Department of Urology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
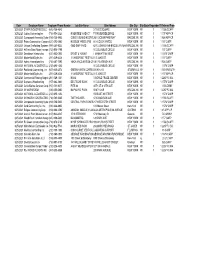
Date Employer Name Employer Phone Numbe Job Site Name Site Address Site City Site State Requmber Filreferred from 3/25/2021 STAR
Date Employer Name Employer Phone Numbe Job Site Name Site Address Site City Site State Requmber FilReferred From 3/25/2021 STARR INDUSTRIES LLC (646) 756-4648 3 TIMES SQUARE NEW YORK NY 1 1 1556 SCAFF 3/25/2021 Judlau Contracting Inc (718) 554-2320 RIVERSIDE VIADUCT 715 RIVERSIDE DRIVE NEW YORK NY 1 1 157 APP-CP 3/25/2021 Component Assembly Syste (914) 738-5400 CONEY ISLAND HOSPIT 2601 OCEAN PARKWAY BROOKLYN NY 1 1 926 APP-CP 3/25/2021 Pabco Construction Corpora (631) 293-6860 HUDSON YARDS (PM) 50 HUDSON YARDS NEW YORK NY 1 1 157 CARP 3/25/2021 Unique Scaffolding Systems (908) 241-9322 GMD SHIP YARD 63 FLUSHING AVE-BROOKLYN NAVYBROOKLYN NY 1 1 1556 SCAFF 3/25/2021 Hi Tech Data Floors Incorpor(732) 905-1799 10 COLUMBUS CIRCLE NEW YORK NY 157 CARP 3/25/2021 Donaldson Interiors Inc. (631) 952-0800 ERNST & YOUNG 1 MANHATTAN WEST NEW YORK NY 1 1 157W CARP 3/25/2021 Modernfold/Styles Inc (201) 329-6226 1 VANDERBILT RESTAU 51 E 42ND ST NEW YORK NY 1 1 157 CARP 3/25/2021 Ashnu International Inc. (718) 267-7590 YMCA VACCINATION CE1401 FLATBUSH AVE BROOKLYN NY 1 1 926 CARP 3/25/2021 NATIONAL ACOUSTICS LLC(212) 695-1252 10 COLUMBUS CIRCLE NEW YORK NY 157W CARP 3/25/2021 Poolbrook Contracting, Inc (607) 435-3578 GREEN HAVEN CORREC594 NY-216 STORMVILLENY 1 1 740 MWDUTH 3/25/2021 Modernfold/Styles Inc (201) 329-6226 1 VANDERBILT RESTAU 51 E 42ND ST NEW YORK NY 1 1 157 APP-CP 3/25/2021 Commercial Flooring Mngmt (201) 729-1331 HANA 3 WORLD TRADE CENTER NEW YORK NY 1 1 2287 FC MA 3/25/2021 Supreme Woodworking (917) 882-4860 DEUTSCHE BANK 10 COLUMBUS -

The Urology Residency Program of the Icahn School of Medicine at Mount Sinai
THE UROLOGY RESIDENCY PROGRAM OF THE ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI Overview The Icahn School of Medicine at Mount Sinai Urology Residency Program is an ACGME-accredited program with a training format consisting of one year of preliminary training in general surgery followed by four years of urology. Its home institution is The Mount Sinai Hospital in New York City. The program is currently approved for a complement of five residents per training year. The program curriculum assures that over the course of training, every resident receives ample experience and didactic grounding in all of the core domains and techniques of urology while acquiring the professional skills and competencies that are characteristic of excellent physicians. Each of the rotations that comprise the curriculum include experience in both in-patient and out- patient treatment settings, with selected rotations offering concentrated experience in areas such as pediatric urology, urodynamics, endourology, female urology, infertility and oncology. An overarching schedule of conferences (led by faculty, fellow residents and guest lecturers), collaborative research projects and support for participation in professional organizations and special programs knit the residents’ clinical experience into the fabric of current urologic scholarship. Our home and affiliated institutions offer an immersive experience in three distinct health care delivery models: the tertiary care academic medical center, the community hospital and the municipal hospital system. Our graduates finish the program with an enviable understanding of the options that are open to them, and well equipped to pursue the urology careers of their choosing. Home and Affiliated Institutions The Mount Sinai Health System consists of seven hospital campuses, each of them a venerable New York institution, located in Manhattan, Brooklyn and Queens. -

