FTC London Conference 2019 Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sunday, November 7, 2021
SUNDAY, NOVEMBER 7, 2021 PRE-CONFERENCE SESSIONS TBA 9:00 AM – 10:30 AM TBA TBA 10:30 AM - Noon TBA Noon - 1:00 PM Lunch OPENING REMARKS 1:00 PM - 1:15 PM Welcome to Adherence 2021 1:15 PM - 1:20 PM Break KEYNOTE ADDRESS Making Up for Lost Time: Critical Steps to Regain Momentum in HIV Prevention and Treatment 1:20 PM - 1:50 PM Meg Doherty, World Health Organization, Geneva, Switzerland* 1:50 PM - 1:55 PM Break HIV TREATMENT ADHERENCE Moderator : Jessica Haberer, Massachussetts General Hospital* and Jean Bisimwa Nachega, University of Pittsbur State-of-the-Art: A Review of Long-Acting Antivirals for HIV Treatment from an Adherence Perspective Susan Swindells, Nebraska AIDS Education Training Center, Omaha, NE, USA* Paradigm Shift: Asssessing Acceptability and Creating Demand for Long-Acting and Extended Release Formulations for HIV Treatment 1:55 PM - 3:10 PM Delivette Castor, Columbia University, New York, NY, USA* Antiretroviral Drug Resistance: Managing the Clinical Challenges of Long-Lasting Drug Concentrations Charlie Flexner, Johns Hopkins University, Baltimore, MD, USA* Discussion (15 minutes) 3:10 PM - 3:40 PM Break IMPLEMENTATION SCIENCE Moderator : Elvin Geng, Washington University of St. Louis* and Juliet Iwelunmor, Saint Louis University* Reaching Youth through Crowd Sourcing Juliet Iwelunmor, Saint Louis University, St. Louis, MO, USA COVID-19 and HIV Services: Disruptive Thinking for Disruptive Times 3:40 PM - 4:55 PM Matt Golden, University of Washington, Seattle, WA, USA Renewing Commitment to Equity in the HIV Response Lisa Bowleg, George Washington University, Washington, DC, USA Discussion (15 minutes) 4:55 PM - 5:00 PM Break THREE TOP-RATED ABSTRACTS 5:00 PM - 6:00 PM 6:00 PM Adjourn MONDAY, NOVEMBER 8, 2021 GARY S. -

Towards a Praxis-Oriented Phenomenological Methodology and Ethics of Deep Travel in Martin Heidegger’S Sojourns
Fast Capitalism ISSN 1930-014X Volume 16 • Issue 2 • 2019 doi:10.32855/fcapital.201902.013 The Solace of the Sojourn: Towards a Praxis-oriented Phenomenological Methodology and Ethics of Deep Travel in Martin Heidegger’s Sojourns Andrew Urie Introduction Martin Heidegger’s little-read travel journal, Sojourns (1962), is a literary-philosophical gem that yields surprisingly fruitful insights into our contemporary era of neoliberal globalization via its implicit exploration of the complex interconnections between travel, phenomenology, and ethics. As I demonstrate in this paper, Sojourns contains an implicit praxis-oriented phenomenological methodology and ethics of global travel that together gesture towards a coherent practice of “deep travel,” which American literature scholar Cinzia Schiavini aptly defines as “a vertical movement in a closed space which starts from the surface of the land and goes backward in time, searching for the hidden social and cultural dynamics embedded in that [given] geographical context” (94). Sociohistorical Context Originally intended as a seventieth birthday gift for Heidegger’s wife, Elfriede, Sojourns bears the following dedication: “To the mother, For her seventieth birthday, A token of Appreciation” (vi). Although penned in 1962 during Heidegger’s first journey to Greece, the text would not be published until 1989, when it was released in Germany as Aufenthalte by the venerable Frankfurt am Main publishing house Vittorrio Klostermann. It would not be available in an official English edition until 2005, -

Athens Democracy Forum 2020 “The New Abnormal: Reimagining Democracy”
