Best Practices in Long-Term Care Management of Pressure Injuries Working Together Towards Excellence in Resident Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
District Name
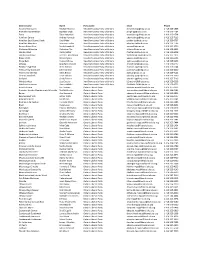
District name Name Party name Email Phone Algoma-Manitoulin Michael Mantha New Democratic Party of Ontario [email protected] 1 416 325-1938 Bramalea-Gore-Malton Jagmeet Singh New Democratic Party of Ontario [email protected] 1 416 325-1784 Essex Taras Natyshak New Democratic Party of Ontario [email protected] 1 416 325-0714 Hamilton Centre Andrea Horwath New Democratic Party of Ontario [email protected] 1 416 325-7116 Hamilton East-Stoney Creek Paul Miller New Democratic Party of Ontario [email protected] 1 416 325-0707 Hamilton Mountain Monique Taylor New Democratic Party of Ontario [email protected] 1 416 325-1796 Kenora-Rainy River Sarah Campbell New Democratic Party of Ontario [email protected] 1 416 325-2750 Kitchener-Waterloo Catherine Fife New Democratic Party of Ontario [email protected] 1 416 325-6913 London West Peggy Sattler New Democratic Party of Ontario [email protected] 1 416 325-6908 London-Fanshawe Teresa J. Armstrong New Democratic Party of Ontario [email protected] 1 416 325-1872 Niagara Falls Wayne Gates New Democratic Party of Ontario [email protected] 1 416 212-6102 Nickel Belt France GŽlinas New Democratic Party of Ontario [email protected] 1 416 325-9203 Oshawa Jennifer K. French New Democratic Party of Ontario [email protected] 1 416 325-0117 Parkdale-High Park Cheri DiNovo New Democratic Party of Ontario [email protected] 1 416 325-0244 Timiskaming-Cochrane John Vanthof New Democratic Party of Ontario [email protected] 1 416 325-2000 Timmins-James Bay Gilles Bisson -

“Doug Ford Has Been Ducking Work and Ducking Accountability.”
Queen’s Park Today – Daily Report March 11, 2019 Quotation of the day “Doug Ford has been ducking work and ducking accountability.” NDP MPP Catherine Fife criticizes the premier for being MIA in question period more than half of the time since December. Today at Queen’s Park On the schedule MPPs are in their ridings for the March Break constituency week. The House is adjourned until Monday, March 18. Premier watch This weekend Premier Doug Ford hit up a youth-focused roundtable discussion with Mississauga-Malton MPP Deepak Anand and visited IBM Canada’s headquarters in Markham. Ford trumpeted his government’s work to make Ontario “open for business” and “life more affordable for university and college students” on his social media feeds. But NDP MPP Catherine Fife says the premier has been “ducking work and ducking accountability” over the Ron Taverner controversy, pointing out Ford was MIA for 11 of 18 question periods since December. Meanwhile the premier’s office points out official Opposition Leader Andrea Horwath has skipped out on question period in about equal proportion over the last session. Global News breaks down the details. Hydro One executive salary will be capped at $1.5M Ontario’s PC government has won a standoff with Hydro One over executive pay. The provincial utility said Friday it agreed to cap its next boss’ direct compensation at $1.5 million, which includes a $500,000 base salary and up to $1 million in bonuses for hitting certain short- and long-term benchmarks. The salaries of other board members will be limited to 75 per cent of what the next CEO rakes in. -