2020-2021 Neurology Training at the Mount Sinai Hospital
2020-2021 Neurology Training at The Mount Sinai Hospital “The moment I stepped into the sun and tree-filled atrium of Mount Sinai Hospital, I knew I wanted to train here. The architectural thoughtfulness provides a respite for patients, families, and staff. In a similar way, the importance of emotional well-being is recognized by our program leaders. While residency is inherently challenging, our faculty cultivate a culture of support. During my Mount Sinai interview dinner, I remember overhearing several residents offer to cover an overnight shift for another resident so she could attend a family wedding. The kindness of my fellow residents and the beauty of our hospital inspire me every day.” – Bridget Mueller, Class of 2019 Contacts Barbara Vickrey, MD, MPH System Chair, Department of Neurology [email protected] Aaron Miller, MD Vice Chair for Education, Department of Neurology [email protected] Michelle Fabian, MD Residency Program Director [email protected] Laura K. Stein, MD, MPH Residency Program Associate Director [email protected] Faye Francisco Education Program Manager, Department of Neurology [email protected] 212-241-7074 Follow us on Twitter: @MSHSNeurology 2020-2021 Neurology Training at The Mount Sinai Hospital “I loved how just within the first 2 weeks of starting PGY 2, I felt as though I was already a part of the Mount Sinai Neurology family. Everyone I met has been so collegial, open, and friendly. Whether it was sharing stories during morning report or bonding while responding to stroke codes in the middle of the night, I couldn’t imagine a better start working with my co-residents and mentors.” - Kenneth Leung, Class of 2020 Contents Message from the Residency Program Directors 2 Welcome from the Chair and Vice Chair of Education 4 Department of Neurology 6 Our Commitment to Diversity and Inclusion 7 Neurology Divisions and Centers 8 Corinne Goldsmith Dickinson (CGD) Center for Multiple Sclerosis 8 Vascular Neurology Division 9 Robert and John M. -

View Our Pediatric ENT Brochure
Claremont Pky e e v v A A y r w e H e t t m n s a o r r Theb Bronx G e e th J 9 L E 16 S W t e v d r A a m w a d d E St r E 167th e t s m A r D e e s W 1 r d 65th u i St s o r c e n v i o R C t t S e E 161s v d A n d a W 158th St e E r e R t 161st S s v G r o r A l e e y v s i p W 155th St n M R x n E A y r a t e S w n d k d a c R o u r r r t B e B E 149th S v i t R S r o r i d Mount Sinai Health System r v D E e Ce l e nt r ral B Ce W 145th St t v lv n e d B tr al x A B lvd v i E n d R r e e 3 v g m r A e e l r s i B a l l H E 138 i th St W e v W 135th St E 135th St A e g e r d v v n B A A a e r h e v t Bruckner Blvd G d A 7 a d N r s i 3 e l v a A e P v d a A o x r W o B 125th St E 125th St Ed n gewate y r A e v k e L P n o s d d R u Ed gew r H at er R y d e y a v r i w n R d e 6 B a r H o o W 116th St E 116th St a r d B A r v D d e R S R e D i F h d c R a W 110th St e airv i r v F n e e A w o e v d o A i v a v R M A o e r B m E 106th St R a d o r be e r t t F s D Ke itmar m n s ne Blvd A d y B rg a Blvd N stori W 97th St 97th St A Hoy E 96th St t Ave W S W 96th St B d ro v o l Blvd k B ria ly Asto n y E 92nd St Q d u e e n e e 1 n v n s e A t E K S d x f W p e n y y J v 2 y a k S W r th t A k 85 W 86th St w t a P e n S l y P i l n t a l e e t o s a E 84th St w n r r s 1 S e d t d n d D 3 v n R a o u A e o T r R H r C e W 81st S h D t t B y v F i r Visit/Contact Us 5 Broadway n R e W 79th St 79th St E 79th St Ave 1st t H S r t e D s v 1 e A 2 E d e i k v r d s A r t v a l l e d e P v B v lv e Mount Sinai Doctors i B os y R n o 1 d W -

