AACN Essentials of Critical-Care Nursing Pocket Handbook, Second
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Article (PDF)
Advances in Engineering Research, volume 205 Proceedings of the 3rd Green Development International Conference (GDIC 2020) The Development of Information Systems in Documentation Management of Critical Care Nursing Fadliyana Ekawaty1*, Dini Rudini2 1Faculty of Medicine and Health Sciences, Universitas Jambi 2Faculty of Medicine and Health Sciences, Universitas Jambi *Corresponding author. Email: [email protected] ABSTRACT Intensive Care Unit (ICU) is one of the units in the hospital that clients receive intensive medical care and monitoring. There, nurses carry out the nursing care process. All steps in the process must be properly documented. Although nursing care documentation is very important for both patients and nurses, but in reality there are still many incomplete nursing care documentations. The nurses’ awareness to completely fill the documents is still lack. Currently, many technological developments have been developed to support activities/work in various fields. one of them is the development of health information system, a nursing management system. So, this research aims to produce a product in the form of ICU nursing care documentation software that enable nurses in documenting their nursing care easier and well documented. The method used at this research is a product-oriented development model. The stages are: 1). Initiation System (initiation of the system), 2). Analysis System, 3). Design System and 4). Production that then tested through the prototype Black Box Testing. The research result shows that this software very useful because it shortens the time for preparing reports. Even this study uses students as research objects, nurses who work in the hospital also can use this software. -
15-Coned-Ccrn-Cardiovascular.Pdf
1 Cardiovascular Introduction A. Anatomy & Physiology B. Cardiac Assessment 1. Cardiac Risk Factors Non Modifiable Age Gender Family History Race Modifiable Smoking Hypertension Diabetes Obesity Stress Exercise Hyperlipidemia 2. Medical & Surgical History 3. Social History 4. Medication History 5. Physical Exam 2 Color Pulses Rate & Rhythm PMI Location Extremity Temperature Dyspnea Fatigue Level Fluid Retention Palpitations Dizziness 6. Chest Pain Exam PQRST Assessment P: Pain, Placement, Provocation Q: Quality (sharp, stabbing, pressure) , Quantity R: Radiation, Relief S: Severity, Systems (nausea, sweaty, dizziness) T: Timing (when it started, how long did it last, what makes it better or worse) C. Diagnostic Tests & Procedures 1. 12 Lead ECG 2. Echocardiography (Transthoracic and Transesepheal) 3. Stress Test 4. Cardiac Catheterization 5. Doppler Ultrasound 6. Blood Work Acute Coronary Syndrome Cardiac Enzymes: CK-MB, Amino Acids: Troponins Heme Proteins: Myoglobin Lipid Profile Triglycerides Cholesterol Low Density Lipoproteins High Density Lipoprotein Coagulation Profile PT/INR aPTT ACT 3 Misc B Type Naturetic Peptide – BNP C Reactive Protein Homocysteine Hemodynamic Monitoring/Assessment CARDIAC OUTPUT HEART RATE X STROKE VOLUME PRELOAD + AFTERLOAD + CONTRACTILITY + The volume of blood in the The pressure or resistance the LV must contract The ability of the against or overcome to eject the blood or create ventricle at end diastole. systole. myocardium to contract. Total Blood Volume -