Government of Ontario Key Contact Ss
GOVERNMENT OF ONTARIO 595 Bay Street Suite 1202 Toronto ON M5G 2C2 KEY CONTACTS 416 586 1474 enterprisecanada.com PARLIAMENTARY MINISTRY MINISTER DEPUTY MINISTER PC CRITICS NDP CRITICS ASSISTANTS Steve Orsini Patrick Brown (Cabinet Secretary) Steve Clark Kathleen Wynne Andrea Horwath Steven Davidson (Deputy Leader + Ethics REMIER S FFICE Deb Matthews Ted McMeekin Jagmeet Singh P ’ O (Policy & Delivery) and Accountability (Deputy Premier) (Deputy Leader) Lynn Betzner Sylvia Jones (Communications) (Deputy Leader) Lorne Coe (Post‐Secondary ADVANCED EDUCATION AND Han Dong Peggy Sattler Education) Deb Matthews Sheldon Levy Yvan Baker Taras Natyshak SKILLS DEVELOPMENT Sam Oosterhoff (Digital Government) (Digital Government) +DIGITAL GOVERNMENT (Digital Government) AGRICULTURE, FOOD AND RURAL AFFAIRS Jeff Leal Deb Stark Grant Crack Toby Barrett John Vanthof +SMALL BUSINESS ATTORNEY GENERAL Yasir Naqvi Patrick Monahan Lorenzo Berardinetti Randy Hillier Jagmeet Singh Monique Taylor Gila Martow (Children, Jagmeet Singh HILDREN AND OUTH ERVICES Youth and Families) C Y S Michael Coteau Alex Bezzina Sophie Kiwala (Anti‐Racism) Lisa MacLeod +ANTI‐RACISM Jennifer French (Anti‐Racism) (Youth Engagement) Jennifer French CITIZENSHIP AND IMMIGRATION Laura Albanese Shirley Phillips (Acting) Shafiq Qaadri Raymond Cho Cheri DiNovo (LGBTQ Issues) Lisa Gretzky OMMUNITY AND OCIAL ERVICES Helena Jaczek Janet Menard Ann Hoggarth Randy Pettapiece C S S (+ Homelessness) Matt Torigian Laurie Scott (Community Safety) (Community Safety) COMMUNITY SAFETY AND Margaret -

October 11, 2007
The Cord WeeklyThe tie that binds since 1926 SILENT SYMPHONY GEMUETLICHKEIT Why students ignore our music The Hawks take on Guelph A brief introduction to KW's PAGES 14-15 department... ... Gryphons PAGE 10 Oktoberfest bash ... PAGE 10 Volume 48 Issue 9 THURSDAY OCTOBER 11, 2007 www.cordweekly.com Witmer, McGuinty re-elected Conservative incumbent Elizabeth Witmer re-elected to lengthen extensive political career; Liberals retain majority government DAN POLISCHUK official, Witmertip-toed around the NEWS EDITOR subject. "I've had the real pleasure of While her party may have lost the serving with John Tory," answered election overall, long-time Con- the current deputy leader. servative Party member Elizabeth "Well see what the future holds." Witmer came out a winner in more Upon arrival at her victory cel- ways than one. ebration at the Waterloo Inn, Wit- With CTV declaring a majority mer was met by a boisterous group government for Dalton McGuinty's of supporters, many of whom she Liberals by 9:30 pm, just a half hour acknowledged in her speech. later it was determined thatWitmer, "I want to thank, from the bottom an MPP for the riding ofKitchener- ofmy heart, thevoters ofKitchener- Waterloo for the last 17 years, had Waterloo for the faith, confidence secured another four years in the and trust you have, again, placed in Ontario legislature. me," saidWitmer, adding, "I believe At press time, with 250 out of 301 we have improved the quality oflife held polls reporting, Witmer 40% ... for everyone in this community." of the overall vote (16,004) - which "I'm ecstatic that the voters have was a nine point lead over Louise seen fit to re-elect me one more Ervin of the Liberals, with 12,276 time and have expressed that level votes. -
Annual-Report-2020-Final.Pdf
The Ontario Society of Professional Engineers The Ontario Society of Professional Engineers (OSPE) is the voice of the engineering profession in Ontario. We represent the entire engineering community, including professional engineers, engineering graduates and students who work or will work in several of the most strategic and influential sectors of Ontario’s economy. OSPE elevates the profile of the profession by advocating to government, offering valued member services and providing opportunities for ongoing learning, networking and community building. 2019 Annual Report OSPE’s 2019 Annual Report provides an overview of the association’s work and impact on behalf of Ontario’s engineering community from January 1 through December 31, 2019. This report was prepared for distribution at OSPE’s Annual General Meeting on May 6, 2020 and outlines how the organization’s initiatives and activities met the tactical goals laid out in Engineering the Future Together, our 2019-2022 Strategic Plan. Table of Contents Pg. 3 2019-2020 Board of Directors Pg. 4 Messages from the CEO and the President & Chair Pg. 6 Engineering the Future Together Pg. 7 Ambassador Program Pg. 8 Year in Review Pg. 16 Events: Uniting the Community Pg. 20 17th Annual Claudette MacKay-Lassonde Forum: #ItsTimeWeBuild Pg. 22 The EDI Imperative: Changing the Profile of STEAM in Canada Pg. 24 OSPE Exchange Hubs Pg. 26 Government Programs Pg. 28 Social Media Impressions Pg. 30 Financial Statements Pg. 34 Partners Pg. 35 Looking Forward 2 OSPE 2019 Annual Report 2019-2020 Board of Directors Back row, left to right Tom Murad, P.Eng. (Director), Jim Chisholm, P.Eng. -

