Harnessing the Anti-Cancer Natural Product Nimbolide for Targeted
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Small Cell Ovarian Carcinoma: Genomic Stability and Responsiveness to Therapeutics
Gamwell et al. Orphanet Journal of Rare Diseases 2013, 8:33 http://www.ojrd.com/content/8/1/33 RESEARCH Open Access Small cell ovarian carcinoma: genomic stability and responsiveness to therapeutics Lisa F Gamwell1,2, Karen Gambaro3, Maria Merziotis2, Colleen Crane2, Suzanna L Arcand4, Valerie Bourada1,2, Christopher Davis2, Jeremy A Squire6, David G Huntsman7,8, Patricia N Tonin3,4,5 and Barbara C Vanderhyden1,2* Abstract Background: The biology of small cell ovarian carcinoma of the hypercalcemic type (SCCOHT), which is a rare and aggressive form of ovarian cancer, is poorly understood. Tumourigenicity, in vitro growth characteristics, genetic and genomic anomalies, and sensitivity to standard and novel chemotherapeutic treatments were investigated in the unique SCCOHT cell line, BIN-67, to provide further insight in the biology of this rare type of ovarian cancer. Method: The tumourigenic potential of BIN-67 cells was determined and the tumours formed in a xenograft model was compared to human SCCOHT. DNA sequencing, spectral karyotyping and high density SNP array analysis was performed. The sensitivity of the BIN-67 cells to standard chemotherapeutic agents and to vesicular stomatitis virus (VSV) and the JX-594 vaccinia virus was tested. Results: BIN-67 cells were capable of forming spheroids in hanging drop cultures. When xenografted into immunodeficient mice, BIN-67 cells developed into tumours that reflected the hypercalcemia and histology of human SCCOHT, notably intense expression of WT-1 and vimentin, and lack of expression of inhibin. Somatic mutations in TP53 and the most common activating mutations in KRAS and BRAF were not found in BIN-67 cells by DNA sequencing. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
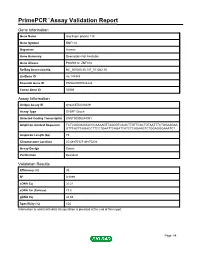
Primepcr™Assay Validation Report
PrimePCR™Assay Validation Report Gene Information Gene Name ring finger protein 114 Gene Symbol RNF114 Organism Human Gene Summary Description Not Available Gene Aliases PSORS12, ZNF313 RefSeq Accession No. NC_000020.10, NT_011362.10 UniGene ID Hs.144949 Ensembl Gene ID ENSG00000124226 Entrez Gene ID 55905 Assay Information Unique Assay ID qHsaCED0044029 Assay Type SYBR® Green Detected Coding Transcript(s) ENST00000244061 Amplicon Context Sequence TCTCGGGAGGACCCAAAAGTTAAGGTCAGCTTGTTCACTGTAATTTCTGGAAGAA GTTCACTCAGACCTTCCTGAATTCAGATCATCTCAGAAGTCTGGAGGGAAATCT Amplicon Length (bp) 79 Chromosome Location 20:48570127-48570235 Assay Design Exonic Purification Desalted Validation Results Efficiency (%) 95 R2 0.9999 cDNA Cq 20.21 cDNA Tm (Celsius) 78.5 gDNA Cq 24.64 Specificity (%) 100 Information to assist with data interpretation is provided at the end of this report. Page 1/4 PrimePCR™Assay Validation Report RNF114, Human Amplification Plot Amplification of cDNA generated from 25 ng of universal reference RNA Melt Peak Melt curve analysis of above amplification Standard Curve Standard curve generated using 20 million copies of template diluted 10-fold to 20 copies Page 2/4 PrimePCR™Assay Validation Report Products used to generate validation data Real-Time PCR Instrument CFX384 Real-Time PCR Detection System Reverse Transcription Reagent iScript™ Advanced cDNA Synthesis Kit for RT-qPCR Real-Time PCR Supermix SsoAdvanced™ SYBR® Green Supermix Experimental Sample qPCR Human Reference Total RNA Data Interpretation Unique Assay ID This is a unique identifier that can be used to identify the assay in the literature and online. Detected Coding Transcript(s) This is a list of the Ensembl transcript ID(s) that this assay will detect. Details for each transcript can be found on the Ensembl website at www.ensembl.org. -

