A Basic Approach to Common Upper Extremity Mononeuropathies and Brachial Plexopathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys
SCIENTIFIC ARTICLES Stomatologija, Baltic Dental and Maxillofacial Journal, 5:44-47, 2003 Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys SUMMARY Aim and purpose of the study were: 1) to study and compare unfavorable factors playing role in the development of upper teeth plexitis and upper teeth plexopathy; 2) to study peculiarities of clinical manifestation of upper teeth plexitis and upper teeth plexopathy, and to establish their diagnostic value; 3) to optimize the treatment. The results of examination and treatment of 79 patients with upper teeth plexitis (UTP-is) and 63 patients with upper teeth plexopathy (UTP-ty) are described in the article. Questions of the etiology, pathogenesis and differential diagnosis are discussed, methods of complex medicamental and surgical treatment are presented. Keywords: atypical facial neuralgia, atypical odontalgia, atypical facial pain, vascular toothache. PREFACE Besides the common clinical tests, in order to ana- lyze in detail the etiology and pathogenesis of the afore- Usually the injury of the trigeminal nerve is re- mentioned disease, its clinical manifestation and pecu- lated to the pathology of the teeth neural plexuses. liarities, we performed specific examinations such as According to the literature data, injury of the upper orthopantomography of the infraorbital canals, mea- teeth neural plexuses makes more than 7% of all sured the velocity of blood flow in the infraorbital blood neurostomatologic diseases. Many terms are used in vessels (doplerography), examined the pain threshold literature to characterize the clinical symptoms com- of facial skin and oral mucous membrane in acute pe- plex of the above-mentioned pathology. Some authors riod and remission, and evaluated the role that the state (1, 2, 3) named it dental plexalgia or dental plexitis. -

An Occupational Therapy Guide for Entry
University of North Dakota UND Scholarly Commons Occupational Therapy Capstones Department of Occupational Therapy 2008 An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries Ryan Edwards University of North Dakota Follow this and additional works at: https://commons.und.edu/ot-grad Part of the Occupational Therapy Commons Recommended Citation Edwards, Ryan, "An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries" (2008). Occupational Therapy Capstones. 57. https://commons.und.edu/ot-grad/57 This Scholarly Project is brought to you for free and open access by the Department of Occupational Therapy at UND Scholarly Commons. It has been accepted for inclusion in Occupational Therapy Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. AN OCCUPATIONAL THERAPY GUIDE FOR ENTRY-LEVEL THERAPISTS NOT SPECIALIZING IN THE TREATMENT OF UPPER EXTREMITY DYSFUNCTION: THREE COMMON CUMULATIVE TRAUMA INJURIES by Ryan Edwards Advisor: Anne Haskins PhD, OTR/L A Scholarly Project Submitted to the Occupational Therapy Department of the University of North Dakota In partial fulfillment of the requirements for the degree of Master’s of Occupational Therapy Grand Forks, North Dakota August 1, 2008 This Scholarly Project Paper, submitted by Ryan Edwards in partial fulfillment of the requirement for the Degree of Master’s of Occupational Therapy from the University of North Dakota, has been read by the Faculty Advisor under whom the work has been done and is hereby approved. -

Brachial-Plexopathy.Pdf
Brachial Plexopathy, an overview Learning Objectives: The brachial plexus is the network of nerves that originate from cervical and upper thoracic nerve roots and eventually terminate as the named nerves that innervate the muscles and skin of the arm. Brachial plexopathies are not common in most practices, but a detailed knowledge of this plexus is important for distinguishing between brachial plexopathies, radiculopathies and mononeuropathies. It is impossible to write a paper on brachial plexopathies without addressing cervical radiculopathies and root avulsions as well. In this paper will review brachial plexus anatomy, clinical features of brachial plexopathies, differential diagnosis, specific nerve conduction techniques, appropriate protocols and case studies. The reader will gain insight to this uncommon nerve problem as well as the importance of the nerve conduction studies used to confirm the diagnosis of plexopathies. Anatomy of the Brachial Plexus: To assess the brachial plexus by localizing the lesion at the correct level, as well as the severity of the injury requires knowledge of the anatomy. An injury involves any condition that impairs the function of the brachial plexus. The plexus is derived of five roots, three trunks, two divisions, three cords, and five branches/nerves. Spinal roots join to form the spinal nerve. There are dorsal and ventral roots that emerge and carry motor and sensory fibers. Motor (efferent) carries messages from the brain and spinal cord to the peripheral nerves. This Dorsal Root Sensory (afferent) carries messages from the peripheral to the Ganglion is why spinal cord or both. A small ganglion containing cell bodies of sensory NCS’s sensory fibers lies on each posterior root. -