Ontario Government Quick Reference Guide: Key Officials and Opposition Critics August 2014
Ontario Government Quick Reference Guide: Key Officials and Opposition Critics August 2014 Ministry Minister Chief of Staff Parliamentary Assistant Deputy Minister PC Critic NDP Critic Hon. David Aboriginal Affairs Milton Chan Vic Dhillon David de Launay Norm Miller Sarah Campbell Zimmer Agriculture, Food & Rural Affairs Hon. Jeff Leal Chad Walsh Arthur Potts Deb Stark Toby Barrett N/A Hon. Lorenzo Berardinetti; Sylvia Jones (AG); Jagmeet Singh (AG); Attorney General / Minister responsible Shane Madeleine Marie-France Lalonde Patrick Monahan Gila Martow France Gélinas for Francophone Affairs Gonzalves Meilleur (Francophone Affairs) (Francophone Affairs) (Francophone Affairs) Granville Anderson; Alexander Bezzina (CYS); Jim McDonell (CYS); Monique Taylor (CYS); Children & Youth Services / Minister Hon. Tracy Omar Reza Harinder Malhi Chisanga Puta-Chekwe Laurie Scott (Women’s Sarah Campbell responsible for Women’s Issues MacCharles (Women’s Issues) (Women’s Issues) Issues) (Women’s Issues) Monte Kwinter; Cristina Citizenship, Immigration & International Hon. Michael Christine Innes Martins (Citizenship & Chisanga Puta-Chekwe Monte McNaughton Teresa Armstrong Trade Chan Immigration) Cindy Forster (MCSS) Hon. Helena Community & Social Services Kristen Munro Soo Wong Marguerite Rappolt Bill Walker Cheri DiNovo (LGBTQ Jaczek Issues) Matthew Torigian (Community Community Safety & Correctional Hon. Yasir Brian Teefy Safety); Rich Nicholls (CSCS); Bas Balkissoon Lisa Gretzky Services / Government House Leader Naqvi (GHLO – TBD) Stephen Rhodes (Correctional Steve Clark (GHLO) Services) Hon. David Michael Government & Consumer Services Chris Ballard Wendy Tilford Randy Pettapiece Jagmeet Singh Orazietti Simpson Marie-France Lalonde Wayne Gates; Economic Development, Employment & Hon. Brad (Economic Melanie Wright Giles Gherson Ted Arnott Percy Hatfield Infrastructure Duguid Development); Peter (Infrastructure) Milczyn (Infrastructure) Hon. Liz Education Howie Bender Grant Crack George Zegarac Garfield Dunlop Peter Tabuns Sandals Hon. -

Student Alliance
ONTARIO UNDERGRADUATE STUDENT ALLIANCE ADVOCACY CONFERENCE 2020 November 16-19th ABOUT OUSA The Ontario Undergraduate Student Alliance (OUSA) represents the interests of approximately 150,000 professional and undergraduate, full-time and part-time university students at eight student associations across Ontario. Our vision is for an accessible, affordable, accountable and high quality post-secondary education in Ontario. OUSA’s approach to advocacy is based on creating substantive, student driven, and evidence-based policy recommendations. INTRODUCTION Student leaders representing over 150,000 undergraduate students from across Ontario attended OUSA’s annual Student Advocacy Conference from November 16th to the 19th. Delegates met with over 50 MPPs from four political parties and sector stakeholders to discuss the future of post-secondary education in Ontario and advance OUSA’s advocacy priorities. Over five days, the student leaders discussed student financial aid, quality of education, racial equity, and student mental health. As we navigate the global pandemic, OUSA recommends improvements to the Ontario Student Assistance Program (OSAP), guidance and support for quality online learning, training and research to support racial equity, and funding for student mental health services. Overall, OUSA received a tremendous amount of support from members and stakeholders. ATTENDEES Julia Periera (WLUSU) Eric Chappell (SGA-AGÉ) Devyn Kelly (WLUSU) Nathan Barnett (TDSA) Mackenzy Metcalfe (USC) Rayna Porter (TDSA) Matt Reesor (USC) Ryan Tse (MSU) Megan Town (WUSA) Giancarlo Da-Ré (MSU) Abbie Simpson (WUSA) Tim Gulliver (UOSU-SÉUO) Hope Tuff-Berg (BUSU) Chris Yendt (BUSU) Matthew Mellon (AMS) Alexia Henriques (AMS) Malek Abou-Rabia (SGA-AGÉ) OUSA MET WITH A VARIETY OF STAKEHOLDERS MPPS CABINET MINISTERS Minister Michael Tibollo MPP Stephen Blais Office of Minister Monte McNaughton MPP Jeff Burch Office of Minister Peter Bethlenfalvy MPP Teresa Armstrong . -