Tele Critical Care Implementation and Education Project
The University of San Francisco USF Scholarship: a digital repository @ Gleeson Library | Geschke Center Master's Projects and Capstones Theses, Dissertations, Capstones and Projects Summer 8-5-2020 Tele Critical Care Implementation and Education Project Jeffrey Dover [email protected] Follow this and additional works at: https://repository.usfca.edu/capstone Part of the Critical Care Nursing Commons, and the Telemedicine Commons Recommended Citation Dover, Jeffrey, "Tele Critical Care Implementation and Education Project" (2020). Master's Projects and Capstones. 1059. https://repository.usfca.edu/capstone/1059 This Project/Capstone is brought to you for free and open access by the Theses, Dissertations, Capstones and Projects at USF Scholarship: a digital repository @ Gleeson Library | Geschke Center. It has been accepted for inclusion in Master's Projects and Capstones by an authorized administrator of USF Scholarship: a digital repository @ Gleeson Library | Geschke Center. For more information, please contact [email protected]. TCC IMPLEMENTATION & EDUCATION PROJECT 1 Practicum Prospectus: Tele Critical Care Implementation and Education Project Jeffrey Dover University of San Francisco TCC IMPLEMENTATION & EDUCATION PROJECT 2 TABLE OF CONTENTS Section I: Title and Abstract Title ........................................................................................................................... 1 Abstract .................................................................................................................... -
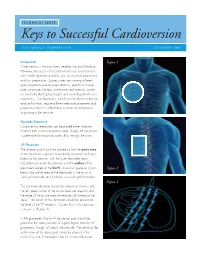
Keys to Successful Cardioversion
TECHNICAL NOTE: Keys to Successful Cardioversion ZOLL MEDICAL CORPORATION DECEMBER 2009 Introduction Figure 1 Cardioversion is the most direct treatment for atrial fibrillation. However, the success of a cardioversion can be enhanced with careful attention to details, such as electrode placement and skin preparation. Success rates vary among different types of patients and among institutions, and this technical note summarizes the keys to enhance cardioversion success as shared by electrophysiologists and cardiologists with vast experience. Cardioversions, which are intended to terminate atrial arrhythmias, require different electrode placement and preparation than for defibrillation to terminate arrhythmias originating in the ventricle. Electrode Placement Cardioversion electrodes can be placed either Anterior– Posterior (AP) or Anterior-Anterior (AA), though AP placement is preferable for maximum current flow through the atria. AP Placement The anterior pad should be placed so that the active area of the electrode is placed immediately adjacent and right lateral to the sternum, with the outer electrode foam circumference under the clavicle and the midline of the electrode located at the fourth intracostal space as shown Figure 2 below (the active area of the electrodes is the tin on a solid gel electrode and the foam on a wet gel electrode). Figure 3 The posterior electrode should be placed as shown, with the left upper corner of the active area sub-scapular and the edge of the active area immediately left lateral to the spine. The center of the electrode should be placed at the level of the T7 vertebra. Current flow in this position is shown in (Figure 3) . In AA placement (Figure 4) the sternal pad should be placed in the same position or slightly higher than for AP placement, though still below the clavicle. -

State of Missouri Physician Manual
STATE OF MISSOURI PHYSICIAN MANUAL Physician SECTION 1-PARTICIPANT CONDITIONS OF PARTICIPATION ........................................22 1.1 INDIVIDUALS ELIGIBLE FOR MO HEALTHNET, MANAGED CARE OR STATE FUNDED BENEFITS........................................................................................................................22 1.1.A DESCRIPTION OF ELIGIBILITY CATEGORIES.............................................................22 1.1.A(1) MO HealthNet...............................................................................................................22 1.1.A(2) MO HealthNet for Kids.................................................................................................23 1.1.A(3) Temporary MO HealthNet During Pregnancy (TEMP)................................................25 1.1.A(4) Voluntary Placement Agreement for Children .............................................................25 1.1.A(5) State Funded MO HealthNet.........................................................................................25 1.1.A(6) MO Rx...........................................................................................................................26 1.1.A(7) Women’s Health Services .............................................................................................26 1.1.A(8) ME Codes Not in Use ...................................................................................................27 1.2 MO HEALTHNET AND MO HEALTHNET MANAGED CARE ID CARD......................27 1.2.A FORMAT OF MO HEALTHNET -