Bankruptcy Forms
12-13021 Doc 1 Filed 07/11/12 Entered 07/11/12 15:28:08 Main Document Pg B1 (Official Form 1)(12/11) 1 of 32 United States Bankruptcy Court Southern District of New York Voluntary Petition }bk1{Form 1.VoluntaryPetition}bk{ Name of Debtor (if individual, enter Last, First, Middle): Name of Joint Debtor (Spouse) (Last, First, Middle): 305 Church Leasehold Inc. All Other Names used by the Debtor in the last 8 years All Other Names used by the Joint Debtor in the last 8 years (include married, maiden, and trade names): (include married, maiden, and trade names): Last four digits of Soc. Sec. or Individual-Taxpayer I.D. (ITIN) No./Complete EIN Last four digits of Soc. Sec. or Individual-Taxpayer I.D. (ITIN) No./Complete EIN (if more than one, state all) (if more than one, state all) 27-0620672 Street Address of Debtor (No. and Street, City, and State): Street Address of Joint Debtor (No. and Street, City, and State): 305 Church Street New York, NY ZIP Code ZIP Code 10013 County of Residence or of the Principal Place of Business: County of Residence or of the Principal Place of Business: New York Mailing Address of Debtor (if different from street address): Mailing Address of Joint Debtor (if different from street address): ZIP Code ZIP Code Location of Principal Assets of Business Debtor (if different from street address above): Type of Debtor Nature of Business Chapter of Bankruptcy Code Under Which (Form of Organization) (Check one box) (Check one box) the Petition is Filed (Check one box) Individual (includes Joint Debtors) Health Care Business Chapter 7 See Exhibit D on page 2 of this form. -

Download the 2019 Map & Guide
ARCHITECTURAL AND CULTURAL Map &Guide FRIENDS of the Upper East Side Historic Districts Architectural and Cultural Map and Guide Founded in 1982, FRIENDS of the Upper East Side Historic Districts is an independent, not-for-profit membership organization dedicated to preserving the architectural legacy, livability, and sense of place of the Upper East Side by monitoring and protecting its seven Historic Districts, 131 Individual Landmarks, and myriad significant buildings. Walk with FRIENDS as we tour some of the cultural and architectural sites that make the Upper East Side such a distinctive place. From elegant apartment houses and mansions to more modest brownstones and early 20th-century immigrant communities, the Upper East Side boasts a rich history and a wonderfully varied built legacy. With this guide in hand, immerse yourself in the history and architecture of this special corner of New York City. We hope you become just as enchanted by it as we are. FRIENDS’ illustrated Architectural and Cultural Map and Guide includes a full listing of all of the Upper East Side’s 131 Individual Landmarks. You can find the location of these architectural gems by going to the map on pages 2-3 of the guide and referring to the numbered green squares. In the second section of the guide, we will take you through the history and development of the Upper East Side’s seven Historic Districts, and the not landmarked, though culturally and architecturally significant neighborhood of Yorkville. FRIENDS has selected representative sites that we feel exemplify each district’s unique history and character. Each of the districts has its own color-coded map with easy-to-read points that can be used to find your own favorite site, or as a self-guided walking tour the next time you find yourself out strolling on the Upper East Side. -

Prospectus Symp19-8-2019.Indd
EXHIBITOR & PROMOTIONAL PARTNERSHIP PROSPECTUS TH INTERNATIONAL PROSTATE CANCER AND UROLOGIC ONCOLOGY SYMPOSIUM NOVEMBER 7-9, 2019 NEW YORK, NY MOUNTSINAIUROLOGYCME.ORG HIGHLIGHTS • Over 100 world-renowned faculty • Engaging point-counterpoint debates and • Live 3-D surgical demonstrations, including panel discussion prostate, kidney, bladder procedures • Global exposure with international web streaming of select sessions and events Welcome to the Fourth International Prostate Cancer and Urologic Oncology Symposium. EDUCATIONAL HIGHLIGHTS • Live 3-D surgery transmission covering complex urologic surgery • Comprehensive didactic lectures from the world’s leading experts in urologic oncology • Robust review of the latest advances in surgical techniques and management of prostate, kidney, and bladder cancer • Personal interaction with world-class faculty • Stimulating point-counterpoint debates on timely topics DAILY HIGHLIGHTS PROSTATE DAY 1 THUR. 11/7/19 PROSTATE DAY 2 FRI. 11/8/19 KIDNEY & BLADDER SAT. 11/9/19 • Advanced imaging in genomics • Innovations in the management of • New progress in pre-operative and for prostate cancer castrate-sensitive prostate cancer intra-operative imaging, 3-D • Biomarkers and immunotherapy modelling, and ultra sound • Focus on radiomics and guidance for renal tumors radiogenomics • Update on clinical trials for castrate-resistant treatments for • Novel therapeutics in the • Utility of imaging and artificial prostate cancer management of metastatic renal intelligence in prostate cancer cell carcinomas: -