Are Doin' It for Themselves” Is the Union Density Is Comprised of Women, and of Name of a 1985 Hit Duet Recorded by Aretha Franklin People of Colour
ARE DOIN’ IT FOR THEMSELVES A Report from the OFL Women’s Summit Sisters By Ashmeela Ahmad ROM DECEMBER 10 TO 12, 2012, THE Ontario Federation of Labour’s Women’s Leadership Summit was held at the Kempenfelt Conference Centre in Barrie, Ontario. Union sisters came from all walks of life, and included those who work in Fgovernment, manufacturing, administration, the service industry, health care and education. They reflected different equity groups, rich in both diver- sity and ethnicity, and in age ranges and life expe- riences. Some were experienced union women, and HUTCHISON NANCY PHOTOGRAPHS: others, like me, were new to the movement. It was empowering and enlightening to meet so many eager women activists. Not only was it a safe space in which to express ourselves, but we had carte blanche to discuss women’s issues, without censure or fear of paternalism. from the Ontario Secondary School Teachers Discussions focussed on key questions affecting Federation (OSSTF), presented the findings of the women activists in leadership union positions, and study “Leadership, Feminism & Equality in Unions the challenges they experience in the struggle for in Canada.” (See page 30.) Ontario Health Coalition equality, against the current economic, political and director Natalie Mehra presented findings from social backdrop. Some of the questions were: “Falling Behind: A Report of the Ontario Common • Do women’s structures (e.g. committees) still Front 2012.” Katie Arnup, from the Ontario work? Coalition for Better Child Care, spoke about “We • How do we support women leaders? Are Ontario” (www.weareontario.ca), a labour- and • Is there a war on women in Harper’s Canada? community-based campaign launched by the • What can we do to encourage women’s Ontario Common Front, a coalition of over 90 committees to become organizing centres for community groups and unions in Ontario. -

“The Moose in the Room.”
Queen’s Park Today – Daily Report April 5, 2019 Quotation of the day “The moose in the room.” Treasury Board President Peter Bethlenfalvy wore a moose-printed tie to illustrate the “Canadian version” of the “elephant in the room” in a speech about Ontario’s public sector compensation spending. Today at Queen’s Park On the schedule The House convenes Monday at 10:30 a.m. for question period. Thursday’s debates and proceedings Two backbench bills passed and a motion failed during the afternoon’s private members’ business debates: ● NDP MPP Rima Berns-McGown’s Bill 83, Day of Remembrance and Action on Islamophobia Act, is off to the social policy committee; ● PC MPP Roman Baber’s Bill 84, Prohibiting Hate-Promoting Demonstrations at Queen’s Park Act, was sent to the Standing Committee on Justice Policy; and ● NDP MPP Laura Mae Lindo’s motion, calling on the government to commit to funding and a timeline for two-way, all-day GO train service along the Kitchener corridor, failed (Ayes 22; Nays 51). In the park A pop-up safe injection site was set up on the Queen’s Park lawn by the Toronto Overdose Prevention Society, as advocates demonstrated against the government’s funding cuts to some sites. Students at hundreds of high schools across the province staged a walkout in protest of the government’s education changes, with many turning up at Queen’s Park. Tories eyeing caps on public-sector wage hikes Treasury Board President Peter Bethlenfalvy fired a shot across the bows of public-sector unions, saying the government may cap their members’ wage increases as it looks to trim the deficit. -
Glp Weekly Times a U G U S T 2 7 , 2 0 2 1 | V O L U M E 1 5 , I S S U E 2 9
GLP WEEKLY TIMES A U G U S T 2 7 , 2 0 2 1 | V O L U M E 1 5 , I S S U E 2 9 PEO 2019 - 2020 President Nancy Hill, P.Eng. (left) spoke about the PEO Government Liasion Program (GLP) in an interview on August 20. Here she is with CEO/Registrar Johnny Zuccon, P.Eng. (right), at a meeting with Attorney General Doug Downey, MPP (Barrie—Springwater—Oro-Medonte) (centre), in 2019. F0RMER PEO PRESIDENT SHARES HER THOUGHTS ON THE GOVERNMENT LIAISON PROGRAM PEO 2019 - 2020 President Nancy Hill, P .Eng. had an WHAT'S INSIDE exclusive interview with the GLP Weekly Times on Meet your MPP...2 August 20. She spoke about her experience with the GLP and opportunities for the program. PEO Lake Ontario Chapter Explains PEO's Regulatory For more on this story, see pages 4,5 and 6. Role to MPP...3 1 MEET YOUR MPP This week, the GLP Weekly Times features Prabmeet Singh Sarkaria, MPP (Brampton South), President of the Treasury Board and Catherine Fife, MPP (Waterloo), NDP Finance and Treasury Board Critic Prabmeet Singh Sarkaria (left) is the MPP for Brampton South and is the President of the Treasury Board. Here he is with Brampton Chapter GLP Chair Ravinder Panesar, P.Eng., (centre right) Transportation Minister Caroline Mulroney, MPP (York-Simcoe) (centre left) and Amarjot Sandhu, MPP (Brampton West), Parliamentary Assistant to the Minister of Infrastructure (right) at a Brampton Board of Trade event in 2019. PRABMEET SINGH SARKARIA, MPP Minister Sarkaria was elected to the Ontario Legislature in 2018 as a Progressive Conservative. -