Genetics of Amyotrophic Lateral Sclerosis in the Han Chinese
Genetics of amyotrophic lateral sclerosis in the Han Chinese Ji He A thesis submitted for the degree of Master of Philosophy at The University of Queensland in 2015 The University of Queensland Diamantina Institute 1 Abstract Amyotrophic lateral sclerosis is the most frequently occurring neuromuscular degenerative disorders, and has an obscure aetiology. Whilst major progress has been made, the majority of the genetic variation involved in ALS is, as yet, undefined. In this thesis, multiple genetic studies have been conducted to advance our understanding of the genetic architecture of the disease. In the light of the paucity of comprehensive genetic studies performed in Chinese, the presented study focused on advancing our current understanding in genetics of ALS in the Han Chinese population. To identify genetic variants altering risk of ALS, a genome-wide association study (GWAS) was performed. The study included 1,324 Chinese ALS cases and 3,115 controls. After quality control, a number of analyses were performed in a cleaned dataset of 1,243 cases and 2,854 controls that included: a genome-wide association analysis to identify SNPs associated with ALS; a genomic restricted maximum likelihood (GREML) analysis to estimate the proportion of the phenotypic variance in ALS liability due to common SNPs; and a gene- based analysis to identify genes associated with ALS. There were no genome-wide significant SNPs or genes associated with ALS. However, it was estimated that 17% (SE: 0.05; P=6×10-5) of the phenotypic variance in ALS liability was due to common SNPs. The top associated SNP was within GNAS (rs4812037; p =7×10-7). -

Genomic Approach in Idiopathic Intellectual Disability Maria De Fátima E Costa Torres
ESTUDOS DE 8 01 PDPGM 2 CICLO Genomic approach in idiopathic intellectual disability Maria de Fátima e Costa Torres D Autor. Maria de Fátima e Costa Torres D.ICBAS 2018 Genomic approach in idiopathic intellectual disability Genomic approach in idiopathic intellectual disability Maria de Fátima e Costa Torres SEDE ADMINISTRATIVA INSTITUTO DE CIÊNCIAS BIOMÉDICAS ABEL SALAZAR FACULDADE DE MEDICINA MARIA DE FÁTIMA E COSTA TORRES GENOMIC APPROACH IN IDIOPATHIC INTELLECTUAL DISABILITY Tese de Candidatura ao grau de Doutor em Patologia e Genética Molecular, submetida ao Instituto de Ciências Biomédicas Abel Salazar da Universidade do Porto Orientadora – Doutora Patrícia Espinheira de Sá Maciel Categoria – Professora Associada Afiliação – Escola de Medicina e Ciências da Saúde da Universidade do Minho Coorientadora – Doutora Maria da Purificação Valenzuela Sampaio Tavares Categoria – Professora Catedrática Afiliação – Faculdade de Medicina Dentária da Universidade do Porto Coorientadora – Doutora Filipa Abreu Gomes de Carvalho Categoria – Professora Auxiliar com Agregação Afiliação – Faculdade de Medicina da Universidade do Porto DECLARAÇÃO Dissertação/Tese Identificação do autor Nome completo _Maria de Fátima e Costa Torres_ N.º de identificação civil _07718822 N.º de estudante __ 198600524___ Email institucional [email protected] OU: [email protected] _ Email alternativo [email protected] _ Tlf/Tlm _918197020_ Ciclo de estudos (Mestrado/Doutoramento) _Patologia e Genética Molecular__ Faculdade/Instituto _Instituto de Ciências -