Central Park Playground Map West Side East Side 1
Central Park Playground Map West Side East Side 1. West 110th Street Playground 13. East 110th Street Playground West 110th Street East 110th Street Toddler, pre-school, and school-age School-age 2. Tarr Family Playground 14. Bernard Family Playground West 100th Street East 108th Street Pre-school and school-age Toddler and pre-school 3. Rudin Family Playground 15. Robert Bendheim Playground West 96th Street East 100th Street Pre-school and school-age Pre-school and school-age 4. Tarr-Coyne Wild West Playground 16. Margaret L. Kempner Playground West 93rd Street East 96th Street Pre-school and school-age Pre-school and school-age 5. Safari Playground 17. Ancient Playground West 91st Street East 85th Street Pre-school Pre-school and school-age 6. Abraham and Joseph Spector 18. Ruth and Arthur Smadbeck — Playground Heckscher East Playground West 86th Street East 79th Street Pre-school and school-age Toddler and pre-school 7. Pinetum Playground 19. James Michael Levin Playground West 85th Street East 76th Street Pre-school, school-age, teens, and adults Pre-school and school-age 8. Toll Family Playground 20. East 72nd Street Playground West 85th Street East 72nd Street Toddler and pre-school School-age 9. Diana Ross Playground 21. Billy Johnson Playground West 81st Street East 67th Street Pre-school and school-age Pre-school and school-age 10. Tarr-Coyne Tots Playground West 68th Street Toddler Playground Hours 11. Adventure Playground Open from 8:00 am until dusk, weather West 67th Street permitting. Visit centralparknyc.org/alerts School-age to check if any playgrounds are closed for 12. -

Actions of the Council on Podiatric Medical Education
ACTIONS OF THE COUNCIL ON PODIATRIC MEDICAL EDUCATION April 2019 MEETING, MAIL BALLOTS, AND CONFERENCE CALLS March 1 – May 15, 2019 Approval as a PMSR (effective April 27, 2019) Coney Island Hospital, Brooklyn, New York 1/1/1 New York Community Hospital, Brooklyn, NY, 2/2/2 Approval as PMSR/RRA (effective April 27, 2019) Beaumont Hospital-Wayne, Wayne, MI, 3/3/3 Christus Saint Patrick Hospital, Lake Charles, LA, 1/1/1 Henry Ford Wyandotte Hospital, Wyandotte, MI, 3/3/3 Jackson South Community Hospital, Miami, FL, 1/1/1 James H. Quillen Veterans Affairs Medical Center, Mountain Home, TN, 1/1/1 John Peter Smith Hospital, Fort Worth, TX, 2/2/2 Kennedy University Hospital, Stratford, NJ, 3/3/3 Kingwood Medical Center, Kingwood, TX, 3/3/3 Mercy Health Regional Medical Center, Lorain, OH, 6/6/6 Mount Sinai Beth Israel Medical Center, New York, NY, 4/4/4/4 (The curriculum of the PMSR/RRA program requires completion of 48 months of training.) (effective July 1, 2019) NYU Winthrop Hospital, Mineola, NY, 2/2/2 Ochsner Clinic Foundation, New Orleans, LA, 3/3/3 Richmond University Medical Center, Staten Island, NY, 2/2/2 Roger Williams Medical Center, Providence, RI, 3/3/3 St. Vincent Evansville, Evansville, IN, 2/2/2 Surgical Hospital of Oklahoma, LLC and Cleveland Clinic Foundation, Oklahoma City, OK, 2/2/2 UnityPoint Health - Trinity Regional Medical Center, Fort Dodge, IA, 1/1/1 Veterans Affairs Puget Sound Health Care System, Seattle, WA, 2/2/2 Wake Forest Baptist Health, Winston-Salem, NC, 3/3/3 (effective July 1, 2019) Westchester General Hospital, Miami, FL, 4/4/4 White Memorial Medical Center, Los Angeles, CA, 2/2/2 Probation as PMSR/RRA (Candidate for withdrawal, effective July 1, 2020) Cooper University Hospital, Camden, NJ, 2/2/2 Fountain Valley Regional Hospital and Medical Center, Fountain Valley, CA, 1/1/1 Surgeons Choice Medical Center, Southfield, MI, 3/3/3 Rush University Medical Center, Chicago, IL, 3/3/3 Approval of Program Transfer Captain James A. -

