Abstracts for the Posters
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Buckinghamshire Attractions
Silverstone Race Track Stowe Milton Keynes Stowe Buckingham Old Gaol Buckingham Bletchley Park Buckingham Brewery M1 Claydon winslow Green Dragon Eco Farm Aylesbury Vale Bicester Ascot House village Wing Buckinghamshire Railway Centre Mentmore Waddesdon Manor Waddesdon Aylesbury Bernwood Royal Grebe Canal Waterside Theatre Hunting Forest Cruises Vale Brewery Aylesbury Ashridge County Museum Brill Hartwell House and Roald Dahl Magnolia Park Children’s Gallery Ickneild way Orchard View Farm Stoke Mandeville Grand union Canal Haddenham Guttman Centre XT Brewing The Chiltern Company Wendover Brewery OXFORD Princes Coombe Hill Risborough M40 Whiteleaf Chinnor and Princes Great missenden Risborough Railway chesham Lacey Green Roald Dahl Museum and Story Centre Malt The Brewery Amersham Red Kite viewing point Hughenden Manor west wycombe Buckinghamshire is one of the most filmed counties Hellfire Caves with blockbuster such Harry Potter and James Bond, The Artichoke together with the popular television series high wycombe Midsummer Murders using it’s scenic countryside and historic buildings as backdrops. M25 beaconsfield The Chilterns is an Area of Outstanding Natural Beauty ideal for walkers and bikers and an excellent Bekonscot Model viewpoint to spot Redkites. It’s the only AONB that The Rebellion Chiltern Open can be reached by the London Underground, is the Beer Company Village and Railway London 4th largest in the UK and has over 12,000 miles of Air Museum walks within it. Marlow denham The Hand Odds Farm With a thriving community of independent and Flowers food and drink providers, farmers markets Buckinghamshire and Michellin Starred restaurants, Buckinghamshire is a food lovers heaven. Stoke Park Iver Buckinghamshire has more golf courses than any other county in England. -

Aylesbury Vale Community Chest Grants April 2014 - March 2015
Aylesbury Vale Community Chest Grants April 2014 - March 2015 Amount Granted Total Cost Award Aylesbury Vale Ward Name of Organisation £ £ Date Purpose Area Buckinghamshire County Local Areas Artfully Reliable Theatre Society 1,000 1,039 Sep-14 Keyboard for rehearsals and performances Aston Clinton Wendover Aylesbury & District Table Tennis League 900 2,012 Sep-14 Wall coverings and additional tables Quarrendon Greater Aylesbury Aylesbury Astronomical Society 900 3,264 Aug-14 new telescope mount to enable more community open events and astrophotography Waddesdon Waddesdon/Haddenham Aylesbury Youth Action 900 2,153 Jul-14 Vtrek - youth volunteering from Buckingham to Aylesbury, August 2014 Vale West Buckingham/Waddesdon Bearbrook Running Club 900 1,015 Mar-15 Training and raceday equipment Mandeville & Elm Farm Greater Aylesbury Bierton with Broughton Parish Council 850 1,411 Aug-14 New goalposts and goal mouth repairs Bierton Greater Aylesbury Brill Memorial Hall 1,000 6,000 Aug-14 New internal and external doors to improve insulation, fire safety and security Brill Haddenham and Long Crendon Buckingham and District Mencap 900 2,700 Feb-15 Social evenings and trip to Buckingham Town Pantomime Luffield Abbey Buckingham Buckingham Town Cricket Club 900 1,000 Feb-15 Cricket equipment for junior section Buckingham South Buckingham Buckland and Aston Clinton Cricket Club 700 764 Jun-14 Replacement netting for existing practice net frames Aston Clinton Wendover Bucks Play Association 955 6,500 Apr-14 Under 5s area at Play in The Park event -