Nurse Anesthesia Program 642 Anesthesia Techniques, Procedures Are Not Allowed to Work at Any Time As an Anesthesia 209 Carroll Street and Simulation Lab 4 Provider
Accreditation: CORE COURSES: CR The program is fully accredited by the 561 Advanced Phys. Concepts-Health Care I 3 Council on Accreditation of Nurse Anesthesia Educational 562 Advanced Phys. Concepts-Health Care II 3 Program, and the American Association of Colleges of ADDITIONAL INFORMATION 603 Theoretical Basis 3 Nursing. 606 Information Management in Nursing 3 Information in this brochure is subject to change. 607 Policy Issues 2 Call program office for additional information at Employment: Limited student employment of one day 619 Principles of Evidence-Based Practice 3 per week as an RN is allowed in the first 12 months as long 330-972-3387 NURSING Total 17 as progress is satisfactory in the program. Employment The University of Akron OF for the last 15 months of residency is discouraged due NURSING ANESTHESIA (NA) to both academic and clinical responsibilities. Students Nurse Anesthesia Program 642 Anesthesia Techniques, Procedures are not allowed to work at any time as an anesthesia 209 Carroll Street and Simulation Lab 4 provider. Akron, OH 44325-3701 640 Scientific Components of NA 3 SCHOOL 643 Advanced Health Assess. & Prin. of NA I 4 Student Financial Aid Loans, stipends, grants and Brian P Radesic 645 Advanced Health Assess. & Prin. of NA II 4 scholarships are available on a limited basis. DNP, MSN, CRNA 641 Advanced Pharmacology for NA I 3 Program Director 644 Advanced Pharmacology for NA II 3 Non-discrimination Statement: The program does not 647 Professional Roles for Nurse Anesthetist 2 discriminate on the basis of race, color, religion, age, 637 NA Residency I 4 gender, nationality, marital status, disability, sexual 646 NA Residency II 4 Melody Betts orientation, or any factor protected by law. -

CVP)/Right Atrial (RA) Catheter: Pressure Measurement, Removal
Critical Care Specialty Procedural Guideline D-6.1 Central Venous (CVP)/Right Atrial (RA) Catheter: Pressure Measurement, Removal Policy Statement(s) Pressure Measurement • CVP or RA represents right ventricular (RV) function and is used to evaluate right-sided heart preload. Normal 2-8 mmHg. • Monitoring trends in CVP is more meaningful than a single reading. • Central venous access may be obtained in a variety of places: • internal jugular vein • subclavian vein • femoral vein • external jugular vein • CVP waveform normally has a, c, v waves present. Removal • An RN can remove a central venous catheter with a physician's order. • The central venous catheter tip is obtained for culture : • Upon order of a physician. • If there is evidence of infection at the site. • If the patient's temperature is elevated. • After removal, cleanse CVP or RA catheter site with alcohol and apply an occlusive dressing. Procedural Guideline(s) • Pressure Measurement • Removal Pressure Measurement 1. Assure transducer has been leveled, zeroed and the square wave test is adequate. 2. Observe pressure tracing (Figure 1) to validate CVP tracing. 3. Pressure readings may be obtained with the patient's head elevated up to 45 degrees as long as the transducer is leveled to the phlebostatic axis. Figure 1 4. CVP waveform consists of (Figure 2): • A wave which correlates with PR interval of the ECG tracing. • C wave which correlates with the end of QRS. • V wave which correlates with after the T wave. 5. Measure the mean of the A wave to obtain pressure. Figure 2 6. The mean of the A wave generally will be consistent with the monitor value displayed unless large A waves are present. -