Genome-Wide Pooling Approach Identifies SPATA5 As A
European Journal of Human Genetics (2012) 20, 326–332 & 2012 Macmillan Publishers Limited All rights reserved 1018-4813/12 www.nature.com/ejhg ARTICLE Genome-wide pooling approach identifies SPATA5 as a new susceptibility locus for alopecia areata Lina M Forstbauer1,20, Felix F Brockschmidt1,2,20, Valentina Moskvina3, Christine Herold4, Silke Redler1, Alexandra Herzog1, Axel M Hillmer5, Christian Meesters4,6, Stefanie Heilmann1,2, Florian Albert1, Margrieta Alblas1,2, Sandra Hanneken7, Sibylle Eigelshoven7, Kathrin A Giehl8, Dagny Jagielska1,9, Ulrike Blume-Peytavi9, Natalie Garcia Bartels9, Jennifer Kuhn10,11,12, Hans Christian Hennies10,11,12, Matthias Goebeler13, Andreas Jung13, Wiebke K Peitsch14, Anne-Katrin Kortu¨m15, Ingrid Moll15, Roland Kruse16, Gerhard Lutz17, Hans Wolff7, Bettina Blaumeiser18, Markus Bo¨hm19, George Kirov3, Tim Becker4,6, Markus M No¨then1,2 and Regina C Betz*,1 Alopecia areata (AA) is a common hair loss disorder, which is thought to be a tissue-specific autoimmune disease. Previous research has identified a few AA susceptibility genes, most of which are implicated in autoimmunity. To identify new genetic variants and further elucidate the genetic basis of AA, we performed a genome-wide association study using the strategy of pooled DNA genotyping (729 cases, 656 controls). The strongest association was for variants in the HLA region, which confirms the validity of the pooling strategy. The selected top 61 single-nucleotide polymorphisms (SNPs) were analyzed in an independent replication sample (454 cases, 1364 controls). Only one SNP outside of the HLA region (rs304650) showed significant association. This SNP was then analyzed in a second independent replication sample (537 cases, 657 controls). -

The Ubl-UBA Ubiquilin4 Protein Functions As a Tumor Suppressor in Gastric Cancer by P53-Dependent and P53-Independent Regulation of P21
Cell Death & Differentiation https://doi.org/10.1038/s41418-018-0141-4 ARTICLE The UbL-UBA Ubiquilin4 protein functions as a tumor suppressor in gastric cancer by p53-dependent and p53-independent regulation of p21 1,2,3 1,2,4 5 1,2,4 6 7,8,9 10 1,2,4 Shengkai Huang ● Yan Li ● Xinghua Yuan ● Mei Zhao ● Jia Wang ● You Li ● Yuan Li ● Hong Lin ● 1,2,4 1,2,4 1,2,4 3 11 7 12 Qiao Zhang ● Wenjie Wang ● Dongdong Li ● Xin Dong ● Lanfen Li ● Min Liu ● Weiyan Huang ● Changzhi Huang1,2,4 Received: 28 November 2017 / Revised: 21 May 2018 / Accepted: 23 May 2018 © The Author(s) 2018. This article is published with open access Abstract Ubiquilin4 (Ubqln4), a member of the UbL-UBA protein family, serves as an adaptor in the degradation of specific substrates via the proteasomal pathway. However, the biological function of Ubqln4 remains largely unknown, especially in cancer. Here, we reported that Ubqln4 was downregulated in gastric cancer tissues and functioned as a tumor suppressor by inhibiting gastric cancer cell proliferation in vivo and in vitro. Overexpression of Ubqln4-induced cellular senescence 1234567890();,: 1234567890();,: and G1-S cell cycle arrest in gastric cancer cells and activated the p53/p21 axis. Moreover, Ubqln4 regulated p21 through both p53-dependent and p53-independent manners. Ubqln4 interacted with RNF114, an E3 ubiquitin ligase of p21, and negatively regulated its expression level, which in turn stabilized p21 by attenuating proteasomal degradation of p21. These effects of Ubqln4 were partly abrogated in gastric cancer cells upon silencing of p21. -