5 Year Housing Land Supply Position Statement June 2018
Aylesbury Vale District Council - Five year housing land supply position statement, June 2018 Purpose of this position statement 1.0 Paragraph 47-49 of the National Planning Policy Framework (NPPF, 2012) requires local planning authorities to identify and keep up-to-date a deliverable five year housing land supply against their housing requirements. Where the Council cannot demonstrate a 5 year housing land supply, there is a presumption in favour of sustainable development in line with the NPPF (para 14). Having an understanding of supply is also key to fulfilling the NPPF requirement to demonstrate the expected rate of housing delivery and how housing targets will be met (paragraph 47). 1.1 This position statement sets out the approach to meeting housing requirements in Aylesbury Vale pending the adoption of the new Local Plan (the Vale of Aylesbury Local Plan, VALP). This statement sets out how the current housing supply has been calculated, and the housing requirement target, to be used by the Council in order to apply the appropriate development plan policy tests and the tests set out in the NPPF when determining relevant planning applications in the period before VALP is adopted. 1.2 The five year housing land supply calculation is dynamic and changes as planning permissions are granted and as existing commitments are completed. Therefore it is important that any developer considering submitting a planning application should consider the latest position on the five year housing supply calculation from the Council. It is intended that the position statement is a living draft that will be regularly updated as the evidence emerges through the Local Plan preparation processes. -
Guidelines for the Use of Rectal Irrigation
CV 412N professional:Layout 1 03/03/2009 10:57 Page 1 Guidelines for the use of Rectal Irrigation (Healthcare Professionals) CV 412N professional:Layout 1 03/03/2009 10:57 Page 2 CV 412N professional:Layout 1 03/03/2009 10:57 Page 3 Preface Dear Colleague It is always a little daunting introducing a new procedure into your clinical practice. There are always questions and some uncertainties. For this reason the bowel continence team at St Mark's Hospital have decided to share their guidelines on rectal irrigation with others. There is too much re-inventing of wheels in today's health service. We are not claiming that this is the last word on irrigation: there is always room for flexibility and adaptation. With experience, our practice may well change and develop over years to come. But for now, this is our clinical practice, which we are happy for you to use and adapt. Feedback or comments would be most welcome. Christine Norton. Burdett Professor of Gastrointestinal Nursing St Marks Hospital, London March 2009 SUPPORTED BY © St Mark's Hospital Continence Service 2009 CV 412N professional:Layout 1 03/03/2009 10:57 Page 4 Background Faecal incontinence is a common health problem, affecting over 1% of community-dwelling adults (1;2). Chronic constipation may affect 3-5% of the population depending on the definition used (3). Most patients will respond to lifestyle modifications (such as dietary modifications), medication (constipating or laxatives as appropriate) and behavioural methods such as pelvic floor muscle training or biofeedback (3;4). But for the minority who do not respond, symptoms may impose severe ongoing restrictions on quality of life. -

Using an Improvement Method to Review Transfers of Care Seven Days a Week
STANDARD 1 STANDARD 2 STANDARD 3 STANDARD 4 STANDARD 5 TIME TO FIRST MULTI- PATIENT CONSULTANT DISCIPLINARY SHIFT ACCESS TO EXPERIENCE REVIEW TEAM REVIEW HANDOVERS DIAGNOSTICS STANDARD 6 STANDARD 7 STANDARD 8 STANDARD 9 STANDARD 10 England TRANSFER TO ACCESS TO COMMUNITY, KEY SERVICES/ MENTAL ONGOING PRIMARY & QUALITY INTERVENTIONS HEALTH REVIEW SOCIAL CARE IMPROVEMENT SEVEN DAY SERVICES CASE STUDY OCT 2015 Aylesbury Vale Clinical Commissioning Group, Chiltern CCG, Buckinghamshire Healthcare NHS Trust and Buckinghamshire County Council Using an improvement method to review transfers of care seven days a week In June 2015, NHS Improving Quality AT A GLANCE: supported Buckinghamshire System • NHS Improving Quality supported Resilience Group (BSRG) to undertake a Buckinghamshire System Resilience ‘snapshot’ review of simple and complex Group (SRG) to review practice at Stoke discharge/transfer of care pathways for Mandeville Hospital in relation to older people admitted as an emergency to meeting standard 9: transfer of care. Stoke Mandeville Hospital (SMH), part of • Buckinghamshire Healthcare Trust (BHT), Buckinghamshire Healthcare NHS Trust. The Buckinghamshire County Council (BCC), work was sponsored by the commissioners and a Aylesbury Vale Clinical Commissioning key driver was to better understand the transfer of Group (AVCCG) and Chiltern CCG co- care issues and identify the focus for new initiatives designed the methodology to identify in preparation for winter pressure planning. where improving access to services may add the most value to inform seven day Since 2013/14, BSRG had implemented a variety of plans. interventions to reduce the demand on urgent care • Information from case note reviews, and to meet urgent and emergency care standards. -