Study of Brachial Plexus with Regards to Its Formation, Branching Pattern and Variations and Possible Clinical Implications of Those Variations
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 4 Ver. VII (Apr. 2016), PP 23-28 www.iosrjournals.org Study of Brachial Plexus With Regards To Its Formation, Branching Pattern and Variations and Possible Clinical Implications of Those Variations. Dr. Shambhu Prasad1, Dr. Pankaj K Patel2 1 (Assistant Professor , Department of Anatomy , NMCH , Sasaram , India ) 2 (Assistant Professor , Department of Pathology , NMCH , Sasaram , India ) Abstract: Aim of the study: to search variations in formation and branching pattern of brachial plexus and correlate them with possible clinical and surgical implications. Materials and Methods: 25human bodies were dissected for this study. Dissection was started in posterior triangle of neck and extended to distal part of upper limb passing through axilla . Photographs were taken and data was tabulated and analyzed . Observations: All 50 plexuses had origin from C5 – T1 . Dorsal scapular nerve was absent in 2 plexuses. Long thoracic nerve was made of C5,C6 fibers in one and of C6,C7 fibers in another . Lower trunk was abnormal in 2 plexuses both of same body, their was no contribution from T1 fibers to posterior cord in one of these plexus. One plexus had double lateral pectoral nerve , communication between lateral and medial pectoral nerves , lateral pectoral and medial root of median nerve also between musculocutaneous and lateral root of median nerve . 2 more plexuses had communication between lateral and medial pectoral nerves. One plexus showed 2 branches coming from posterior division of upper trunk itself before formation of posterior cord. -

Morphology of Extensor Indicis Proprius Muscle in the North Indian Region: an Anatomy Section Anatomic Study with Ontogenic and Phylogenetic Perspective
DOI: 10.7860/IJARS/2019/41047:2477 Original Article Morphology of Extensor Indicis Proprius Muscle in the North Indian Region: An Anatomy Section Anatomic Study with Ontogenic and Phylogenetic Perspective MEENAKSHI KHULLAR1, SHERRY SHARMA2 ABSTRACT to the index finger were noted and appropriate photographs Introduction: Variants on muscles and tendons of the forearm were taken. or hand occur frequently in human beings. They are often Results: In two limbs, the EIP muscle was altogether absent. discovered during routine educational cadaveric dissections In all the remaining 58 limbs, the origin of EIP was from the and surgical procedures. posterior surface of the distal third of the ulnar shaft. Out of Aim: To observe any variation of Extensor Indicis Proprius (EIP) these 58 limbs, this muscle had a single tendon of insertion in 52 muscle and to document any accessory muscles or tendons limbs, whereas in the remaining six limbs it had two tendinous related to the index finger. slips with different insertions. Materials and Methods: The EIP muscle was dissected in 60 Conclusion: Knowledge of the various normal as well as upper limb specimens. After reflection of the skin and superficial anomalous tendons on the dorsal aspect of the hand is fascia from the back of the forearm and hand, the extensor necessary for evaluating an injured or diseased hand and also at retinaculum was divided longitudinally and the dorsum of the the time of tendon repair or transfer. Awareness of such variants hand was diligently dissected. The extensor tendons were becomes significant in surgeries in order to avoid damage to the delineated and followed to their insertions. -

Bilateral Presence of a Variant Subscapularis Muscle
CASE REPORT Bilateral presence of a variant subscapularis muscle Krause DA and Youdas JW Krause DA, Youdas JW. Bilateral presence of a variant subscapularis the lateral subscapularis inserting into the proximal humerus with the tendon of muscle. Int J Anat Var. 2017;10(4):79-80. the subscapularis. The axillary and lower subscapular nerves coursed between the observed muscle and the subscapularis. The presence of the muscle has potential ABSTRACT to entrap the axillary nerve and the lower subscapular nerve. We describe the presence of an accessory subscapularis muscle observed bilaterally Key Words: Accessory subscapularis; Axillary nerve; Lower subscapular nerve; in a human anatomy laboratory. The muscle originated from the mid-region of Entrapment INTRODUCTION everal anatomic variations in axillary musculature have been reported (1- S4). One of the more common variations is the axillary arch muscle, also known as Langer’s muscle, the axillopectoral muscle, and the pectordorsal muscle (3,4). This muscle typically arises from the lateral aspect of the latissimus dorsi inserting deep to the pectoralis major on the humerus. Several variations of the axillary arch muscle are described with a reported incidence of 6-9% (4-6). Less frequent and distinctly different than the axillary arch muscle, is a variant muscle associated with the subscapularis. This has been termed the subscapulo-humeral muscle, subscapularis minor, subscapularis-teres-latissimus muscle, and the accessory subcapularis muscle (1,2,7). Reported incidence ranges from 0.45 to 2.6% (2,7). CASE REPORT A variant muscle associated with the subscapularis bilaterally was observed on a Caucasian female embalmed cadaver during routine dissection in a human anatomy class for first year physical therapy students. -