Athens Democracy Forum 2020 “The New Abnormal: Reimagining Democracy” The ADF 2020 Themes Even before the current crises, democracy was taking a beating: from hijacked elections to the spread of extreme ideologies to the increasingly sophisticated tactics of strongmen. The effects have become alarmingly apparent: migration shifts, climate change, economic uncertainty and general global unrest, for a start. Since the pandemic hit and the world struggles to get out from under it, the assaults have become even more prevalent, and calls to reinvent democracy are more urgent than ever. Operating for the second year under the aegis of the Democracy and Culture Foundation, in association with The New York Times, the Athens Democracy Forum will convene leaders from government, business, civic society and the nonprofit sector to debate -- and enact -- real solutions to the world’s most pressing issues. The Foundation’s focus on impact is designed to produce the two outcomes of "better governance" and "citizen engagement." Kim Conniff Taber, Editorial Director, Athens Democracy Forum Serge Schmemann, Editorial Board Member, The New York Times and Program Director, Athens Democracy Forum Wednesday, September 30, 2020 ALL TIMES LISTED ARE ATHENS TIME (GMT +3) Hotel Grande Bretagne Studio 1:30 p.m. – 2:20 p.m. Bespoke Panel Discussion: “Business for Purpose” Roundtable Sponsored by Mishcon de Reya and National Bank of Greece What does “business for purpose” really mean? What are the different ways that businesses can acknowledge systemic problems and build toward more systemic change? This session will wrestle with these questions and more. Valerie Keller, Co-founder and CEO, Imagine (P) Alexander Rhodes, Head of Mishcon Purpose (V) Costas Michaelides, Chairman of the Board, National Bank of Greece (P) Mete Coban MBE, Founder and Chief Executive, My Life My Say (P) Moderated by Alison Smale, Journalist and former UN Undersecretary General for Global Communications, and former Executive Editor of the International Herald Tribune (P) Hotel Grande Bretagne Studio 3:00 p.m. -

Aidsimpact 2009 Programme
1 Tuesday # Title Type Times Room Chairs SIDACTION, Tsodilo Vincent Douris, 1 An international measure of Quality of Life specific to PW HIV Satellite 10.00-13:00 B4 Veronica Noseda Tsodilo 2 Ethics of Clinical Research Satellite 10:00-13:00 Sidaction B1+2 Tsodilo 3 HIV considerations in Botswana Satellite 13:00-14:00 Sheila Tlou B1+2 Rosemary Building capacity for HIV/AIDS prevention trials in Africa: Strategies for Serondela 4 Satellite 10:00-12:00 Musonda, meeting a multi-dimensional challenge 3+4 Robert Geneau HSRC, Serondela 46 HIV in South Africa: A Turning Tide Among Teenagers? Satellite 12:00-14:00 Olive Shisana, 3+4 Linda Richter Tsodilo Simon Rosser, 47 Are gay communities dying Satellite 13:00-14:00 B4 William West Sheila Tlou, 5 Opening Ceremony Plenary 14:00-15:00Tsodilo C Batho C. Molomo 5.1OPENING CEREMONY - 14:00-14:05--National Anthem led by NACA Choi 14:05-14:10--Welcome remarks by Prof. Sheila Tlou, Co-Chair, Local Organising Committee 14:10-14:15--Remarks by Prof. Lorraine Sherr, AIDS Impact 14:15-14:20--Remarks Ms. Regina Lesole , Activist, Ms. Stigma-Free 2006 14:20-14:30--Song by NACA choir 5.2Mark Stirling Keynote address - Global HIV Challenges 2 Lorraine Sherr, 6 HIV state of the Art Plenary 15:30-18:00Tsodilo C Pepe Catalan 6.1Olive Shisana HIV in the disabled population: are we doing our part? 6.2Chloe Orkin Anti-retroviral therapy in 2009: what have we learned? 6.3Gita Ramjee HIV Prevention Overview 6.4Bruno Spire Quality of Life and HIV- ANRS Plenary 6.5John De Wit Gay Men 6.6Elly Katabira International AIDS -

3Rd EU HCV Virtual Policy Summit Final Programme "Securing Wider EU Commitment to the Elimination of HCV" Wednesday, 24 March 2021 14:00 – 18:30 CET
3rd EU HCV Virtual Policy Summit Final Programme "Securing Wider EU Commitment to the elimination of HCV" Wednesday, 24 March 2021 14:00 – 18:30 CET Meeting Chairs: Prof Angelos Hatzakis, Prof George Papatheodoridis and Prof Heiner Wedemeyer Hepatitis B&C Public Policy Association Timing Programme Item Speakers 14:00 – Welcome and Introductory comments 14:25 • Welcome and scene setting Prof Heiner Wedemeyer, Co-Chair “5 years on: Revisiting the Elimination Manifesto” HepBCPPA and Hannover Medical School, Germany Prof George Papatheodoridis, Co-chair HepBCPPA and University of Athens Medical School, Greece • Introductory comments on the continued need/opportunity to eliminate HCV in Europe - European Association for the Study of the Liver Prof Maria Buti, EU Policy Councillor, EASL - ACHIEVE Coalition Mr George Kalamitsis, Co-Chair ACHIEVE Coalition and Chair, Liver Patients International - WHO Europe Dr Antons Mozalevskis, WHO Europe - European Parliament Mr Petros Kokkalis, MEP, Greece 14:25 – Keynote addresses Chair: Prof Rafael Esteban Mur 14:55 Co-Chair HepBCPPA and University Hospital Vall d'Hebron, Barcelona, Spain • How the EU can help deliver on the WHO elimination goal for Mr John F Ryan, Director of Public viral Hepatitis B and C Health, Country Knowledge, Crisis Management, DG SANTE, European Commission • The elimination of viral hepatitis as a public health threat in Mr Alexis Goosdeel, Director, the EU : Keeping People Who Inject Drugs in focus European Monitoring Centre for Drugs and Drug Addiction 14:55 – Session 1. Progress -