Buckinghamshire and Oxfordshire Summer 2021 3-Month Construction Look Ahead
Buckinghamshire and Oxfordshire Summer 2021 3-month construction look ahead Buckinghamshire and Oxfordshire Summer 2021 This forward look covers HS2 associated work in Buckinghamshire and Oxfordshire. The document includes: • A forward look of construction activities planned in the next three months • Works to be aware of that will take place in the next 12 months, but may not yet have been confirmed The dates and information included in the forward look are subject to change as programme develops. These will be updated in the next edition of the forward look. If you have any queries about the information in this forward look, the HS2 Helpdesk is available all day, every day on 08081 434 434 or by emailing [email protected] Page 2 Buckinghamshire and Oxfordshire Contents Map 1 – Turweston to Mixbury................................................................................................ 4 Map 2 – Finmere to Twyford .................................................................................................... 7 Map 3 – Calvert ....................................................................................................................... 10 Map 4 – Quainton ................................................................................................................... 12 Map 5 – Waddesdon to Stoke Mandeville ............................................................................ 14 Map 6 – Wendover ................................................................................................................. -

Consensus Review of Best Practice of Transanal Irrigation in Children �Giovanni Mosiello, Ydavid Marshall, Zudo Rolle, §Ce´Lia Cre´Tolle, Jjbruno G
INVITED REVIEW Consensus Review of Best Practice of Transanal Irrigation in Children ÃGiovanni Mosiello, yDavid Marshall, zUdo Rolle, §Ce´lia Cre´tolle, jjBruno G. Santacruz, ôJason Frischer, and #Marc A. Benninga See ‘‘Transanal Irrigations: A Few Considerations’’ by What Is Known Ambartsumyan on page 341. Transanal irrigation is an increasingly accepted treat- ment in children with bowel dysfunction who do not ABSTRACT respond to conservative treatments. In recent years, data have been published on the Pediatric patients with either functional or organic bowel dysfunction may efficacy of transanal irrigation in pediatric patient suffer from constipation and fecal incontinence and represent a complex populations such as anorectal malformations and group in whom management is often difficult. Many noninvasive and functional constipation. invasive treatments have been proposed, with variable efficacy and adverse Although the use of transanal irrigation in adults has effects. Transanal irrigation (TAI) is now an accepted alternative, in both been standardized, the practice in children still children and adults, for bowel dysfunction that has not responded to remains largely empirical. conservative and medical therapies. There is, however, still some uncer- tainty about the use of TAI in pediatric populations. Hence, a group of What Is New specialists from different nations and pediatric disciplines, all with long- standing experience of bowel management in children, performed a litera- The first best-practice article based on published ture search and had round table discussions to determine the best-practice evidence and professional experience, aimed at use of TAI in the pediatric patient population. Based on these findings, this healthcare professionals who manage pediatric article provides best-practice recommendations on indications, patient bowel dysfunction and who currently use transanal selection, important considerations before treatment, patient and family irrigation or would like to initiate in its use. -

Abstracts for Posters
303 Spinal holocord epidural abscess evacuated with double thoracic interval laminectomy - A rare case report with literature review Dr Kaustubh Ahuja1, Dr. Laxmana Das1, Dr Aakriti Jain1, Dr. Pankaj Kandwal1, Dr. Shobha Arora1 1All India Institute Of Medical Sciences, Rishikesh Introduction: Spinal epidural abscess is a rare but lethal condition. Its reported incidence ranges from 0.2- 1.2% per 10000 hospital admissions. Holocord Spinal Epidural Space(HSEA) is an even rarer condition associated with high morbidity and mortality.Management for HSEA is controversial and generally includes a thorough surgical decompression with targeted antibiotic therapy. Despite the advances in radiology, antibiotic therapy and surgical techniques mortality rate associated with HSEA is around 15%. This case report describes a novel technique of keystone skip laminectomies at two sites in dorsal spine and surgical decompression with the help of infant feeding tube in a case of HSEA. Methods and Results An 18-year-old previously healthy male presented with high grade fever and low back ache (VAS: 9/10) for 2 weeks and loss of bowel and bladder control for 4 days to our emergency department. There was no history of trauma or any history of drug abuse .Muscle power in bilateral upper limb and lower limb was MRC grade 5. Sensations were intact and reflexes were universally mute. Over the next 24 hours his neurology deteriorated rapidly with complete loss of muscle power in both upper and lower limbs and sensory deficit upto 60 percent in all limbs. MRI showed hyperintense epidural collection extending from C2 to sacral neural foramina with peripheral post contrast enhancement causing anterior displacement of cord. -