Efccna Competency Tool for European Critical Care Nurses 2013
2013 EfCCNa Competencies for European Critical Care Nurses European federation of Critical Care Nursing associations – EfCCNa Contents DEVELOPED BY 3 INTRODUCTION 4 BACKGROUND 4 HOW TO USE 5 COMPETENCY TOOL 7 CLINICAL DOMAIN 8 PROFESSIONAL DOMAIN 14 MANAGEMENT DOMAIN 17 EDUCATION & DEVELOPMENT DOMAIN 21 2 Developed by The European federation of Critical Care Nursing associations (EfCCNa) Education Committee (2013) David Waters (United Kingdom) Anne Kokko (Finland) Heike Strunk (Germany) Evanthia Georgiou (Cyprus) Maria Hadjibalassi (Cyprus) Drago Satosek (Slovenia) Karin Klas (Austria) 3 Introduction Critical care is a complex and dynamic specialty, which aims to treat the delicate health needs of the acutely or critically ill patient and their families. The role of the critical care nurse is invaluable in the delivery of evidence-based care and remains a core member of the critical care multi-professional team. Due to the increasing complexity and holistic nature of critical care delivery, the critical care nurse is required to have a unique combination of skills, knowledge and attitudes. To ensure that the critical care nurse is fit for purpose and competent to perform their role, the appropriate training and development opportunities should be provided; examples include post- registration critical care training and local competency tools. Background In 2009 the EfCCNa Education Committee commenced work on a project to develop a European Critical Care Nursing competency framework that could be utilised in practice to assess competence and facilitate continuing professional development (CPD). The motivation for pursuing this project came from member associations within EfCCNa, who reported the need for a competency assessment tool that could allow competence to be mapped, but also to articulate an acceptable level of clinical skill and knowledge for the critical care nursing workforce across Europe. -

The Roles of Critical Care Advanced Practice Nurse
Journal of Korean Academy of Nursing (2006) Vol. 36, No. 8, 1340-1351 The Roles of Critical Care Advanced Practice Nurse Sung, Young Hee1, Yi, Young Hee1, Kwon, In Gak1, Cho, Yong Ae1 Purpose. To determine and compare the perception among nurses and doctors of the roles and tasks of critical care advanced practice nurses (APNs) in order to establish standardized and formally agreed role criteria for such critical care APNs. Method. This study measured and analyzed the necessity of each of the roles and tasks of critical care APNs, as perceived by nurses and doctors, through a survey of 121 participants: 71 nurses in 7 intensive care units (ICUs) at a general hospital in Seoul, and 50 doctors who used ICUs. Data collection utilized a questionnaire of 128 questions in the following fields: direct practice (79), leadership and change agent (17), consultation and collaboration (15), education and counseling (11), and research (6). Results. Both the nurses’ and the doctors’ groups confirmed the necessity of critical care APNs, with doctors who frequently used ICUs indicating a particularly strong need. As for the priority of each role of critical care APNs, the nurses considered direct practice to be the most critical, followed by education and counsel- ing, research, consultation and collaboration, and leadership and change agent. The doctors also considered direct practice to be the most critical, followed by education and counseling, consultation and collaboration, research, and leadership and change agent. There was a statistically significant difference between how the two groups regarded all the roles, except for the consultation and collaboration roles. -

The Intensive Care Unit
The Intensive Care Unit Information for relatives, friends and carers ContentsContents Introduction 3 What is the Intensive Care Unit? 4 Where are the Intensive Care Units? 4 What happens when a patient is taken to ICU? 5 Visiting the unit 6 How do I get into ICU? 6 Visiting times 6 Who can visit? 6 Telephoning the hospital 7 Information about your relative 7 Using telephones 7 How can I help restrict infection? 8 What can I expect when I enter ICU? 9 Can I touch my relative? 9 Can I talk to my relative? 10 Can I get involved in my relative’s care? 10 Who is looking after my relative? 11 How to identify staff 14 What are ward rounds? 15 Does a patient need any personal items in ICU? 15 Clothing and valuables 15 Personal items and toiletries 15 Practicalities when visiting the hospital 16 Transportation 16 Facilities 16 Can I stay overnight? 17 Shops and hospital services 17 Cashpoint 17 Who else might be able to help me? 18 2 Looking after yourself 18 Chaplaincy and Spiritual Care Department, Ext. 4122 18 What if I want to make a suggestion, comment or complaint? 18 The Patient Advice and Liaison Service (PALS), Ext. 4029 19 Interpreter and Communication Services 19 How long will my relative need intensive care? 19 Patient transfer 20 If a patient dies 20 What to expect following discharge of a recovering patient from ICU 21 Follow up from ICU after hospital discharge 22 ICUsteps support group 22 Sources of help/useful Information 23 IntroductionIntroduction It can be frightening when your relative is admitted to the Intensive Care Unit (ICU). -