Content Based Search in Gene Expression Databases and a Meta-Analysis of Host Responses to Infection
Content Based Search in Gene Expression Databases and a Meta-analysis of Host Responses to Infection A Thesis Submitted to the Faculty of Drexel University by Francis X. Bell in partial fulfillment of the requirements for the degree of Doctor of Philosophy November 2015 c Copyright 2015 Francis X. Bell. All Rights Reserved. ii Acknowledgments I would like to acknowledge and thank my advisor, Dr. Ahmet Sacan. Without his advice, support, and patience I would not have been able to accomplish all that I have. I would also like to thank my committee members and the Biomed Faculty that have guided me. I would like to give a special thanks for the members of the bioinformatics lab, in particular the members of the Sacan lab: Rehman Qureshi, Daisy Heng Yang, April Chunyu Zhao, and Yiqian Zhou. Thank you for creating a pleasant and friendly environment in the lab. I give the members of my family my sincerest gratitude for all that they have done for me. I cannot begin to repay my parents for their sacrifices. I am eternally grateful for everything they have done. The support of my sisters and their encouragement gave me the strength to persevere to the end. iii Table of Contents LIST OF TABLES.......................................................................... vii LIST OF FIGURES ........................................................................ xiv ABSTRACT ................................................................................ xvii 1. A BRIEF INTRODUCTION TO GENE EXPRESSION............................. 1 1.1 Central Dogma of Molecular Biology........................................... 1 1.1.1 Basic Transfers .......................................................... 1 1.1.2 Uncommon Transfers ................................................... 3 1.2 Gene Expression ................................................................. 4 1.2.1 Estimating Gene Expression ............................................ 4 1.2.2 DNA Microarrays ...................................................... -

Supplementary Table 1 Double Treatment Vs Single Treatment
Supplementary table 1 Double treatment vs single treatment Probe ID Symbol Gene name P value Fold change TC0500007292.hg.1 NIM1K NIM1 serine/threonine protein kinase 1.05E-04 5.02 HTA2-neg-47424007_st NA NA 3.44E-03 4.11 HTA2-pos-3475282_st NA NA 3.30E-03 3.24 TC0X00007013.hg.1 MPC1L mitochondrial pyruvate carrier 1-like 5.22E-03 3.21 TC0200010447.hg.1 CASP8 caspase 8, apoptosis-related cysteine peptidase 3.54E-03 2.46 TC0400008390.hg.1 LRIT3 leucine-rich repeat, immunoglobulin-like and transmembrane domains 3 1.86E-03 2.41 TC1700011905.hg.1 DNAH17 dynein, axonemal, heavy chain 17 1.81E-04 2.40 TC0600012064.hg.1 GCM1 glial cells missing homolog 1 (Drosophila) 2.81E-03 2.39 TC0100015789.hg.1 POGZ Transcript Identified by AceView, Entrez Gene ID(s) 23126 3.64E-04 2.38 TC1300010039.hg.1 NEK5 NIMA-related kinase 5 3.39E-03 2.36 TC0900008222.hg.1 STX17 syntaxin 17 1.08E-03 2.29 TC1700012355.hg.1 KRBA2 KRAB-A domain containing 2 5.98E-03 2.28 HTA2-neg-47424044_st NA NA 5.94E-03 2.24 HTA2-neg-47424360_st NA NA 2.12E-03 2.22 TC0800010802.hg.1 C8orf89 chromosome 8 open reading frame 89 6.51E-04 2.20 TC1500010745.hg.1 POLR2M polymerase (RNA) II (DNA directed) polypeptide M 5.19E-03 2.20 TC1500007409.hg.1 GCNT3 glucosaminyl (N-acetyl) transferase 3, mucin type 6.48E-03 2.17 TC2200007132.hg.1 RFPL3 ret finger protein-like 3 5.91E-05 2.17 HTA2-neg-47424024_st NA NA 2.45E-03 2.16 TC0200010474.hg.1 KIAA2012 KIAA2012 5.20E-03 2.16 TC1100007216.hg.1 PRRG4 proline rich Gla (G-carboxyglutamic acid) 4 (transmembrane) 7.43E-03 2.15 TC0400012977.hg.1 SH3D19 -