This Level Site Is Occupied by a Detached Bungalow Built in the 1920S Which Remains Largely Original
This level site is occupied by a detached bungalow built in the 1920s which remains largely original. There is a drive for this from the A413. Measuring with Promap the land amounts to .9958 acres. Subject to planning there is scope for redevelopment with at least two or three houses but possibly a comprehensive development. Furthermore the gardens of adjoining houses give possible additional development land. The owners of 123 Wendover Road have instructed Christopher Pallet to seek proposals for their property as a separate transaction. The verge to the south of Arnold Close has been retained by the developers and could provide a potential further access. Please discuss with us. With a view to encouraging applicants to submit attractive offers the Executors are not intending to apply an uplift clause or ransom strip along the boundary with 123 Wendover Road. However they may decide to include such provision if offers do not meet their expectations. A ransom strip will be retained along the rear boundary. One Acre of Potential Building Land 121 Wendover Road, Stoke Mandeville, Aylesbury, Buckinghamshire HP22 5TD GUIDE PRICE £650,000 Chartered Surveyors Location Services The site fronts the A413 Wendover Road on the outskirts The existing bungalow is connected to water and electricity. of the village of Stoke Mandeville some 2¼ miles from All services are believed to be available in Wendover the centre of the County Town of Aylesbury and Road and Arnold Close. 2½ miles from the small town of Wendover. Stoke No enquiries as to the capacity and availability of Mandeville is a medium size village with a local shop/ services have been made. -