A Retrospective Analysis of Nursing Documentation in the Intensive Care Units of an Academic Hos P Ital in the Wes Tern Cap E
A RETROSPECTIVE ANALYSIS OF NURSING DOCUMENTATION IN THE INTENSIVE CARE UNITS OF AN ACADEMIC HOS P ITAL IN THE WES TERN CAP E by Dawn Sharon Hector Thesis presented in partial fulfillment of the degree of Magister Curationis (Nursing) at the Stellenbosch University Division of Nursing Faculty of Health Science Supervisor: Dr. E.L.Stellenberg Date: March 2010 ii DECLARATION By submitting this thesis electronically, I declare that the entirety of the work contained therein is my own, original work, that I am the owner of the copyright thereof (unless to the extent explicitly otherwise stated) and that I have not previously in its entirety or in part submitted it for obtaining any qualification. Signature Date: Copyright © 2009 Stellenbosch University All rights reserved iii ABSTRACT Critical care nursing is the specialty within nursing that deals with an individual's response to life-threatening problems. These life threatening problems require continuous in-depth assessment and intense therapeutic measures and interventions. The level of nursing care is intense and the amount of documentation is enormous in the intensive care unit. Failure to document any aspects, may threaten the continuity of care and patient safety. Furthermore, it may result in negligence that may result in litigation. The purpose of this study was to retrospectively analyse nursing documentation in the intensive care units of an academic hospital in the Western Cape. The objectives set for this study were to determine whether the documentation of the: • assessment of the patients were adequate; • diagnoses were based on the assessment; • nursing care plans were based on the diagnoses; • nursing care plans were implemented and • nursing care plan shows evidence of continuous evaluation A retrospective exploratory- descriptive research design with a quantitative approach was applied to audit objectively the status of nursing documentation of patients who were admitted to the ICU’s of an academic hospital in the Western Cape in the first 48 hours of admission. -

**Induction for Critical Care Staff
**INDUCTION FOR For transfer to CRITICAL CARE Intensive Care STAFF Education Team March 2020 Welcome to Critical Care at MFT Name Contact Phone Number Starting Department Line Manager Firstly, Critical Care would like to take this opportunity to thank you for your support in assisting in the Covid-19 escalation plan. The following document and competencies are to support your temporary return to Critical Care. The competencies and study day/s will help you deliver safe care while looking after critical care patients. If you require further information that is not included within this document please do not hesitate to ask either the Education Team or any member of the Critical Care Team. General Information Telephone Numbers Switchboard (0161) 2761234 Contact for Sickness – Absence Manager 03308080260 Cardiac Critical Care (0161)2764544 Intensive Care Unit (0161) 2764712/3 High Dependency Unit (0161) 2764166 Trafford High Care Unit (0161) 7462196 Critical Care refers to patients who require a higher level of care than the normal ward patient, level 2 and 3 patients. The NHS has four levels of patients; Level 0 Ward patients who require minimal assistance and only require Observations once per day. Level 1 Ward patients who require some assistance and Observations 4 hourly. Level 2 Patients who require close monitoring and assistance and hourly/2 hourly Observations. Level 3 Patients who require organ support usually ventilation and continuous invasive monitoring. Critical Care at MFT comprises of; General Critical Care- Intensive Care Unit (ICU) MRI (20 Beds) High Dependency Unit (HDU) MRI (20 Beds) Trafford High Care Unit (THCU) TGH (4 Beds) Central Delivery Unit (CDU) St Marys Hospital Cardiac Intensive Care Unit (CICU) MRI (16 Beds) Reading List Books Adam, S.