Vast Human-Specific Delay in Cortical Ontogenesis Associated With
Supplementary information Extension of cortical synaptic development distinguishes humans from chimpanzees and macaques Supplementary Methods Sample collection We used prefrontal cortex (PFC) and cerebellar cortex (CBC) samples from postmortem brains of 33 human (aged 0-98 years), 14 chimpanzee (aged 0-44 years) and 44 rhesus macaque individuals (aged 0-28 years) (Table S1). Human samples were obtained from the NICHD Brain and Tissue Bank for Developmental Disorders at the University of Maryland, USA, the Netherlands Brain Bank, Amsterdam, Netherlands and the Chinese Brain Bank Center, Wuhan, China. Informed consent for use of human tissues for research was obtained in writing from all donors or their next of kin. All subjects were defined as normal by forensic pathologists at the corresponding brain bank. All subjects suffered sudden death with no prolonged agonal state. Chimpanzee samples were obtained from the Yerkes Primate Center, GA, USA, the Anthropological Institute & Museum of the University of Zürich-Irchel, Switzerland and the Biomedical Primate Research Centre, Netherlands (eight Western chimpanzees, one Central/Eastern and five of unknown origin). Rhesus macaque samples were obtained from the Suzhou Experimental Animal Center, China. All non-human primates used in this study suffered sudden deaths for reasons other than their participation in this study and without any relation to the tissue used. CBC dissections were made from the cerebellar cortex. PFC dissections were made from the frontal part of the superior frontal gyrus. All samples contained an approximately 2:1 grey matter to white matter volume ratio. RNA microarray hybridization RNA isolation, hybridization to microarrays, and data preprocessing were performed as described previously (Khaitovich et al. -

Single Nucleotide Polymorphism and Haplotype Effects Associated With
Single nucleotide polymorphism and haplotype effects associated with somatic cell score in German Holstein cattle Hamdy Abdel-Shafy, Ralf H Bortfeldt, Jens Tetens, Gudrun A Brockmann To cite this version: Hamdy Abdel-Shafy, Ralf H Bortfeldt, Jens Tetens, Gudrun A Brockmann. Single nucleotide poly- morphism and haplotype effects associated with somatic cell score in German Holstein cattle. Genetics Selection Evolution, 2014, 46 (1), pp.35. 10.1186/1297-9686-46-35. hal-01341264 HAL Id: hal-01341264 https://hal.archives-ouvertes.fr/hal-01341264 Submitted on 4 Jul 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. et al. Genetics Selection Evolution Abdel-Shafy 2014, 46:35 Genetics http://www.gsejournal.org/content/46/1/35 Selection Evolution RESEARCH Open Access Single nucleotide polymorphism and haplotype effects associated with somatic cell score in German Holstein cattle Hamdy Abdel-Shafy1,2, Ralf H Bortfeldt1, Jens Tetens3 and Gudrun A Brockmann1* Abstract Background: To better understand the genetic determination of udder health, we performed a genome-wide association study (GWAS) on a population of 2354 German Holstein bulls for which daughter yield deviations (DYD) for somatic cell score (SCS) were available. -

Cross-Species Alcohol Dependence-Associated Gene Networks: Co-Analysis Of
bioRxiv preprint doi: https://doi.org/10.1101/380584; this version posted July 30, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 1 Cross-species alcohol dependence-associated gene networks: Co-analysis of 2 mouse brain gene expression and human genome-wide association data 3 4 Short Title: Cross-species analysis reveals alcohol dependence-associated gene networks 5 6 Kristin M. Mignogna2,3,4, Silviu A. Bacanu2,3, Brien P. Riley2,3, Aaron R. Wolen5, Michael F. 7 Miles1,3* 8 9 1 Department of Pharmacology and Toxicology, Virginia Commonwealth University, Richmond, 10 Virginia, United States of America 11 2 Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, 12 Richmond, Virginia, United States of America 13 3 VCU Alcohol Research Center, Virginia Commonwealth University, Richmond, Virginia, 14 United States of America 15 4 VCU Center for Clinical & Translational Research, Virginia Commonwealth University, 16 Richmond, Virginia, United States of America 17 5Department of Human and Molecular Genetics, Virginia Commonwealth University, Richmond, 18 Virginia, United States of America 19 20 * Corresponding author 21 E-mail: [email protected] bioRxiv preprint doi: https://doi.org/10.1101/380584; this version posted July 30, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license.