Transanal Irrigation for Neurogenic Bowel Disease, Low Anterior Resection Syndrome, Faecal Incontinence and Chronic Constipation: a Systematic Review
Journal of Clinical Medicine Review Transanal Irrigation for Neurogenic Bowel Disease, Low Anterior Resection Syndrome, Faecal Incontinence and Chronic Constipation: A Systematic Review Mira Mekhael 1,2,3,*, Helle Ø Kristensen 1,2, Helene Mathilde Larsen 1,2,3 , Therese Juul 1,2,3 , Anton Emmanuel 4, Klaus Krogh 2,5 and Peter Christensen 1,2,3 1 Department of Surgery, Aarhus University Hospital, DK8200 Aarhus, Denmark; [email protected] (H.Ø.K.); [email protected] (H.M.L.); [email protected] (T.J.); [email protected] (P.C.) 2 Danish Cancer Society Centre for Research on Survivorship and Late Adverse Effects after Cancer in the Pelvic Organs, DK8200 Aarhus, Denmark; [email protected] 3 Department of Clinical Medicine, Aarhus University, DK8200 Aarhus, Denmark 4 GI Physiology Unit, University College London Hospital, London NW1 2BU, UK; [email protected] 5 Department of Hepatology and Gastroenterology, Aarhus University Hospital, DK8200 Aarhus, Denmark * Correspondence: [email protected] Abstract: Transanal irrigation (TAI) has received increasing attention as a treatment option in patients with bowel dysfunction. This systematic review was conducted according to the PRISMA guidelines and evaluates the effect of TAI in neurogenic bowel dysfunction (NBD), low anterior resection syndrome (LARS), faecal incontinence (FI) and chronic constipation (CC). The primary outcome was the effect of TAI on bowel function. Secondary outcomes included details on TAI, quality of life (QoL), the discontinuation rate, adverse events, predictive factors for a successful outcome, and Citation: Mekhael, M.; Kristensen, health economics. A systematic search for articles reporting original data on the effect of TAI on H.Ø; Larsen, H.M.; Juul, T.; bowel function was performed, and 27 eligible studies including 1435 individuals were included. -
Download Original Attachment
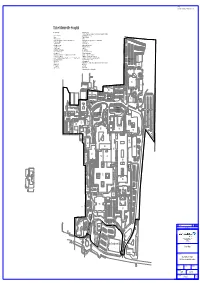
NOTES: Do not scale from drawing. Check all dimensions on site. Stoke Mandeville Hospital Building No. Legend 73 Haematology Dept. 74 Health Care Safety Team, Occupational Health, Backcare Safety Advisors & Finance 2. Gardeners Workshop 75 National Spinal Injuries Center 3 Empty 77 Man Med Pharmacy 29 Pathology Laboratories 79 Empty 36 Estates Dept. Workshops, General Stores & Sodexo Hard Services 80 Sodexo Soft Services, Property Services, General Administration 37 Estates Dept. Offices. 81 X-Ray Extension 41 Hydrotherapy Pool 83 Pathology Extension 48 Occupational Therapy 84 Florence Nightingale Hospice 49 Occupational Annex 85 Outpatients Extension 54 Floyd Auditorium 86 Maternity 55 David Brown Hall of Residence 86B Maternity Pod 56 Duke of Edinburgh Lounge 88 Day Nursery (Private Owned) 57 Ophthalmic Unit 89 Cancer Care Hematology 67 John Hampden Unit (Oxfordshire, Buckinghamshire Mental Health Trust) 90 Aston House Doctors Accommodation 68 Trust Management Offices 91 Main Entrance, Catering & Administration (PFI) 69 A & E, ITU, Out Patients, Theatres, Wards 11, 12, 20, 21, 22, 23, X-Ray Phase 1, IT 92 Wards 1 - 9, Pharmacy, Day Surgery, Endoscopy (PFI) Dept. & Clinical Administration 93 Ward 10, Medical Records & Mortuary Willows Car 69A Service Tower 94 ADL Bungalow (PFI) Park 69B Service Tower 95 Mandeville Wing - Ophthalmic Theatres, Ophthalmic Outpatinets, Ward 14 & General 70 Energy Center Administration 71 Transport Dept. 96 Renal Unit 72 Sterile Services H1 Pharmacy QC R6 Harrington House Student Accommodation Aston House -

BUCKINGHAMSHIRE POSSE COMITATUS 1798 the Posse Comitatus, P
THE BUCKINGHAMSHIRE POSSE COMITATUS 1798 The Posse Comitatus, p. 632 THE BUCKINGHAMSHIRE POSSE COMITATUS 1798 IAN F. W. BECKETT BUCKINGHAMSHIRE RECORD SOCIETY No. 22 MCMLXXXV Copyright ~,' 1985 by the Buckinghamshire Record Society ISBN 0 801198 18 8 This volume is dedicated to Professor A. C. Chibnall TYPESET BY QUADRASET LIMITED, MIDSOMER NORTON, BATH, AVON PRINTED IN GREAT BRITAIN BY ANTONY ROWE LIMITED, CHIPPENHAM, WILTSHIRE FOR THE BUCKINGHAMSHIRE RECORD SOCIETY CONTENTS Acknowledgments p,'lge vi Abbreviations vi Introduction vii Tables 1 Variations in the Totals for the Buckinghamshire Posse Comitatus xxi 2 Totals for Each Hundred xxi 3-26 List of Occupations or Status xxii 27 Occupational Totals xxvi 28 The 1801 Census xxvii Note on Editorial Method xxviii Glossary xxviii THE POSSE COMITATUS 1 Appendixes 1 Surviving Partial Returns for Other Counties 363 2 A Note on Local Military Records 365 Index of Names 369 Index of Places 435 ACKNOWLEDGMENTS The editor gratefully acknowledges the considerable assistance of Mr Hugh Hanley and his staff at the Buckinghamshire County Record Office in the preparation of this edition of the Posse Comitatus for publication. Mr Hanley was also kind enough to make a number of valuable suggestions on the first draft of the introduction which also benefited from the ideas (albeit on their part unknowingly) of Dr J. Broad of the North East London Polytechnic and Dr D. R. Mills of the Open University whose lectures on Bucks village society at Stowe School in April 1982 proved immensely illuminating. None of the above, of course, bear any responsibility for any errors of interpretation on my part.