Coonrad/Morrey Total Elbow Surgical Technique
Zimmer Coonrad/Morrey Total Elbow Surgical Technique Table of Contents Indications/Contraindications ................................................................................ 2 Preoperative Considerations ................................................................................... 3 Surgical Technique ................................................................................................... 4 Incision ............................................................................................................... 4 Humeral Resection ............................................................................................. 5 Preparation of the Ulna ....................................................................................... 7 Trial Reduction .................................................................................................... 9 Cement Technique .............................................................................................. 9 Humeral Bone Graft ......................................................................................... 10 Assembly and Impaction .................................................................................. 10 Closure ............................................................................................................. 11 Postoperative Management .................................................................................. 11 2 | Coonrad/Morrey Total Elbow Surgical Technique INDICATIONS & CONTRAINDICATIONS Indications include: post—traumatic -

Muscle Attachment Sites in the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Muscle Attachment Sites in the Upper Limb The Clavicle Pectoralis major Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: Right clavicle attachment of the deltoid Deltoid Axillary nerve Acromial facet Trapezius Sternocleidomastoid and Trapezius innervated by the Spinal Accessory nerve Sternocleidomastoid Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Conoid ligament Costoclavicular ligament Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Subclavian groove: Subclavius trapezoid ligament which binds the clavicle to site of attachment of the Innervated by Nerve to Subclavius which is the lateral part of the the first rib subclavius muscle coracoclavicular ligament Trapezoid ligament This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. The Scapula Trapezius Right scapula: posterior Levator scapulae Supraspinatus Deltoid Deltoid and Teres Minor are innervated by the Axillary nerve Rhomboid minor Levator Scapulae, Rhomboid minor and Rhomboid Major are innervated by the Dorsal Scapular Nerve Supraspinatus and Infraspinatus innervated by the Suprascapular nerve Infraspinatus Long head of triceps Rhomboid major Teres Minor Teres Major Teres Major -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -
Reference List for RMA425-2 As at 7 April 2020 Number
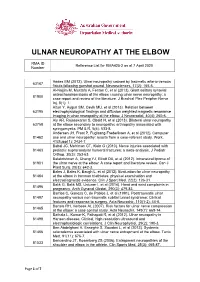
ULNAR NEUROPATHY AT THE ELBOW RMA ID Reference List for RMA425-2 as at 7 April 2020 Number Addas BM (2012). Ulnar neuropathy caused by traumatic arterio-venous 63167 fistula following gunshot wound. Neurosciences, 17(2): 165-6. Al-Najjim M, Mustafa A, Fenton C, et al (2013). Giant solitary synovial osteochondromatosis of the elbow causing ulnar nerve neuropathy: a 81900 case report and review of the literature. J Brachial Plex Peripher Nerve Inj, 8(1): 1. Altun Y, Aygun SM, Cevik MU, et al (2013). Relation between 63195 electrophysiological findings and diffusion weighted magnetic resonance imaging in ulnar neuropathy at the elbow. J Neuroradiol, 40(4): 260-6. Aly AR, Rajasekaran S, Obaid H, et al (2013). Bilateral ulnar neuropathy 63758 at the elbow secondary to neuropathic arthropathy associated with syringomyelia. PM & R, 5(6): 533-8. Andersen JH, Frost P, Fuglsang-Frederiksen A, et al (2012). Computer 81462 use and ulnar neuropathy: results from a case-referent study. Work, 41(Suppl 1): 2434-7. Babal JC, Mehlman CT, Klein G (2010). Nerve injuries associated with 81463 pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop, 30(3): 253-63. Balakrishnan A, Chang YJ, Elliott DA, et al (2012). Intraneural lipoma of 81901 the ulnar nerve at the elbow: A case report and literature review. Can J Plast Surg, 20(3): e42-3. Bales J, Bales K, Baugh L, et al (2012). Evaluation for ulnar neuropathy 81464 at the elbow in Ironman triathletes: physical examination and electrodiagnostic evidence. Clin J Sport Med, 22(2): 126-31. Balik G, Balik MS, Ustuner I, et al (2014). -

