared by ERM India Private Limited a member of Environmental Resources Management Group of companies, with all reasonable skill, care and diligence within the terms of the Contract with the client, incorporating our General Terms and Conditions of Business and taking account of the resources devoted to it by agreement with the client. We disclaim any responsibility to the client and others in respect of any matters outside the scope of the above. This report is confidential to the client and we accept no responsibility of whatsoever nature to third parties to whom this report, or any part thereof, is made known. Any such party relies on the report at their own risk. TABLE OF CONTENTS EXECUTIVE SUMMARY I 1 INTRODUCTION 1 1.1 BACKGROUND 1 1.2 PROJECT OVERVIEW 1 1.3 PURPOSE AND SCOPE OF THIS ESIA 2 1.4 STRUCTURE OF THE REPORT 2 1.5 LIMITATION 3 1.6 USES OF THIS REPORT 3 2 POLICY, LEGAL AND ADMINISTRATIVE FRAME WORK 5 2.1 APPLICABLE LAWS AND STANDARDS 5 -

A. Title: Quality Seeds No Longer a Dream
SS -I ATMA, PALAMAU A. Title: Quality seeds no longer a dream B. Background: Come the Rabi season, and the majority of farmers in the western district of Palamu take to wheat cultivation. The reason that drives the move is consumption — both by humans and animals. But ever since Jharkhand was carved out of Bihar, there has been a problem with regard to the supply of quality seeds. The State has been relying heavily on outside assistance to meet its quota for the same. This, however, has begotten fresh problems instead of offering solutions to meet the scarcity. Most of the time seeds aren’t delivered on time, and when they do arrive they are not quite of the desired standards vis-à-vis the new micro-farming situation prevalent in the State. The Department of Agriculture has its hand on the pulse of this problem and is trying to promote the concept of ‘seed villages’, wherein farmers are encouraged to grow seeds themselves instead of banking on somebody else’s mercy. C. Intervention and process: Presently, ZRS, Chianki, is the only research station in the district that produces quality seeds of wheat. But that has not been enough to cater to the growing demands of the farming community. To bridge the gap between the burgeoning demand and scarce supply of quality seeds, ATMA, Palamu in association with KVK, Chianki convened a meeting of all Food Advisory Committee chairmen, District Agriculture Officers and two progressive wheat farmers. Two wheat growers, who were economically sound and had a feel for technology, were picked.