Boston March 4-7, 2018 Program and Conference Information
Program and Conference Information Conference on Retroviruses and Opportunistic Infections Boston March 4-7, 2018 General Information CONTENTS Information General CROI FOUNDATION ...........................................................2 IAS–USA.......................................................................2 CROI 2018 PROGRAM COMMITTEE.........................................3 Scientific Program Committee .........................................3 Community Liaison Subcommittee .....................................5 EXTERNAL REVIEWERS . 6 SCHOLARSHIP AWARDEES ..................................................8 New Investigator Awardees.................................................8 International Investigator Awardees .......................................12 Community Educator Awardees............................................12 CONTINUING MEDICAL EDUCATION ......................................13 GENERAL INFORMATION . .15 Overview .................................................................15 Conference Support .......................................................15 Americans With Disabilities Act ............................................15 Emergency Services . .15 Embargo Policies and Social Media ....................................16 Welcome Reception .......................................................16 Meals.....................................................................16 Overflow Accommodations for Oral Sessions................................17 Mobile App ...............................................................17 -
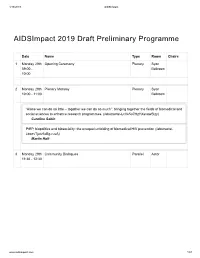
Aidsimpact 2019 Draft Preliminary Programme
4/16/2019 AIDSImpact AIDSImpact 2019 Draft Preliminary Programme Date Name Type Room Chairs 1 Monday 29th Opening Ceremony Plenary Syon 09:00 - Ballroom 10:00 2 Monday 29th Plenary Monday Plenary Syon 10:00 - 11:00 Ballroom “Alone we can do so little – together we can do so much”: bringing together the fields of biomedical and social sciences to enhance research programmes. (/abstracts/-LcVe5o7HzYXsvawSlzy) Caroline Sabin PrEP, biopolitics and biosociality: the unequal unfolding of biomedical HIV prevention (/abstracts/- LbaevTjutv6xBg-ruvA) Martin Holt 3 Monday 29th Community Dialogues Parallel Astor 11:30 - 12:30 www.aidsimpact.com 1/57 4/16/2019 AIDSImpact Date Name Type Room Chairs South African adolescent girls’ and young women’s narratives of communication with and support from parents and teachers: implications for sexual and reproductive health decisions (/abstracts/- LZtCv6dXuEhYZ5V5V8n) Zoe Duby, Kim Jonas, Kealeboga Maruping, Ashleigh LoVette, Caroline Kuo, Catherine Mathews The embodied relationality of blood-borne viruses: How families matter in the context of a stigmatised viral infection (/abstracts/-LZqqpIxbkjOKRBI0o8y) Asha Persson, Christy Newman, Myra Hamilton, Joanne Bryant, kylie valentine, Kerryn Drysdale, Rebecca Gray A support for autonomy for people living with HIV in West Guina: health and associative professionals’ discourses and visions on a complex phenomenon. (/abstracts/-LZfTrHBB_l_aYW52RT1) Anne-Sophie Petit, Nikos Kalampalikis, Marie Préau Adherence and retention in a community-based trial testing PrEP -
Croi 2021 Program Committee