Emergency Response Incidents
Emergency Response Incidents Incident Type Location Borough Utility-Water Main 136-17 72 Avenue Queens Structural-Sidewalk Collapse 927 Broadway Manhattan Utility-Other Manhattan Administration-Other Seagirt Blvd & Beach 9 Street Queens Law Enforcement-Other Brooklyn Utility-Water Main 2-17 54 Avenue Queens Fire-2nd Alarm 238 East 24 Street Manhattan Utility-Water Main 7th Avenue & West 27 Street Manhattan Fire-10-76 (Commercial High Rise Fire) 130 East 57 Street Manhattan Structural-Crane Brooklyn Fire-2nd Alarm 24 Charles Street Manhattan Fire-3rd Alarm 581 3 ave new york Structural-Collapse 55 Thompson St Manhattan Utility-Other Hylan Blvd & Arbutus Avenue Staten Island Fire-2nd Alarm 53-09 Beach Channel Drive Far Rockaway Fire-1st Alarm 151 West 100 Street Manhattan Fire-2nd Alarm 1747 West 6 Street Brooklyn Structural-Crane Brooklyn Structural-Crane 225 Park Avenue South Manhattan Utility-Gas Low Pressure Noble Avenue & Watson Avenue Bronx Page 1 of 478 09/30/2021 Emergency Response Incidents Creation Date Closed Date Latitude Longitude 01/16/2017 01:13:38 PM 40.71400364095638 -73.82998933154158 10/29/2016 12:13:31 PM 40.71442154062271 -74.00607638041981 11/22/2016 08:53:17 AM 11/14/2016 03:53:54 PM 40.71400364095638 -73.82998933154158 10/29/2016 05:35:28 PM 12/02/2016 04:40:13 PM 40.71400364095638 -73.82998933154158 11/25/2016 04:06:09 AM 40.71442154062271 -74.00607638041981 12/03/2016 04:17:30 AM 40.71442154062271 -74.00607638041981 11/26/2016 05:45:43 AM 11/18/2016 01:12:51 PM 12/14/2016 10:26:17 PM 40.71442154062271 -74.00607638041981 -

126 East 86Th Street New York, NY 10028
126 East 86th Street New York, NY 10028 Highlights ··52,210± max ZSF per residential FAR ··C5-1A zoning district, which has an R10 equivalent ··52 feet of frontage along the highly visible 86th Street corridor, which commands retail rents north of $365 / SF ··Few remaining development sites in coveted Upper East Side ··Median prices for new development condominiums in the area have risen by an average of 26% per quarter since the third quarter of 2017 ··Highly successful luxury residential condominiums nearby with sellouts at $2,500 per square foot ··Centrally located amongst a strong retail tenant roster, including H&M, Whole Foods and Maison Kayser ··Steps from the 4, 5 and 6 trains at the 86th Street and Third Avenue Station and the Q train at the 86th Street and Second Avenue Station ··Eligible for off-site inclusionary housing air-rights ··Not subject to Historic District or Landmark Designation Avison Young, as exclusive agent, is pleased to offer for sale 126 East residential neighborhoods. Additionally, the neighborhood has seen 86th Street (the “Property” or “Site”), a development sitxe located a recent influx of new developments, which have performed well on the south side of East 86th Street between Lexington Avenue above the citywide average, a testament to the strong demand for and Park Avenue. As one of the few remaining development sites new construction condominiums in the Upper East Side. in the Upper East Side, the Property provides a developer with The site is located in a C5-1A zone, which has a R10 residential the opportunity to create a highly visible development that will equivalent and offers a developer an opportunity to increase the ZFA permanently join one of Manhattan’s preeminent neighborhoods. -

In the News September 30, 2016
From: ITNDaily on behalf of Werle, Laura Subject: Mount Sinai In the News - September 30, 2016 Date: Friday, September 30, 2016 2:06:09 PM Attachments: ATT00002.txt In the News September 30, 2016 Nature – September 30 Inflammation in Patients With Cushing Disease — Claire Greenhill Circulating levels of proinflammatory cytokines are increased in patients with Cushing disease, both during active disease and after remission, according to new data published in Clinical Endocrinology. These findings demonstrate that cytokine levels are increased in patients after remission of Cushing disease, which could explain the persistent increased risk of cardiovascular-related death. The study, led by Eliza Geer, MD, a professor of endocrinology at the Icahn School of Medicine at Mount Sinai, notes that more studies are needed to determine why levels of IL-6 and IL-1β remain elevated after remission of Cushing disease. - Eliza Geer, MD, Associate Professor, Medicine, Endocrinology, Diabetes and Bone Disease, Neurosurgery, Icahn School of Medicine at Mount Sinai Learn more: http://www.nature.com/nrendo/journal/vaop/ncurrent/full/nrendo.2016.170.html WCBS – September 29 ‘Artificial Pancreas’ Expected To Make Life Easier, Healthier For Type 1 Diabetes Patients — Max Gomez A groundbreaking new device could change the lives of millions of people living with diabetes. Federal regulators just approved an artificial pancreas that can monitor and administer insulin. The key is a computer algorithm that does those calculations faster and more accurately than a patient can. “It looks at the numbers from a moment to moment basis, and it will proactively predict what is going to happen next and make clinical decisions that cannot be done at that rate.