The Usefulness of Proximal Radial Motor Conduction in Acute Compressive Radial Neuropathy
JCN Open Access ORIGINAL ARTICLE pISSN 1738-6586 / eISSN 2005-5013 / J Clin Neurol 2015;11(2):178-182 / http://dx.doi.org/10.3988/jcn.2015.11.2.178 The Usefulness of Proximal Radial Motor Conduction in Acute Compressive Radial Neuropathy Kun Hyun Kima b Background and PurposezzThe objective of this study was to determine diagnostic and Kee-Duk Park a prognostic values of proximal radial motor conduction in acute compressive radial neuropathy. Pil-Wook Chung a MethodszzThirty-nine consecutive cases of acute compressive radial neuropathy with radial Heui-Soo Moon conduction studies–including stimulation at Erb’s point–performed within 14 days from a Yong Bum Kim clinical onset were reviewed. The radial conduction data of 39 control subjects were used as a Won Tae Yoon reference data. b Hyung Jun Park ResultszzThirty-one men and eight women (age, 45.2±12.7 years, mean±SD) were enrolled. Bum Chun Suha All 33 patients in whom clinical follow-up data were available experienced complete recov- ery, with a recovery time of 46.8±34.3 days. Partial conduction block was found frequently a Department of Neurology, Kangbuk Samsung Hospital, (17 patients) on radial conduction studies. The decrease in the compound muscle action po- Sungkyunkwan University tential area between the arm and Erb’s point was an independent predictor for recovery time. School of Medicine, Seoul, Korea zzProximal radial motor conduction appears to be a useful method for the early b Conclusions Department of Neurology, detection and prediction of prognosis of acute compressive radial neuropathy. Mokdong Hospital, Ewha Womans University Key Wordszz radial neuropathy, nerve conduction study, conduction block, diagnosis, School of Medicine, Seoul, Korea prognosis. -

Examination of the Shoulder Bruce S
Examination of the Shoulder Bruce S. Wolock, MD Towson Orthopaedic Associates 3 Joints, 1 Articulation 1. Sternoclavicular 2. Acromioclavicular 3. Glenohumeral 4. Scapulothoracic AC Separation Bony Landmarks 1. Suprasternal notch 2. Sternoclavicular joint 3. Coracoid 4. Acromioclavicular joint 5. Acromion 6. Greater tuberosity of the humerus 7. Bicipital groove 8. Scapular spine 9. Scapular borders-vertebral and lateral Sternoclavicular Dislocation Soft Tissues 1. Rotator Cuff 2. Subacromial bursa 3. Axilla 4. Muscles: a. Sternocleidomastoid b. Pectoralis major c. Biceps d. Deltoid Congenital Absence of Pectoralis Major Pectoralis Major Rupture Soft Tissues (con’t) e. Trapezius f. Rhomboid major and minor g. Latissimus dorsi h. Serratus anterior Range of Motion: Active and Passive 1. Abduction - 90 degrees 2. Adduction - 45 degrees 3. Extension - 45 degrees 4. Flexion - 180 degrees 5. Internal rotation – 90 degrees 6. External rotation – 45 degrees Muscle Testing 1. Flexion a. Primary - Anterior deltoid (axillary nerve, C5) - Coracobrachialis (musculocutaneous nerve, C5/6 b. Secondary - Pectoralis major - Biceps Biceps Rupture- Longhead Muscle Testing 2. Extension a. Primary - Latissimus dorsi (thoracodorsal nerve, C6/8) - Teres major (lower subscapular nerve, C5/6) - Posterior deltoid (axillary nerve, C5/6) b. Secondary - Teres minor - Triceps Abduction Primary a. Middle deltoid (axillary nerve, C5/6) b. Supraspinatus (suprascapular nerve, C5/6) Secondary a. Anterior and posterior deltoid b. Serratus anterior Deltoid Ruputure Axillary Nerve Palsy Adduction Primary a. Pectoralis major (medial and lateral pectoral nerves, C5-T1 b. Latissimus dorsi (thoracodorsal nerve, C6/8) Secondary a. Teres major b. Anterior deltoid External Rotation Primary a. Infraspinatus (suprascapular nerve, C5/6) b. Teres minor (axillary nerve, C5) Secondary a.