General Information CONTENTS WELCOME . 2 General Information General Information OVERVIEW . 2 CONTINUING MEDICAL EDUCATION . 3 CONFERENCE SUPPORT . 4 VIRTUAL PLATFORM . 5 ON-DEMAND CONTENT AND WEBCASTS . 5 CONFERENCE SCHEDULE AT A GLANCE . 6 PRECONFERENCE SESSIONS . 9 LIVE PLENARY, ORAL, AND INTERACTIVE SESSIONS, AND ON-DEMAND SYMPOSIA BY DAY . 11 SCIENCE SPOTLIGHTS™ . 47 SCIENCE SPOTLIGHT™ SESSIONS BY CATEGORY . 109 CROI FOUNDATION . 112 IAS–USA . 112 CROI 2021 PROGRAM COMMITTEE . 113 Scientific Program Committee . 113 Community Liaison Subcommittee . 113 Former Members . 113 EXTERNAL REVIEWERS . .114 SCHOLARSHIP AWARDEES . 114 AFFILIATED OR PROXIMATE ACTIVITIES . 114 EMBARGO POLICIES AND SOCIAL MEDIA . 115 CONFERENCE ETIQUETTE . 115 ABSTRACT PROCESS Scientific Categories . 116 Abstract Content . 117 Presenter Responsibilities . 117 Abstract Review Process . 117 Statistics for Abstracts . 117 Abstracts Related to SARS-CoV-2 and Special Study Populations . 117. INDEX OF SPECIAL STUDY POPULATIONS . 118 INDEX OF PRESENTING AUTHORS . .122 . Version 9 .0 | Last Update on March 8, 2021 Printed in the United States of America . © Copyright 2021 CROI Foundation/IAS–USA . All rights reserved . ISBN #978-1-7320053-4-1 vCROI 2021 1 General Information WELCOME TO vCROI 2021 Welcome to vCROI 2021! The COVID-19 pandemic has changed the world for all of us in so many ways . Over the past year, we have had to put some of our HIV research on hold, learned to do our research in different ways using different tools, to communicate with each other in virtual formats, and to apply the many lessons in HIV research, care, and community advocacy to addressing the COVID-19 pandemic . Scientists and community stakeholders who have long been engaged in the endeavor to end the epidemic of HIV have pivoted to support and inform the unprecedented progress made in battle against SARS-CoV-2 . -

List of Participants ◼
ECFR ANNUAL COUNCIL MEETING 27 -28 June 2016 #ECFR16 ◼ LIST OF PARTICIPANTS ◼ A Asger Aamund (Denmark) President and CEO, A. J. Aamund A/S; Chairman of Bavarian Nordic A/S Rebecca Adler-Nissen (Denmark) Professor, Department of Political Science, University of Copenhagen @RebAdlerNissen Martti Ahtisaari (Finland) Emeritus Chair, ECFR; former President of Finland Yoeri Albrecht (The Netherlands) Director, De Balie @YoeriAlbrecht Douglas Alexander (United Kingdom) Former Secretary of State for International Development @D_G_Alexander Joaquín Almunia (Spain) Former Vice President of the European Commission and Commissioner for Competition @AlmuniaJoaquin Luís Amado (Portugal) Former Minister of Foreign Affairs; former Minister of Defence Giampiero Auletta Armenise (Italy) Chairman, Rothschild Bank (Italy) B Gordon Bajnai (Hungary) Former Prime Minister @Bajnai_Gordon Kostas Bakoyannis (Greece) Governor of Central Greece @KBakoyannis Host partners Sponsors ECFR ANNUAL COUNCIL MEETING 27 -28 June 2016 #ECFR16 Juraj Bayer (Slovakia) CFO and Member of the Board, ZSE Energia Dick Benschop (The Netherlands) President Director, Shell Netherlands @DickBenschop Carl Bildt (Sweden) Co-chair of the Board of ECFR; former Prime Minister; former Minister of Foreign Affairs @carlbildt Emma Bonino (Italy) Co-chair of the Board of ECFR; former Minister of Foreign Affairs @emmabonino Stine Bosse (Denmark) Chairman, Non-Executive Board Member; Adjunct Professor, Copenhagen Business School @BosseStine Sandra Breka (Germany) Senior Vice President, Robert Bosch -

Reframing EU-Russia Relations
“We are living through a global counter-revolution. The institutions and values of liberal internationalism are being eroded beneath our feet and societies are becoming increasingly polarised. The consensus for EU action is increasingly difficult to forge, but there is a way forward. In this new world, on our tenth anniversary, the European Council on Foreign Relations will take a bottom-up approach to building grassroots consensus for greater cooperation on European foreign and security policy. Our vision is to demonstrate that engaging in common European action remains the most effective way of protecting European citizens. But we will reach out beyond those already converted to our message, framing our ideas and calls for action in a way that resonates with key decision- makers and the wider public across Europe’s capitals.” Mark Leonard, Director “ We believe a common foreign policy will allow individual countries to increase their global influence. A strong European voice in favour of human rights, democracy and international law will not just benefit Europeans; it will be good for the world.” Martti Ahtisaari, Joschka Fischer, Mark Leonard and Mabel van Oranje writing in the Financial Times, 1 October 2007 ecfr.eu Our leadership The European Council on Foreign Relations We provide a safe meeting space for decision- (ECFR) is an award-winning international makers and influencers to share ideas for think-tank that aims to conduct cutting-edge common action; we promote informed debate independent research in pursuit of a on Europe’s role in the world; and we build coherent, effective and values-based pan-European coalitions for policy change. -