Best Practice Spotlight Organizations Celebrate 10 Years of Nursing Innovation Thatmakes Evidence-Based Practice Apriority
PRIL 2013 A MARCH/ JOURNAL ON Best Practice Spotlight Organizations celebrate 10 years of nursing innovation that makes evidence-based practice a priority. The unique challenges of rural nursing • Taking Queen’s Park Day “on the road” RNAO celebrates 10 GREAT YEARS with BPSOs BPSO® ORGANIZATIONS Australian Nursing and Midwifery Federation, RNAO congratulates SA Branch (Host Site-3) Baycrest Centre for Geriatric Care its leading edge BPSOs and the Bayshore Home Health thousands of nurses and health- Bluewater Health Cambridge Memorial Hospital care professionals who have led CBI Home Health the way over the past 10 years to Centre for Addiction and Mental Health Chatham-Kent Health Alliance enhance evidence-based practice Clinica Las Condes, Chile for the benet of Ontarians. Escuela De Enfermeria, Facultad De Medicina, Universidad De Chile, Chile Mackenzie Health Thunder Bay District Health Unit FOSCAL Fundación Oftalmológica de Santander – Colombia Mount Sinai Hospital Thunder Bay Regional Health Sciences Centre Grand River Hospital Niagara Health System Toronto Public Health Grey Bruce Health Unit Niagara Region Public Health Trent University Guelph General Hospital North Bay Nurse Practitioner-Led Clinic Trillium Health Partners Hamilton Health Sciences Centre Ontario Telemedecine Network Two Rivers Family Health Team Health Sciences North Red Cross Care Partners Universidad de Investigacion en Cuidados de Salud (Investen-isciii) del Instituto de Salud HNHB Community Care Access Centre Royal Victoria Hospital Carlos III (Host Site-8) HNHB Local Health Integrated Network Saint Elizabeth Health Care University Health Network Holland Bloorview Kids Rehab St. Joseph's Health Care, London University of Hartford, USA Hospital Cardio Infantil, Colombia St. -

The Shortened Fall Legislative Session Brought a Much Welcome Change in Tone, However, the Song Remains the Same.”
Queen’s Park Today – Daily Report December 12, 2019 Quotation of the day “The shortened fall legislative session brought a much welcome change in tone, however, the song remains the same.” Liberal Interim Leader John Fraser bids adieu to the 2019 fall session. Today at Queen’s Park On the schedule It’s the final sitting day before the winter recess; MPPs are slated to return February 18, 2020. The house convenes at 9 a.m. The government could call any of the following bills for second-reading debate: ● Bill 156, Security From Trespass and Protecting Food Safety Act; ● Bill 161, Smarter and Stronger Justice Act; and ● Bill 167, Legislative Assembly Amendment Act. Bill 159, Rebuilding Consumer Confidence Act, bypassed second reading thanks to a rarely used standing order (74(a)). The Tarion reform bill will be studied by the justice committee in a closed session this afternoon and for up to five days over the winter break. Two bills and one motion are on the docket for this afternoon’s private members’ business debates: ● NDP Transportation critic Jessica Bell will put forward her (non-binding) motion calling on the government to match municipal funding for public transit operations and maintenance; ● NDP MPP Catherine Fife will move second reading of Bill 153, Till Death Do Us Part Act, which would enshrine the right for spouses to live together in a nursing home; and ● PC MPP Belinda Karahalios will call second reading on her bill to beef up accountability for political party nominations and executive elections, Bill 150, Ensuring Transparency and Integrity in Political Party Elections Act.