Day 1 | Monday, May 10, 2021
DAY 1 | MONDAY, MAY 10, 2021 11.00 OPENING SESSION *Language: Greek KEYNOTE REMARKS H.E. Katerina Sakellaropoulou, President of the Hellenic Republic KEYNOTE REMARKS H.E. Kersti Kaljulaid, President of the Republic of Estonia KEYNOTE REMARKS H.E. Zuzana Čaputová, President of the Slovak Republic (video message) OPENING REMARKS Margaritis Schinas, Vice President, Promoting our European Way of Life, European Commission, Belgium OPENING REMARKS His Beatitude Hieronymos II, Archbishop of Athens and All Greece OPENING REMARKS Gianna Angelopoulos-Daskalaki, President, Greece 2021 Committee, Greece Chair: Symeon G. Tsomokos, Delphi Economic Forum HOW HISTORY CAN HELP US MEET CHALLENGES Language: English* Margaret MacMillan, Professor of History, University of Toronto, Canada Chair: Nik Gowing, Co-Director, Thinking the Unthinkable, UK CULTURE & THE PANDEMIC Language: Greek with English subtitles Rector Hélène Ahrweiler, President, Administration Council, European Cultural Centre of Delphi, Greece Marianna V. Vardinoyannis, Goodwill Ambassador, UNESCO, United Nations “Nelson Mandela Prize 2020”, Greece Chair: Antonis Sroiter, Anchorman, Alpha TV, Greece *=English/Greek Translation provided for online audience 1 DAY 1 | MONDAY, MAY 10, 2021 STREAM APOLLON 12.25 ΒREAK 12.30 1821-2021: AN ACCOUNT OF TWO CENTURIES OF EXISTENCE Language: Greek* Under the Auspices of “Greece 2021” Committee Content Partner: Alpha Bank Historical Archives Kostas Kostis, Prof. of Economic and Social History, University of Athens; Advisor to the Mngmt, Alpha Bank Nikiforos Diamandouros, Professor Emeritus, Political Science, University of Athens, Greece Efi Gazi, Professor of Modern History, University of the Peloponnese, Greece Tassos Giannitsis, Alternate Minister of Foreign Affairs 2001-2004, Prof. Emeritus, University of Athens, Greece Stathis Kalyvas, Gladstone Professor of Government, Department Politics & Int. -

Ursula Von Der Leyen President European Commission Rue De La Loi/ Wetstraat 200 BE-1049 Brussels 1
Ursula von der Leyen President European Commission Rue de la Loi/ Wetstraat 200 BE-1049 Brussels 1 2 March 2020 Dear President von der Leyen, Taking meaningful, measurable and sustainable action on climate change is the defining struggle of our time and a policy challenge of unprecedented scale for European and global policy-makers alike. We wholeheartedly welcome the European Commission’s proposal for a European Green Deal and we fully support the ambition for Europe to become the world’s first climate-neutral continent by 2050. The European Green Deal rightly recognizes that an effective response to the climate emergency can only happen through systemic change. Cities led by elected leaders now represent two-thirds of Europe’s population, and are responsible for the bulk of its climate mitigation and adaptation efforts. The fight against climate change will be won or lost in cities. As countless examples from recent years have shown, local governments often take the lead in climate action and realize ambitious action plans for a sustainable future. Cities are well equipped to enact policy change. Local authorities are usually faster to act and less constrained by the pressures from the fossil fuel industry than national governments. Europe’s major cities and metropolitan areas are key and willing players in the all-European climate fight and need to be empowered accordingly. We were encouraged by the European Green Deal Communication’s professed intent to empower regional and local communities, as well as strengthening the urban dimension of cohesion policy with special regard to the European Urban Initiative.